Abstract
Purpose
Data on encephalitis in elderly patients are scarce. We aimed to describe the characteristics, aetiologies, management, and outcome of encephalitis in patients older than 65 years.
Methods
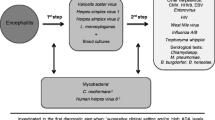
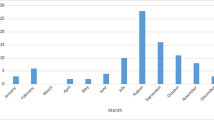
We performed an ancillary study of ENCEIF, a prospective cohort that enrolled all cases of encephalitis managed in 46 clinical sites in France during years 2016–2019. Cases were categorized in three age groups: (1) 18–64; (2) 65–79; (3) ≥ 80 years.
Results
Of the 494 adults with encephalitis enrolled, 258 (52%) were ≥ 65 years, including 74 (15%) ≥ 80 years. Patients ≥ 65 years were more likely to present with coma, impaired consciousness, confusion, aphasia, and rash, but less likely to present with fever, and headache (P < 0.05 for each). Median cerebrospinal fluid (CSF) white cells count was 61/mm3[13–220] in 65–79 years, 62 [17–180] in ≥ 80 years, vs. 114 [34–302] in < 65 years (P = 0.01). The proportion of cases due to Listeria monocytogenes and VZV increased after 65 years (P < 0.001), while the proportion of tick-borne encephalitis and Mycobacterium tuberculosis decreased with age (P < 0.05 for each). In-hospital mortality was 6/234 (3%) in < 65 years, 18/183 (10%) in 65–79 years, and 13/73 (18%) in ≥ 80 years (P < 0.001). Age ≥ 80 years, coma on admission, CSF protein ≥ 0.8 g/L and viral encephalitis were independently predictive of 6 month mortality.
Conclusion
Elderly patients represent > 50% of adults with encephalitis in France, with higher proportion of L. monocytogenes and VZV encephalitis, increased risk of death, and sequels. The empirical treatment currently recommended, aciclovir and amoxicillin, is appropriate for this age group.

Similar content being viewed by others
Data availability
Data may be available on request.
References
Stahl JP, Azouvi P, Bruneel F, et al. Guidelines on the management of infectious encephalitis in adults. Médecine Mal Infect. 2017;47:179–94.
Venkatesan A, Tunkel AR, Bloch KC, et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: consensus statement of the international encephalitis consortium. Clin Infect Dis. 2013;57:1114–28.
Granerod J, Ambrose HE, Davies NW, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10:835–44.
George BP, Schneider EB, Venkatesan A. Encephalitis hospitalization rates and inpatient mortality in the United States, 2000–2010. PLoS ONE. 2014;9: e104169.
Singh TD, Fugate JE, Rabinstein AA. The spectrum of acute encephalitis: causes, management, and predictors of outcome. Neurology. 2015;84:359–66.
Glaser CA, Honarmand S, Anderson LJ, et al. Beyond viruses: clinical profiles and etiologies associated with encephalitis. Clin Infect Dis. 2006;43:1565–77.
Bodilsen J, Storgaard M, Larsen L, et al. Infectious meningitis and encephalitis in adults in Denmark: a prospective nationwide observational cohort study (DASGIB). Clin Microbiol Infect. 2018;24:1102.e1-1102.e5.
Mailles A, Stahl J. Infectious encephalitis in France in 2007: a national prospective study. Clin Infect Dis. 2009;49:1838–47.
Granerod J, Tam CC, Crowcroft NS, Davies NWS, Borchert M, Thomas SL. Challenge of the unknown: a systematic review of acute encephalitis in non-outbreak situations. Neurology. 2010;75:924–32.
Davison KL, Crowcroft NS, Ramsay ME, Brown DWG, Andrews NJ. Viral encephalitis in England, 1989–1998: what did we miss? Emerg Infect Dis. 2003;9:234–40.
Quist-Paulsen E, Kran A-MB, Dunlop O, Wilson J, Ormaasen V. Infectious encephalitis: a description of a Norwegian cohort. Scand J Infect Dis. 2013;45:179–85.
Mailles A, De Broucker T, Costanzo P, et al. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 2012;54:1455–64.
