Abstract
Purpose
We aimed to evaluate the performance of the FilmArray (FA) meningitis/encephalitis (ME) panel. Secondarily, we analyzed the false positive (FP) and false negative (FN) results, as well as the predictive values of the technique, regarding the cerebrospinal fluid (CSF) characteristics.
Methods
FA is a multiplex real-time PCR detecting 14 of the most common ME pathogens in CSF. All FA performed at our hospital (2018–2022) were retrospectively reviewed. FA was compared to conventional techniques and its performance was assessed based on the final diagnosis of the episode.
Results
FA was performed in 313 patients with suspicion of ME. Most patients had altered mental status (65.2%) and fever (61%). Regarding CSF characteristics, 49.8% and 53.7% presented high CSF proteins and pleocytosis, respectively. There were 84 (26.8%) positive FA results, mainly for HSV-1 (10.9%), VZV (5.1%), Enterovirus (2.6%), and S. pneumoniae (1.9%). In the 136 cases where both FA and routine methods were performed, there was a 25.7% lack of agreement. We identified 6.6% FN results, but 28.6% FP, mainly due to HSV-1. This resulted in a high negative predictive value (NPV) of 93.4%, but a positive predictive value (PPV) of 73%. Remarkably, PPV as low as 36.9%, and 70.2%, were found in cases without pleocytosis, or lack of high CSF protein levels, respectively.
Conclusion
FA was associated with high NPV, but frequent FP results and low PPV, particularly for HSV-1, and especially in patients without high CSF protein levels or pleocytosis.
Similar content being viewed by others
Introduction
Acute meningoencephalitis (ME) is a life-threatening infection of the central nervous system (CNS) with a remaining high global incidence [1] and up to 19.9% risk of sequelae [2]. Early microbiological diagnosis is essential to guide correct antimicrobial treatment [3], and also to avoid the costs and toxicity of unnecessary treatments. However, conventional microbiological techniques to diagnose ME remain slow and frequently low-yielded [4].
In the last decade, multiplex real-time PCRs to detect the most common microorganisms associated with ME in a cerebrospinal fluid (CSF) sample have been developed for a rapid diagnosis. FilmArray® (FA) ME Panel (BioFire Diagnostics) is a multiplex real-time PCR that detects 14 of the most common bacterial, viral, and fungal causes of infectious ME, with a turnaround time of 3 h [5]. BioFire FA reports an overall sensitivity and specificity of 94.2% and 99.8%, respectively [6]. Nevertheless, a recent meta-analysis including 8 studies and 3059 patients, reported estimates of sensitivity of 90% (95% confidence interval [CI] 86–93%), and a specificity of 97% (95% CI 94–99%) [7]. A later meta-analysis reported a sensitivity of 92.1% (95% CI 86.8–95.3%) and a specificity of 99.2% (95% CI 98.3–99.6%) for bacterial meningitis, based on the analysis of 15 studies including 5524 patients, and considering a final diagnosis adjudication based on clinical/laboratory criteria [8]. In the same meta-analysis, sensitivity for Herpes simplex virus 1 (HSV-1) decreased to 78.2% (95% CI 58.1 − 90.3%) based on 3 studies including 6883 patients. Additionally, there was a concern for potential false positive (FP) and false negative (FN) results reported in real-life practice [7, 8].
We aimed to assess the FA performance since its introduction in the routine practice in our hospital to patients in whom ME was suspected. Secondarily, we analyzed the experienced FP and FN results, as well as the predictive values of the technique regarding the CSF characteristics.
Methods
Setting and data collection
This is a retrospective cohort study performed at the Hospital Clinic in Barcelona (Spain), an 800-bed university center that provides broad and specialized medical, surgical, and intensive care attention for an urban population of 500,000 people. Since 2018, our center has been performing FA testing when it was clinically indicated under the suspicion of ME.
Study population and design
We analyzed all consecutive cases of suspected ME in which FA was performed between January 2018 and February 2022. The following data were obtained for all patients: age and sex, pre-existing immunosuppression, clinical presentation, prior antibiotic therapy, CSF characteristics, intensive care unit (ICU) admission, and 30-day mortality. All data gathered were anonymously registered in a specific database designed for this study.
