Abstract
Purpose
Multidrug-resistant Gram-negative bacteria (MDR-GNB) have become a major global public health threat. Ceftazidime–avibactam (CAZ–AVI) is a newer combination of β-lactam/β-lactamase inhibitor, with activity against carbapenem-resistant Enterobacterales (CRE) and carbapenem-resistant Pseudomonas aeruginosa (CRPA). The aim of this review is to describe the recent real-world experience of CAZ–AVI for the infections due to MDR-GNB.
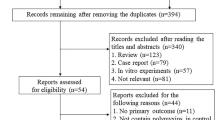
Methods
We searched PubMed, Embase and Google Scholar for clinical application in CAZ-AVI for MDR-GNB infections. Reference lists were reviewed and synthesized for narrative review.
Results
MDRGNB infections are associated with higher mortality significantly comparing to drug-susceptible bacterial infections. Fortunately, CAZ–AVI shows significant benefits for infections due to KPC or OXA-48 CRE, comparing to colistin, carbapenem, aminoglycoside and other older agents, even in those with immunocompromised status. The efficacy of CAZ–AVI varies in different infection sites due to CRE, which is lower in pneumonia. Early use is associated with improved clinical outcomes. Noteworthy, when adopted as salvage therapy, CAZ–AVI is still superior to other GNB active antibiotics. CAZ–AVI plus aztreonam is recommended as the first line of MBL-CRE infections. However, for infections caused by KPC- and OXA-48-producing isolates, further investigations are needed to demonstrate the benefit of combination therapy. Besides CRE, CAZ-AVI is also active to MDR-PA. However, the development of resistance in CRE and MDR-PA against CAZ–AVI is alarming, and more investigations and studies are needed to prevent, diagnose, and treat infections due to CAZ–AVI-resistant pathogens.
Conclusions
CAZ-AVI appears to be a valuable therapeutic option in MDR-GNB infections. Using CAZ-AVI appropriately to improve efficacy and decrease the emergence of resistance is important.
Similar content being viewed by others
References
Doi Y, Iovleva A, Bonomo R. The ecology of extended-spectrum β-lactamases (ESBLs) in the developed world. J Travel Med. 2017;24:S44-S51. https://doi.org/10.1093/jtm/taw102.
Grundmann H, Glasner C, Albiger B, Aanensen D, Tomlinson C, Andrasević A, et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): a prospective, multinational study. Lancet Infect Dis. 2017;17:153–63. https://doi.org/10.1016/s1473-3099(16)30257-2.
Shortridge D, Gales A, Streit J, Huband M, Tsakris A, Jones R. Pseudomonas aeruginosageographic and temporal patterns of antimicrobial resistance in over 20 years from the SENTRY antimicrobial surveillance program, 1997–2016. Open Forum Infect Dis. 2019;6:S63–8. https://doi.org/10.1093/ofid/ofy343.
Eichenberger E, Thaden J. Epidemiology and Mechanisms of Resistance of Extensively Drug Resistant Gram-Negative Bacteria. Antibiotics (Basel, Switzerland). 2019;8(2). https://doi.org/10.3390/antibiotics8020037.
Weiner L, Webb A, Limbago B, Dudeck M, Patel J, Kallen A, et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the national healthcare safety network at the centers for disease control and prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37:1288–301. https://doi.org/10.1017/ice.2016.174.
https://www.ecdc.europa.eu/sites/portal/files/documents/EARS-Net-report-2017-update-jan-2019.pdf.
Centers for Disease Control and Prevention (CDC). Antimicrobial Resistance. Atlanta: CDC; 2015. http://www.cdc.gov/drugresistance/index.html. https://doi.org/10.3389/fmed.2019.00074.
Vardakas K, Matthaiou D, Falagas M, Antypa E, Koteli A, Antoniadou E. Characteristics, risk factors and outcomes of carbapenem-resistant Klebsiella pneumoniae infections in the intensive care unit. J Infect. 2015;70:592–9. https://doi.org/10.1016/j.jinf.2014.11.003.
