Abstract
Background
The stress hyperglycemia ratio (SHR), adjusted for average glycemic status, is suggested for assessing actual blood glucose levels. Its link with adverse outcomes is known in certain populations, yet its impact on sepsis patients’ prognosis is unclear. This study explores the association between SHR and mortality in sepsis.
Methods
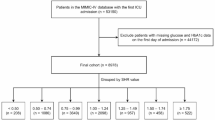
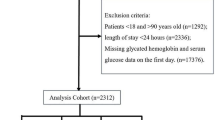
We included 13,199 sepsis patients in this study and categorized SHR into distinct groups. Additionally, we utilized restricted cubic spline analysis to evaluate the correlation between SHR as a continuous variable and mortality. The primary outcome was 1-year all-cause mortality. Logistic regression and Cox proportional hazards models were employed to assess the associations between the SHR and both in-hospital mortality and 1-year mortality, respectively.
Results
Among the study participants, 4,690 (35.5%) patients died during the 1-year follow-up. After adjusting for confounding variables, we identified a U-shaped correlation between SHR and 1-year mortality. Using an SHR of 0.99 as the reference point, the hazard ratio for predicted 1-year mortality increased by 1.17 (95% CI 1.08 to 1.27) per standard deviation above 0.99, whereas each standard deviation increase predicted the hazard ratio of 0.52 (95% CI 0.39 to 0.69) below 0.99. Furthermore, we found that SHR could enhance the predictive performance of conventional severity scores.
Conclusion
There exists a U shaped association between SHR and mortality in sepsis patients, where both low and high SHR values are associated with an increased risk of poor outcomes.




Similar content being viewed by others
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request.
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–10.
Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54.
Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, et al. Assessment of Global Incidence and Mortality of Hospital-treated. Sepsis Current Estimates and Limitations. Am J Respir Crit Care Med. 2016;193:259–72.
Xie J, Wang H, Kang Y, Zhou L, Liu Z, Qin B, et al. The Epidemiology of Sepsis in Chinese ICUs: A National Cross-Sectional Survey. Crit Care Med. 2020;48:e209–18.
Chiu C, Legrand M. Epidemiology of sepsis and septic shock. Curr Opin Anaesthesiol. 2021;34:71–6.
Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376:1339–46.
van Vught LA, Klein Klouwenberg PM, Spitoni C, Scicluna BP, Wiewel MA, Horn J, et al. Incidence, Risk Factors, and Attributable Mortality of Secondary Infections in the Intensive Care Unit After Admission for Sepsis. JAMA. 2016;315:1469–79.
Martin-Loeches I, Guia MC, Vallecoccia MS, Suarez D, Ibarz M, Irazabal M, et al. Risk factors for mortality in elderly and very elderly critically ill patients with sepsis: a prospective, observational, multicenter cohort study. Ann Intensive Care. 2019;9:26.
Pandolfi F, Brun-Buisson C, Guillemot D, Watier L. One-year hospital readmission for recurrent sepsis: associated risk factors and impact on 1-year mortality-a French nationwide study. Crit Care. 2022;26:371.
Marik PE, Bellomo R. Stress hyperglycemia: an essential survival response! Crit Care. 2013;17:305.
Zohar Y, Zilberman Itskovich S, Koren S, Zaidenstein R, Marchaim D, Koren R. The association of diabetes and hyperglycemia with sepsis outcomes: a population-based cohort analysis. Intern Emerg Med. 2021;16:719–28.
Lu Z, Tao G, Sun X, Zhang Y, Jiang M, Liu Y, et al. Association of Blood Glucose Level and Glycemic Variability With Mortality in Sepsis Patients During ICU Hospitalization. Front Public Health. 2022;10: 857368.
Roberts GW, Quinn SJ, Valentine N, Alhawassi T, O’Dea H, Stranks SN, et al. Relative Hyperglycemia, a Marker of Critical Illness: Introducing the Stress Hyperglycemia Ratio. J Clin Endocrinol Metab. 2015;100:4490–7.
Xu W, Song Q, Wang X, Zhao Z, Meng X, Xia C, et al. Association of stress hyperglycemia ratio and in-hospital mortality in patients with coronary artery disease: insights from a large cohort study. Cardiovasc Diabetol. 2022;21:217.
Cui K, Fu R, Yang J, Xu H, Yin D, Song W, et al. Stress hyperglycemia ratio and long-term mortality after acute myocardial infarction in patients with and without diabetes: A prospective, nationwide, and multicentre registry. Diabetes Metab Res Rev. 2022;38: e3562.