Definitions
Prior antibiotic therapy was defined as any antibiotics the patient had received in the last 24 h before obtaining a CSF sample. Prior corticosteroid use was defined as a minimum dose of 0.3 mg/kg/day of prednisone equivalent for > 3 weeks. Neutropenia was defined as an absolute neutrophil count of < 500 cells/mm3. Hypoglycorrhachia was defined as CSF glucose levels < 40 mg/dL. High protein CSF levels were > 600 mg/dL, high LDH levels were > 40 U/L, and high lactate levels were > 35 mg/dL. CSF pleocytosis was defined as > 10 leukocytes/mm3. The final diagnosis of the episode was determined by the investigators (N.L., G.C., and P.P-A.) after a thorough evaluation of microbiological and radiological results, clinical evolution, response to treatment, and the presence or absence of an alternative diagnosis.
Microbiological methods
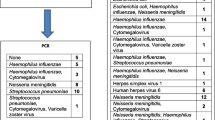
For the FA analysis, 200 µL of CSF was used. Samples were handled in a biosafety cabinet according to the manufacturer's instructions. BIOFIRE® FILMARRAY® Meningitis-Encephalitis (ME) Panel (BioFire Diagnostics, Salt Lake City, USA.) (FA) detects the following 14 potential ME pathogens in CSF: Escherichia coli K1, Haemophilus influenzae, Listeria monocytogenes, Neisseria meningitidis, Streptococcus agalactiae, Streptococcus pneumoniae, Enterovirus, HSV-1, Herpes simplex virus 2 (HSV-2), Human herpesvirus 6 (HHV-6), Human parechovirus, Varicella-zoster virus (VZV), Cytomegalovirus (CMV), and Cryptococcus neoformans/gattii.
The routine microbiology protocol for CSF samples with suspicion of ME includes inoculation of blood and chocolate agar, and thioglycolate broth, and Cryptococcus neoformans antigen (Remel™ Cryptococcus Antigen Test Kits; Thermo. Scientific, Lenexa, USA). Other complementary tests include detection in the CSF of traces of the pathogenic agent by 16S rRNA PCR and sequencing analysis (SensiFAST™ SYBR Hi-ROX kit; Meridian Bioscience, Inc., Cincinnati, OH, US., and sequences were identified using the Blast algorithm in the National Center for Biotechnology Information [NCBI] database), detection of S. pneumoniae antigen in CSF (BinaxNOW S. pneumoniae Antigen Card (BinaxNOW; Abbott, Chicago, USA), Neisseria meningitidis antigen (latex agglutination Wellcogen™ Neisseria meningitidis; Thermofisher, Waltham, USA), pathogen isolation in blood cultures (BACTEC™ FX; BD®; NYSE, USA), and detection of S. pneumoniae antigen in urine (BinaxNOW S. pneumoniae Antigen Card (BinaxNOW; Abbott, Chicago, USA). Conventional viral detections were performed by real-time PCR for HSV1/2, CMV, HHV-6, VZV (Nanogen Advanced Diagnostics; Palex®, Barcelona, Spain), and Enterovirus (OneStep RT-PCR Kit; QIAGEN®, Hilden, Germany). FA was performed in all cases, but conventional tests were not always available due to insufficient sample volume. Complementary tests were performed, whenever feasible, based on physicians’ discretion. Results obtained were used to support other clinical, laboratory, and radiological findings to get the final diagnosis.
Statistical analysis
Categorical variables were described as counts and percentages, whereas continuous variables were expressed as means and standard deviations (SD) or medians and interquartile ranges (IQRs). All analyses were performed with SPSS software (version 25.0; SPSS, Inc., Chicago, IL). The sensitivity, specificity, and predictive values of the technique were based on the final diagnosis of the episode, as determined by the investigators.
Ethics approval
This observational study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee Board of the Hospital Clinic of Barcelona (HCB/2022/0943). To protect personal privacy of patients, identifiable information in the database was encrypted for each patient. Informed consent was waived, as no intervention was involved, and no patient-identifiable information was included.
Results
Cohort characteristics, clinical presentation, outcomes, and CSF characteristics
During the study period, FA multiplex real-time PCR was performed in 313 patients with suspicion of ME. Table 1 shows the cohort characteristics and clinical presentation of the episodes. Overall, 123 (39.3%) patients had some known immunosuppression and 18 (5.8%) patients had neutropenia. Most patients presented with altered mental status (65.2%) and fever (61%), while only 38 (12.1%) had neck stiffness. ICU admission was required in 135 (43.1%) patients, and 30-day mortality was 11.8%.