Villegas M, Pallares C, Escandón-Vargas K, Hernández-Gómez C, Correa A, Álvarez C, et al. Characterization and clinical impact of bloodstream infection caused by carbapenemase-producing enterobacteriaceae in seven Latin American Countries. PLoS ONE. 2016;11: e0154092. https://doi.org/10.1371/journal.pone.0154092.
Veeraraghavan B, Shankar C, Karunasree S, Kumari S, Ravi R, Ralph R. Carbapenem resistant Klebsiella pneumoniae isolated from bloodstream infection: Indian experience. Pathogens Global Health. 2017;111:240–6. https://doi.org/10.1080/20477724.2017.1340128.
Paczosa M, Mecsas J. Klebsiella pneumoniae: going on the offense with a strong defense. Microbiol Mol Biol Rev. 2016;80:629–61. https://doi.org/10.1128/mmbr.00078-15.
Iredell J, Brown J, Tagg K. Antibiotic resistance in Enterobacteriaceae: mechanisms and clinical implications. BMJ (Clin Res ed). 2016;352: h6420. https://doi.org/10.1136/bmj.h6420.
Maraolo A, Corcione S, Grossi A, Signori A, Alicino C, Hussein K, et al. The impact of carbapenem resistance on mortality in patients with klebsiella pneumoniae bloodstream infection: an individual patient data meta-analysis of 1952 patients. Infect Dis Therapy. 2021;10(1):541–58. https://doi.org/10.1007/s40121-021-00408-8.
Garcia-Vidal C, Cardozo-Espinola C, Puerta-Alcalde P, Marco F, Tellez A, Agüero D, et al. Risk factors for mortality in patients with acute leukemia and bloodstream infections in the era of multiresistance. PLoS ONE. 2018;13: e0199531. https://doi.org/10.1371/journal.pone.0199531.
Micozzi A, Gentile G, Minotti C, Cartoni C, Capria S, Ballarò D, et al. Carbapenem-resistant Klebsiella pneumoniae in high-risk haematological patients: factors favouring spread, risk factors and outcome of carbapenem-resistant Klebsiella pneumoniae bacteremias. BMC Infect Dis. 2017;17:203. https://doi.org/10.1186/s12879-017-2297-9.
Trecarichi EM, Pagano L, Martino B, Candoni A, Di Blasi R, Nadali G, et al. Bloodstream infections caused by Klebsiella pneumoniae in onco-hematological patients: clinical impact of carbapenem resistance in a multicentre prospective survey. Am J Hematol. 2016;91:1076–81. https://doi.org/10.1002/ajh.24489.
Wei J, Zhu Q, Sun Z, Wang C. Pseudomonas aeruginosa[The impact of carbapenem-resistance infections on mortality of patients with hematological disorders]. Zhonghua Nei Ke Za Zhi. 2020;59:353–9. https://doi.org/10.3760/cma.j.cn112138-20191104-00728.
de Jonge B, Karlowsky J, Kazmierczak K, Biedenbach D, Sahm D, Nichols W. In vitro susceptibility to ceftazidime–avibactam of carbapenem-non-susceptible enterobacteriaceae isolates collected during the inform global surveillance study (2012 to 2014). Antimicrob Agents Chemother. 2016;60:3163–9. https://doi.org/10.1128/aac.03042-15.
Zhanel G, Lawson C, Adam H, Schweizer F, Zelenitsky S, Lagacé-Wiens P, et al. Ceftazidime–avibactam: a novel cephalosporin/β-lactamase inhibitor combination. Drugs. 2013;73:159–77. https://doi.org/10.1007/s40265-013-0013-7.
Turton J, Woodford N, Glover J, Yarde S, Kaufmann M, Pitt T. Identification of Acinetobacter baumannii by detection of the blaOXA-51-like carbapenemase gene intrinsic to this species. J Clin Microbiol. 2006;44:2974–6. https://doi.org/10.1128/jcm.01021-06.
Savov E, Trifonova A, Kovachka K, Kjosseva E, Strateva T. in vitroAntimicrobial activities of ceftazidime–avibactam, meropenem–vaborbactam and plazomicin against multidrug-resistant and—a pilot Bulgarian study. Infect Dis (London, England). 2019;51:870–3. https://doi.org/10.1080/23744235.2019.1653491.