Tunkel AR, Glaser CA, Bloch KC, et al. The management of encephalitis: clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis. 2008;47:303–27.
Schlitt M, Lakeman FD, Whitley RJ. Psychosis and herpes simplex encephalitis. South Med J. 1985;78(11):1347–50.
Solomon T, Hart IJ, Beeching NJ. Viral encephalitis: a clinician’s guide. Pract Neurol. 2007;7:288–305.
Gavazzi G, Krause K-H. Ageing and infection. Lancet Infect Dis. 2002;2:659–66.
Yoshikawa TT, Norman DC. Geriatric infectious diseases: current concepts on diagnosis and management. J Am Geriatr Soc. 2017;65:631–41.
Hansen MA, Samannodi MS, Castelblanco RL, Hasbun R. Clinical epidemiology, risk factors, and outcomes of encephalitis in older adults. Clin Infect Dis. 2020;70:2377–85.
Mailles A, Argemi X, Biron C, et al. Changing profile of encephalitis: results of a 4-year study in France. Infect Dis Now. 2022;52:1–6.
Jennett B. Assessment of outcome after severe brain damage. The Lancet. 1975;305:480–4.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJA, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Logar M, Bogovič P, Cerar D, Avšič-Županc T, Strle F. Tick-borne encephalitis in Slovenia from 2000 to 2004: comparison of the course in adult and elderly patients. Wien Klin Wochenschr. 2006;118:702–7.
Hebant B, Miret N, Bouwyn JP, Delafosse E, Lefaucheur R. Absence of pleocytosis in cerebrospinal fluid does not exclude herpes simplex virus encephalitis in elderly adults. J Am Geriatr Soc. 2015;63:1278–9.
Schoonman GG, Rath JJG, Buren M, Melief PHGJ, Wirtz PW. Herpes simplex virus encephalitis without cerebrospinal fluid pleocytosis is not unusual. J Am Geriatr Soc. 2012;60:377–8.
Raschilas F, Wolff M, Delatour F, et al. Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis. 2002;35:254–60.
Vora NM, Holman RC, Mehal JM, Steiner CA, Blanton J, et al. Burden of encephalitis-associated hospitalizations in the United States, 1998–2010. Neurology. 2014;82:443–51.
Campbell GL, Marfin AA, Lanciotti RS, Gubler DJ. West Nile virus. Lancet Infect Dis. 2002;2:519–29.
Hjalmarsson A, Blomqvist P, Skoldenberg B. Herpes simplex encephalitis in Sweden, 1990–2001: incidence, morbidity, and mortality. Clin Infect Dis. 2007;45:875–80.
Miller RA. The aging immune system: primer and prospectus. Science. 1996;273:70–4.
Velay A, Solis M, Kack-Kack W, et al. A new hot spot for tick-borne encephalitis (TBE): a marked increase of TBE cases in France in 2016. Ticks Tick-Borne Dis. 2018;9:120–5.
Office fédéral de la santé publique. Encéphalite à tique: extension des zones à risque où la vaccination est recommandée. https://www.bag.admin.ch/bag/fr/home/das-bag/aktuell/news/news-04-02-2019.html. Accessed 24 Apr 2021.
Haut Comité de Santé Publique. Avis relatif à l’inscription de l’encéphalite à tiques sur la liste des maladies à déclaration obligatoire Available at: https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=856. Accessed 24 Apr 2021.
Sili U, Tavsanli ME, Tufan A. Herpes simplex virus encephalitis in geriatric patients. Curr Geriatr Rep. 2017;6:34–41.
Sheybani F, Naderi H, Sajjadi S. The optimal management of acute febrile encephalopathy in the aged patient: a systematic review. Interdiscip Perspect Infect Dis. 2016;2016:1–13.
Acknowledgements
The authors would like to thank the investigators’ group and the scientific committee of ENCEIF.