Table 2 detailed the characteristics of the analyzed CSF. Overall, 154 (49.8%) patients presented high proteins in CSF, and 168 (53.7%) had pleocytosis. Conversely, hypoglycorrhachia was present in only 33 (10.6%) patients.
A final diagnosis of ME was made in 79 (25.2%) patients. In such cases, 65.8% patients had high proteins in CSF, 89.9% had pleocytosis, and 21.5% had hypoglycorrhachia.
FA results and comparison to routine methods
Out of the 313 FA tests performed, 84 (26.8%) were positive. Table 3 shows the positive FA results. HSV-1 was the most diagnosed pathogen (10.9%), followed by VZV (5.1%), and enterovirus (2.6%). Most diagnosed bacteria were S. pneumoniae (1.9%), L. monocytogenes (1.3%), and S. agalactiae (1.3%). There were 5 cases with positive polymicrobial results.
There were 136 (43.5%) cases in which both FA and routine methods were performed and a positive result was obtained. In 35 (25.7%) of such cases, there was a lack of agreement between FA and routine methods. There were 13 cases in which the FA yielded a positive bacterial result, but the cultures were negative (3 S. pneumoniae, 2 S. agalactiae, 2 L. monocytogenes, 2 N. meningitidis, 1 E. coli, 1 H. influenzae, and 2 positives for both S. pneumoniae and H. influenzae). On the other hand, there were 7 cases with a negative FA result, in which the culture was positive for bacterial isolates not included in the multiplex PCR (3 Mycobacterium tuberculosis, 2 Enterococcus faecium, 1 Klebsiella pneumoniae, and 1 Staphylococcus epidermidis). There were also 12 cases in which the FA yielded a positive viral result, but routine PCRs were negative (9 HSV-1, 1 CMV, 1 HHV-6, and 1 positive for both HSV-1 and HSV-2). Finally, there were 5 cases where FA was negative, but routine PCRs were positive for a viral infection (all for HSV-1).
FA performance for the diagnosis of ME
After clinical assessment, of the 229 negative FA results, 214 (93.4%) were considered true negatives, while 15 (6.6%) were considered FN. Most (10 out of 15) of the considered FN cases presented with ME caused by microorganisms not included in the multiplex PCR panel.
Of the 84 positive FA results, 64 (76.2%) were considered true positives, while 24 (28.6%) were considered FP. There were 4 polymicrobial results, in which both true and FP results were obtained. In this sense, all five cases in which the FA yielded a positive polymicrobial result, some or all the results were considered to be a FP. FP results were mainly attributed to HSV-1 (n = 17), followed by H. influenzae (n = 3), S. pneumoniae (n = 2), HHV-6 (n = 2), CMV (n = 1), enterovirus (n = 1), HSV-2 (n = 1), VZV (n = 1), E. coli (n = 1), and C. neoformans/gattii (n = 1). Table 4 details all FP cases and their final diagnosis.
Considering a 25.2% of infection prevalence in this cohort, the sensitivity and specificity of FA were 81.0% (95% CI, 70.6%-89.0%) and 89.9% (85.4%-93.4%), respectively. The positive predictive value (PPV) was 73.0% (64.6%-80.1%) and the negative predictive value (NPV) was 93.4% (89.9%-95.7%). After excluding those pathogens not included in the multiplex PCR panel, NPV increased to 97.41% (94.4%-99.1%).
Episodes without CSF pleocytosis and/or high CSF protein levels
There were 145, and 155 cases in which FA was performed despite the lack of pleocytosis, or high CSF protein levels, respectively. Of those cases without pleocytosis, or high CSF protein levels, 8 (5.5%), and 26 (16.8%), respectively, were finally considered to have presented a viral meningoencephalitis. No bacterial infection was diagnosed without pleocytosis. Only one N. meningitidis meningitis was diagnosed without high CSF protein levels.
Table 5 shows sensitivities, specificities, and predictive values of FA regarding CSF characteristics. Remarkably, PPVs as low as 36.9%, and 70.2%, were found in cases with a lack of pleocytosis, or lack of high CSF protein levels, respectively.