Merdjan H, Rangaraju M, Tarral A. Safety and pharmacokinetics of single and multiple ascending doses of avibactam alone and in combination with ceftazidime in healthy male volunteers: results of two randomized, placebo-controlled studies. Clin Drug Investig. 2015;35:307–17. https://doi.org/10.1007/s40261-015-0283-9.
https://www.idsociety.org/practice-guideline/amr-guidance/. Accessed 22 March 2022.
van Duin D, Lok J, Earley M, Cober E, Richter S, Perez F, et al. Colistin versus ceftazidime–avibactam in the treatment of infections due to carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2018;66:163–71. https://doi.org/10.1093/cid/cix783.
Hakeam H, Alsahli H, Albabtain L, Alassaf S, Al Duhailib Z, Althawadi S. Effectiveness of ceftazidime–avibactam versus colistin in treating carbapenem-resistant Enterobacteriaceae bacteremia. Int J Infect Dis. 2021;109:1–7. https://doi.org/10.1016/j.ijid.2021.05.079.
Almangour T, Ghonem L, Aljabri A, Alruwaili A, Al Musawa M, Damfu N, et al. Ceftazidime–avibactam versus colistin for the treatment of infections due to carbapenem-resistant enterobacterales: a multicenter cohort study. Infect Drug Resistance. 2022;15:211–21. https://doi.org/10.2147/idr.S349004.
Fang J, Li H, Zhang M, Shi G, Liu M, Wang Y, et al. Klebsiella pneumonia efficacy of ceftazidime–avibactam versus polymyxin b and risk factors affecting clinical outcomes in patients with carbapenem-resistant infections a retrospective study. Front Pharmacol. 2021;12: 780940. https://doi.org/10.3389/fphar.2021.780940.
Castón J, Cano A, Pérez-Camacho I, Aguado J, Carratalá J, Ramasco F, et al. Impact of ceftazidime/avibactam versus best available therapy on mortality from infections caused by carbapenemase-producing Enterobacterales (CAVICOR study). J Antimicrob Chemother. 2022. https://doi.org/10.1093/jac/dkac049.
Shields R, Nguyen M, Chen L, Press E, Potoski B, Marini R, et al. Ceftazidime–avibactam Is Superior to Other Treatment Regimens against Carbapenem-Resistant Klebsiella pneumoniae Bacteremia. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.00883-17.
Gu J, Xu J, Zuo T, Chen Y. Ceftazidime–avibactam in the treatment of infections from carbapenem-resistant Klebsiella pneumoniae: Ceftazidime–avibactam against CR-KP infections. J Global Antimicrobial Resistance. 2021;26:20–5. https://doi.org/10.1016/j.jgar.2021.04.022.
Alraddadi B, Saeedi M, Qutub M, Alshukairi A, Hassanien A, Wali G. Efficacy of ceftazidime–avibactam in the treatment of infections due to Carbapenem-resistant Enterobacteriaceae. BMC Infect Dis. 2019;19:772. https://doi.org/10.1186/s12879-019-4409-1.
Chen L, Han X, Li Y, Li M. Enterobacterales assessment of mortality-related risk factors and effective antimicrobial regimens for treatment of bloodstream infections caused by carbapenem-resistant. Antimicrob Agents Chemother. 2021;65: e0069821. https://doi.org/10.1128/aac.00698-21.
Tsolaki V, Mantzarlis K, Mpakalis A, Malli E, Tsimpoukas F, Tsirogianni A, et al. Ceftazidime–avibactam To Treat Life-Threatening Infections by Carbapenem-Resistant Pathogens in Critically Ill Mechanically Ventilated Patients. Antimicrob Agents Chemother. 2020;64. https://doi.org/10.1128/aac.02320-19.
Shen L, Lian C, Zhu B, Yao Y, Yang Q, Zhou J, et al. Klebsiella pneumonia bloodstream infections due to carbapenem-resistant : a single-center retrospective study on risk factors and therapy options. Microbial drug resistance (Larchmont, NY). 2021;27:227–33. https://doi.org/10.1089/mdr.2019.0455.