Li L, Ding L, Zheng L, Wu L, Hu Z, Liu L, et al. U-shaped association between stress hyperglycemia ratio and risk of all-cause mortality in cardiac ICU. Diabetes Metab Syndr. 2024;18: 102932.
Li L, Zhao M, Zhang Z, Zhou L, Zhang Z, Xiong Y, et al. Prognostic significance of the stress hyperglycemia ratio in critically ill patients. Cardiovasc Diabetol. 2023;22:275.
Gotts JE, Matthay MA. Sepsis: pathophysiology and clinical management. BMJ. 2016;353: i1585.
Marik PE, Raghavan M. Stress-hyperglycemia, insulin and immunomodulation in sepsis. Intensive Care Med. 2004;30:748–56.
Tiruvoipati R, Chiezey B, Lewis D, Ong K, Villanueva E, Haji K, et al. Stress hyperglycemia may not be harmful in critically ill patients with sepsis. J Crit Care. 2012;27:153–8.
Leonidou L, Michalaki M, Leonardou A, Polyzogopoulou E, Fouka K, Gerolymos M, et al. Stress-induced hyperglycemia in patients with severe sepsis: a compromising factor for survival. Am J Med Sci. 2008;336:467–71.
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a New Definition and Assessing New Clinical Criteria for Septic Shock: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:775–87.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4:30.
Zhou Q, Yang J, Wang W, Shao C, Hua X, Tang YD. The impact of the stress hyperglycemia ratio on mortality and rehospitalization rate in patients with acute decompensated heart failure and diabetes. Cardiovasc Diabetol. 2023;22:189.
Wei QC, Chen YW, Gao QY, Ren KD, Liu YB, He F, et al. Association of stress hyperglycemia with clinical outcomes in patients with ST-elevation myocardial infarction undergoing percutaneous coronary intervention: a cohort study. Cardiovasc Diabetol. 2023;22:85.
Fabbri A, Marchesini G, Benazzi B, Morelli A, Montesi D, Bini C, et al. Stress Hyperglycemia and Mortality in Subjects With Diabetes and Sepsis. Crit Care Explor. 2020;2: e0152.
Yang J, Zheng Y, Li C, Gao J, Meng X, Zhang K, et al. The Impact of the Stress Hyperglycemia Ratio on Short-term and Long-term Poor Prognosis in Patients With Acute Coronary Syndrome: Insight From a Large Cohort Study in Asia. Diabetes Care. 2022;45:947–56.
McNamara JJ, Mills D, Aaby GV. Effect of hypertonic glucose on hemorrhagic shock in rabbits. Ann Thorac Surg. 1970;9:116–21.
Losser MR, Damoisel C, Payen D. Bench-to-bedside review: Glucose and stress conditions in the intensive care unit. Crit Care. 2010;14:231.
Malfitano C, Alba Loureiro TC, Rodrigues B, Sirvente R, Salemi VM, Rabechi NB, et al. Hyperglycaemia protects the heart after myocardial infarction: aspects of programmed cell survival and cell death. Eur J Heart Fail. 2010;12:659–67.
Bahadoran Z, Mirmiran P, Ghasemi A. Role of Nitric Oxide in Insulin Secretion and Glucose Metabolism. Trends Endocrinol Metab. 2020;31:118–30.
Ling PR, Smith RJ, Bistrian BR. Hyperglycemia enhances the cytokine production and oxidative responses to a low but not high dose of endotoxin in rats. Crit Care Med. 2005;33:1084–9.
Stentz FB, Umpierrez GE, Cuervo R, Kitabchi AE. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises. Diabetes. 2004;53:2079–86.
Xu W, Zhao T, Xiao H. The Implication of Oxidative Stress and AMPK-Nrf2 Antioxidative Signaling in Pneumonia Pathogenesis. Front Endocrinol (Lausanne). 2020;11:400.
Acknowledgements
None.
Funding
This study was supported by the Medical and Health Technology Innovation Project of the Chinese Academy of Medical Sciences (2021-CXGC09-1).
Author information
Authors and Affiliations
Contributions
This study was designed by LL and LKZ. XP, ZXZ, LKZ, YLX, ZHZ, and ZH were responsible for data collation and statistical analysis. LL wrote the first draft. YY reviewed and checked the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, L., Zhou, L., Peng, X. et al. Association of stress hyperglycemia ratio and mortality in patients with sepsis: results from 13,199 patients. Infection (2024). https://doi.org/10.1007/s15010-024-02264-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02264-3