Discussion
The current study describes a large cohort of patients in whom a ME was suspected and the multiplex real-time PCR FilmArray® (FA) ME Panel (BioFire Diagnostics) was performed to identify the etiology. We aimed to evaluate FA performance and its concordance with routine microbiological methods. The most important findings were: (1) FA was frequently performed in patients without high CSF protein levels or pleocytosis; (2) in this setting, over a quarter of patients presented a positive result, mostly due to viral pathogens; (3) in those cases in which both FA and routine methods were performed, there was a substantial lack of concordance (25.7% of cases); (4) FA was associated to a low rate of FN results, but a considerable rate of FP were found, resulting in excellent specificity and NPV, with moderate sensitivity and PPV; (5) in those cases without pleocytosis, or high CSF protein levels, PPV was substantially lower (Table 5).
In our cohort, FA was performed in patients with clinical suspicion of ME, but in which CSF characteristics were frequently only mildly altered. In this context of potential low pre-test probability of ME, a positive FA result was found in 26.8% of the patients, mostly due to viral pathogens. Prior studies regarding patients with suspected ME reported slightly higher numbers of proteins and leukocytes in the CSF samples, but the rates of positivity were similar, ranging from 8 to 25% [5, 9,10,11,12]. Similar to our study, most positive FA results were viral pathogens, mainly HSV-1, enterovirus, and VZV, although this varied widely, especially regarding some studies including children. As expected, the most common bacterial pathogen in our cohort and other studies was S. pneumoniae.
In our cases, when both routine methods and FA were performed, concordance rates were relatively low (74.3%). These findings contrast with previous studies where overall agreement between techniques was found in over 80–90% of cases [11, 13,14,15]. The lack of concordance in our study was mainly due to positive FA results with negative routine tests. Regarding bacterial pathogens, this could be explained by the high rates of antibiotic use before lumbar puncture (38% in the whole cohort), potentially causing a negative culture [16, 17]. In this sense, half of patients with positive FA and a negative CSF culture had received antibiotic prior to CSF analysis. Regarding viral pathogens, there were mainly positive FA results that were finally negative in routine methods, but also negative FA results with positive routine PCRs. The potential explanation for this lack of agreement for viral pathogens is unclear since both methods are real-time PCRs, although they use different primers/probes and are run on different platforms. One potential limitation of FA is that is a closed, qualitative technique, in which only the melting curve is available, but amplification curves or cycle thresholds are not available. This information could be helpful to interpret discordant or uncertain cases.
After the final clinical and microbiological evaluation of the episode, the performance of the FA was overall good. Like previous reports [7, 8], high specificity and NPV (89.9% and 93.4%, respectively) were obtained. Moreover, many of the few false negative results were ME cases caused by pathogens not included in the multiplex PCR panel, which is an expected limitation of the technique. On the other hand, the rates of FPs were high (25.8%) resulting in a relatively low PPV (73%). This is somehow higher to other studies with FA, reporting FP rates around 10–30% compared to reference tests combined with clinical and analytical data [8, 10,11,12]. False positive results by bacterial targets such as H. influenzae and S. pneumoniae (which accounted for most bacterial FP results in our cohort) could be explained by potential specimen contaminations at the time of collection or processing by colonized professionals. However, most FP results in our cohort were due to HSV-1, which contrasts with most studies reporting bacterial pathogens as the most frequent cause of FP [7, 8, 10]. In fact, half of the positive FA results for HSV-1 were considered FPs, with previous studies reporting rates of FP HSV-1 ranging from 5 to 50% among positive cases, but with significantly lower cases [7, 10,11,12]. One potential hypothesis would be that positive HSV-1 from the blood instead of CSF is being detected due to hematic contamination of the sample [8, 11]. Interestingly, out of the 24 FP results, only 3 had no red cells in the sample, and 12 of them had more than 100 red cells/mm3. Unfortunately, none of these FP cases had a blood HSV-1 viral load performed at a time close to the lumbar puncture. Another explanation would be that all positive FA results were assessed and prospectively followed by an Infectious Diseases specialist, potentially allowing for antiviral stopping and FP detection whenever the other tests and clinical picture were not suggestive of herpes encephalitis. Finally, the low PPV in our study was mainly driven by the high rates of only mildly or not altered CSF characteristics, which is known to decrease the FA performance [5, 8], particularly when the pre-test probability of ME is low. In this sense, PPV in those patients with either lack of pleocytosis, or normal CSF proteins, was remarkably low. This is challenging since many patients presenting with ME suspicion will actually have these only mildly altered CSF characteristics. This is especially important in severely immunosuppressed patients with profound neutropenia, as they may develop CNS infections without pleocytosis. In such a context, FA could still be useful due to its high NPV [18, 19], but confirmation of positive results (with routine methods, radiology, etc.) is imperative.