Zhong H, Zhao X, Zhang Z, Gu Z, Zhang C, Gao Y, et al. Evaluation of the efficacy and safety of ceftazidime/avibactam in the treatment of Gram-negative bacterial infections: a systematic review and meta-analysis. Int J Antimicrob Agents. 2018;52:443–50. https://doi.org/10.1016/j.ijantimicag.2018.07.004.
Ackley R, Roshdy D, Meredith J, Minor S, Anderson W, Capraro G, et al. Enterobacteriaceae meropenem–vaborbactam versus ceftazidime–avibactam for treatment of carbapenem-resistant infections. antimicrob agents chemother. 2020;64. https://doi.org/10.1128/aac.02313-19.
Castón J, Gallo M, García M, Cano A, Escribano A, Machuca I, et al. Ceftazidime–avibactam in the treatment of infections caused by KPC-producing Klebsiella pneumoniae: factors associated with clinical efficacy in a single-center cohort. Int J Antimicrob Agents. 2020;56: 106075. https://doi.org/10.1016/j.ijantimicag.2020.106075.
Tumbarello M, Trecarichi E, Corona A, De Rosa F, Bassetti M, Mussini C, et al. Efficacy of Ceftazidime–avibactam Salvage Therapy in Patients With Infections Caused by Klebsiella pneumoniae Carbapenemase-producing K. pneumoniae. Clin Infect Dis. 2019;68:355–64. https://doi.org/10.1093/cid/ciy492.
Shields R, Nguyen M, Chen L, Press E, Kreiswirth B, Clancy C. Pneumonia and Renal Replacement Therapy Are Risk Factors for Ceftazidime–avibactam Treatment Failures and Resistance among Patients with Carbapenem-Resistant Enterobacteriaceae Infections. Antimicrob Agents Chemother. 2018;62. https://doi.org/10.1128/aac.02497-17.
Shi Y, Hu J, Liu P, Wang T, Wang H, Liu Y, et al. Ceftazidime–avibactam-based versus tigecycline-based regimen for the treatment of carbapenem-resistant klebsiella pneumoniae-induced pneumonia in critically Ill patients. Infect Dis Therapy. 2021;10:2721–34. https://doi.org/10.1007/s40121-021-00542-3.
Castón J, Lacort-Peralta I, Martín-Dávila P, Loeches B, Tabares S, Temkin L, et al. Clinical efficacy of ceftazidime/avibactam versus other active agents for the treatment of bacteremia due to carbapenemase-producing Enterobacteriaceae in hematologic patients. Int J Infect Dis. 2017;59:118–23. https://doi.org/10.1016/j.ijid.2017.03.021.
Clerici D, Oltolini C, Greco R, Ripa M, Giglio F, Mastaglio S, et al. The place of ceftazidime/avibactam and ceftolozane/tazobactam for therapy of haematological patients with febrile neutropenia. Int J Antimicrob Agents. 2021;57: 106335. https://doi.org/10.1016/j.ijantimicag.2021.106335.
Chen F, Zhong H, Yang T, Shen C, Deng Y, Han L, et al. Klebsiella pneumoniaeCeftazidime–avibactam as Salvage Treatment for Infections Due to Carbapenem-Resistant in Liver Transplantation Recipients. Infect Drug Resistance. 2021;14:5603–12. https://doi.org/10.2147/idr.S342163.
Zhang F, Zhong J, Ding H, Liao G. Klebsiella pneumonia efficacy of ceftazidime–avibactam in the treatment of carbapenem-resistant infection after kidney transplantation. Infect Drug Resistance. 2021;14:5165–74. https://doi.org/10.2147/idr.S343505.
Chen W, Sun L, Guo L, Cao B, Liu Y, Zhao L, et al. Clinical outcomes of ceftazidime–avibactam in lung transplant recipients with infections caused by extensively drug-resistant gram-negative bacilli. Ann Trans Med. 2020;8:39. https://doi.org/10.21037/atm.2019.10.40.