Sophie Abgrall, Laurent Argaud, Xavier Argemi, Nathalie Asseray, Guillaume Baille, Aurélie Baldolli, Julien Biberon, Charlotte Biron, Geneviève Blanchet-Fourcade, Mathieu Blot, Anne Bonnetain, Elisabeth Botelho-Nevers, Frédéric Bourdain, David Boutoille, Hélène Brasme, Cédric Bruel, Fabrice Bruneel, Rodolphe Buzele, Etienne Canouï, Philippe Casenave, Bernard Castan, Charles Cazanave, Céline Cazorla, Thibault Challan-Belval, Pascal Chavanet, Catherine Chirouze, Tomasz Chroboczek, Johan Courjon, Thomas De Broucker, Arnaud De La Blanchardière, Etienne de Montmollin, Thècle Degroote, Marine Delaroche, Eric Denes, Colin Deschanvres, Capucine Diard-Detoeuf, Aurélien Dinh, Olivier Epaulard, Pierre Fillatre, Emmanuel Forestier, Thibault Fraisse, Marie Froidure, Benjamin Gaborit, Amandine Gagneux-Brunon, Nicolas Gaillard, Arnaud Galbois, Mathieu Godement, François Goehringer, Simon Gravier, Valentin Greigert, Isabelle Gueit, Thomas Guimard, Carole Henry, Maxime Hentzien, Jean-Etienne Herbrecht, Pierre Jaquet, Fanny Jommier, Lydie Katchatourian, Solene Kerneis, Jessica Krause, Manuela Le Cam, Marion Le Maréchal, Gwenael Le Moal, Paul Le Turnier, Raphael Lecomte, Anne-Sophie Lecompte, Romain Lefaucheur, Stéphanie Lejeune, Xavier Lescure, Olivier Lesieur, Philippe Lesprit, Guillaume Louis, Christelle Lucas, Rafael Mahieu, Alain Makinson, Guillaune Marc, Alexandre Maria, Nathalie Marin, Aurélie Martin, Guillaume Martin-Blondel, Martin Martinot, Alexandre Mas, Philippe Mateu, Morgan Matt, Laurence Maulin, Frédéric Mechai, Jean-Paul Mira, Eugénie Mutez, Jérémie Orain, Anne Schieber-Pachart, Nathalie Pansu, Solene Patrat-Delon, Patricia Pavese, Hélène Pelerin, Véronique Pelonde-Erimée, Isabelle Pierre, Diane Ponscarme, Dimitri Psimaras, Mathilde Puges, Mathilde Reveillon-Istin, Sylvain Rheims, Aurélie Richard-Mornas, Agnès Riché, Vincent Roubeau, Yvon Ruch, Isabelle Runge, Hélène Savini, Romain Sonneville, Jean-Paul Stahl, Pierre Tattevin, Kelly Tiercelet, Saber Touati, Jean-Marie Turmel, Isabelle Tyvaert, Marc-Olivier Vareil, Magalie Vidal-Roux, Virginie Vitrat, Heidi Wille, Mathieu Zuber, Laurent Almoyna-Martinez, Olivier Bouchaud, Thomas de Broucker, Fabrice Bruneel, Bernard Castan, Eric Denes, Olivier Epaulard, Nadine Girard, Jean-Louis Herrmann, Jérome Honnorat, Alexandra Mailles, Patrice Morand, François Raffi, France Roblot, Jean-Paul Stahl, Romain Sonneville, Pierre Tattevin
Funding
French Infectious Diseases Society (Société de pathologie infectieuse de langue française, SPILF).
Author information
Authors and Affiliations
Consortia
Contributions
AM and JPS: planned and designed the ENCEIF study, obtained funding, and coordinated patients enrolment. AM, PF and PP: performed primary analysis. PT: contributed to the analysis and wrote the first draft of the manuscript. All authors contributed to the final version and approved the revised manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Patients or their close relatives received oral and written information about the study, and could refuse to be enrolled, but no written consent was required according to the French regulations for observational studies. This study was authorized by French Commission for Data Protection, the “Commission Nationale Informatique et Liberté” (CNIL, DR-2015-300) and was approved by the Advisory Committee on Research Information Processing, the “Comité Consultatif sur le Traitement de l'Information en matière de Recherche dans le domaine de la Santé” (CCTIRS).
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Petitgas, P., Tattevin, P., Mailles, A. et al. Infectious encephalitis in elderly patients: a prospective multicentre observational study in France 2016–2019. Infection 51, 859–867 (2023). https://doi.org/10.1007/s15010-022-01927-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01927-3