The strength of this study is that it thoroughly analyzes all clinical cases to evaluate the performance of FA in a real-life setting. However, this study has some limitations that should be acknowledged. First, this is a single-center study reporting a moderate number of cases over four years. Second, routine analysis of all samples was not available due to insufficient sample volume. Third, complementary tests were not performed systematically but based on the physicians' discretion. Finally, as already exposed, FA performance was limited by the fact that it was frequently performed in patients with normal or slightly altered CSF characteristics.
In conclusion, FA is a useful technique in cases of suspected ME, providing fast results with high NPV. This could be helpful to rule out ME and avoid unnecessary treatments. However, FP results are frequent, especially in patients without high CSF protein levels or pleocytosis.
Data availability
Data would be available from the corresponding author under reasonable request.
References
Meningitis—Level 3 cause | Institute for Health Metrics and Evaluation. https://www.healthdata.org/results/gbd_summaries/2019/meningitis-level-3-cause. Retrieved 6 March 2023.
Edmond K, Clark A, Korczak VS, Sanderson C, Griffiths UK, Rudan I. Global and regional risk of disabling sequelae from bacterial meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:317–28.
Dorsett M, Liang SY. Diagnosis and treatment of central nervous system infections in the emergency department. Emerg Med Clin North Am. 2016;34:917–42.
Brouwer MC, Tunkel AR, Van De Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin Microbiol Rev. 2010;23:467–92.
Cailleaux M, Pilmis B, Mizrahi A, Lourtet-Hascoet J, Van JCN, Alix L, Couzigou C, Vidal B, Tattevin P, Le Monnier A. Impact of a multiplex PCR assay (FilmArray®) on the management of patients with suspected central nervous system infections. Eur J Clin Microbiol Infect Dis. 2020;39:293–7.
Biofire Diagnostics. 2020. BioFire FilmArray Meningitis/Encephalitis Panel (ME) | BioFire Diagnostics. https://www.biofiredx.com/products/the-filmarray-panels/filmarrayme/. Retrieved 6 March 2023.
Tansarli GS, Chapin KC. Diagnostic test accuracy of the BioFire® FilmArray® meningitis/encephalitis panel: a systematic review and meta-analysis. Clin Microbiol Infect. 2020;26:281–90.
Trujillo-G Omez J, Tsokani S, Arango-Ferreira C, Atehort Ua-Mu~ S, Jos E Jimenez-Villegas M, Serrano-Tabares C, Veroniki A-A, Florez ID. Biofire FilmArray Meningitis/Encephalitis panel for the aetiological diagnosis of central nervous system infections: A systematic review and diagnostic test accuracy meta-analysis. eClinicalMedicine. 2022;44:101275.
Moffa MA, Bremmer DN, Carr D, Buchanan C, Shively NR, Elrufay R, Walsh TL. Impact of a multiplex polymerase chain reaction assay on the clinical management of adults undergoing a lumbar puncture for suspected community-onset central nervous system infections. Antibiotics. 2020;9:282.
Vincent JJ, Zandotti C, Baron S, Kandil C, Levy PY, Drancourt M, Raoult D, Ninove L. Point-of-care multiplexed diagnosis of meningitis using the FilmArray® ME panel technology. Eur J Clin Microbiol Infect Dis. 2020;39:1573–80.
Leber AL, Everhart K, Balada-Llasat JM, Cullison J, Daly J, Holt S, Lephart P, Salimnia H, Schreckenberger PC, DesJarlais S, Reed SL, Chapin KC, LeBlanc L, Johnson JK, Soliven NL, Carroll KC, Miller JA, Bard JD, Mestas J, Bankowski M, Enomoto T, Hemmert AC, Bourzac KM. Multicenter evaluation of biofire filmarray meningitis/encephalitis panel for detection of bacteria, viruses, and yeast in cerebrospinal fluid specimens. J Clin Microbiol. 2016;54:2251–61.
Lindström J, Elfving K, Lindh M, Westin J, Studahl M. Assessment of the FilmArray ME panel in 4199 consecutively tested cerebrospinal fluid samples. Clin Microbiol Infect. 2022;28:79–84.
Hanson KE, Slechta ES, Killpack JA, Heyrend C, Lunt T, Daly JA, Hemmert AC, Blaschke AJ. preclinical assessment of a fully automated multiplex PCR panel for detection of central nervous system pathogens. J Clin Microbiol. 2016;54:785–7.
Liesman RM, Strasburg AP, Heitman AK, Theel ES, Patel R, Binnicker MJ. Evaluation of a commercial multiplex molecular panel for diagnosis of infectious meningitis and encephalitis. J Clin Microbiol. 2018;56:e01927-e2017.
Radmard S, Reid S, Ciryam P, Boubour A, Ho N, Zucker J, Sayre D, Greendyke WG, Miko BA, Pereira MR, Whittier S, Green DA, Thakur KT. Clinical utilization of the filmarray meningitis/encephalitis (ME) multiplex polymerase chain reaction (PCR) assay. Front Neurol. 2019;10:281.
Bronska E, Kalmusova J, Dzupova O, Maresova V, Kriz P, Benes J. Dynamics of PCR-based diagnosis in patients with invasive meningococcal disease. Clin Microbiol Infect. 2006;12:137–41.
Seth R, Murthy PSR, Sistla S, Subramanian M, Tamilarasu K. Rapid and accurate diagnosis of acute pyogenic meningitis due to Streptococcus pneumoniae, Haemophilus influenzae type b and Neisseria meningitidis using a multiplex PCR assay. J Clin Diagnostic Res. 2017;11:FC01–FC04.
Markovich K, Wingler MJB, Stover KR, Barber KE, Wagner JL, Cretella DA. Analysis of the clinical impact of the BioFire FilmArray meningitis encephalitis panel on antimicrobial use and duration of therapy at an academic medical center. Diseases. 2022;10:110.
DiDIodato G, Bradbury N. Cerebrospinal fluid analysis with the biofire filmarray meningitis/ encephalitis molecular panel reduces length of hospital stay in patients with suspected central nervous system infections. Open Forum Infect Dis. 2019;6:ofz119.
Acknowledgements
We would like to thank Anna Vilalta Vidal and Sergi Anguera for their help in collecting data.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. P.P.-A. (JR20/00012, PI21/00498, and ICI21/00103) and C.G.-V. (FIS PI21/01640 and ICI21/00103) have received research grants funded by Instituto de Salud Carlos III (ISCIII) and co-funded by the European Union. The funders had neither a specific role in study design or collection of data, nor in writing of the paper or decision to submit.
Author information
Authors and Affiliations
Contributions
Conceptualization: PP-A; methodology: GC, AS, PP-A; software: GC, PP-A; formal analysis: PP-A; investigation: all authors; resources: all authors; data curation: all authors; writing—original draft: NL, GC, PP-A; writing—review and editing: all authors; visualization: all authors; supervision: AS, PP-A; project administration: PP-A.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
CG-V has received honoraria for talks on behalf of Gilead Science, Merck Sharp and Dohme, Pfizer, Jannsen, Novartis, Lilly and a grant support from Gilead Science and Merck Sharp and Dohme. AS has received honoraria for lectures and advisory boards from Pfizer, Merck Sharp and Dohme, Shionogi, Angelini, Menarini, and Gilead Sciences. AS has received grants from Pfizer and Gilead Sciences. P.P.-A. has received honoraria for talks on behalf of Merck Sharp and Dohme, Lilly, ViiV Healthcare and Gilead Science. P.P.-A. has participated in advisory boards for Gilead Science.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
López, N., Cuesta, G., Rodríguez-Vega, S. et al. Multiplex real-time PCR FilmArray performance in the diagnosis of meningoencephalitis: lights and shadows. Infection 52, 165–172 (2024). https://doi.org/10.1007/s15010-023-02076-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-023-02076-x