Kuang H, Zhong C, Wang Y, Ye H, Ao K, Zong Z, et al. Clinical characteristics and outcomes of patients with multidrug-resistant Gram-negative bacterial infections treated with ceftazidime/avibactam. J Global Antimicrobial Resistance. 2020;23:404–7. https://doi.org/10.1016/j.jgar.2020.10.023.
King M, Heil E, Kuriakose S, Bias T, Huang V, El-Beyrouty C, et al. Multicenter Study of Outcomes with Ceftazidime–avibactam in Patients with Carbapenem-Resistant Enterobacteriaceae Infections. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.00449-17.
Shields R, Potoski B, Haidar G, Hao B, Doi Y, Chen L, et al. Clinical outcomes, drug toxicity, and emergence of ceftazidime–avibactam resistance among patients treated for carbapenem-resistant enterobacteriaceae infections. Clin Infect Dis. 2016;63:1615–8. https://doi.org/10.1093/cid/ciw636.
King M, Heil E, Kuriakose S, Bias T, Huang V, El-Beyrouty C, et al. Outcomes With Ceftazidime/Avibactam in Patients With Carbapenem-Resistant Enterobacteriaceae (CRE) Infections: A Multicenter Study. Open Forum Infectious Diseases. 2016;3. https://doi.org/10.1093/ofid/ofw172.1595.
De la Calle C, Rodríguez O, Morata L, Marco F, Cardozo C, García-Vidal C, et al. Clinical characteristics and prognosis of infections caused by OXA-48 carbapenemase-producing Enterobacteriaceae in patients treated with ceftazidime–avibactam. Int J Antimicrob Agents. 2019;53:520–4. https://doi.org/10.1016/j.ijantimicag.2018.11.015.
Fiore M, Alfieri A, Di Franco S, Pace M, Simeon V, Ingoglia G, et al. Ceftazidime–avibactam Combination Therapy Compared to Ceftazidime–avibactam Monotherapy for the Treatment of Severe Infections Due to Carbapenem-Resistant Pathogens: A Systematic Review and Network Meta-Analysis. Antibiotics (Basel, Switzerland). 2020;9. https://doi.org/10.3390/antibiotics9070388.
Tumbarello M, Raffaelli F, Giannella M, Mantengoli E, Mularoni A, Venditti M, et al. Ceftazidime–avibactam use for KPC-Kp infections: a retrospective observational multicenter study. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab176.
Karaiskos I, Daikos G, Gkoufa A, Adamis G, Stefos A, Symbardi S, et al. Ceftazidime/avibactam in the era of carbapenemase-producing Klebsiella pneumoniae: experience from a national registry study. J Antimicrob Chemother. 2021;76:775–83. https://doi.org/10.1093/jac/dkaa503.
Zheng G, Zhang J, Wang B, Cai J, Wang L, Hou K, et al. Ceftazidime–avibactam in combination with in vitro non-susceptible antimicrobials versus ceftazidime–avibactam in monotherapy in critically Ill patients with carbapenem-resistant klebsiella pneumoniae infection: a retrospective cohort study. Infect Dis Therapy. 2021;10:1699–713. https://doi.org/10.1007/s40121-021-00479-7.
Shaw E, Rombauts A, Tubau F, Padullés A, Càmara J, Lozano T, et al. Clinical outcomes after combination treatment with ceftazidime/avibactam and aztreonam for NDM-1/OXA-48/CTX-M-15-producing Klebsiella pneumoniae infection. J Antimicrob Chemother. 2018;73:1104–6. https://doi.org/10.1093/jac/dkx496.
Davido B, Fellous L, Lawrence C, Maxime V, Rottman M, Dinh A. Ceftazidime–avibactam and Aztreonam, an Interesting Strategy To Overcome β-Lactam Resistance Conferred by Metallo-β-Lactamases in Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.01008-17.
Bocanegra-Ibarias P, Camacho-Ortiz A, Garza-González E, Flores-Treviño S, Kim H, Perez-Alba E. Aztreonam plus ceftazidime–avibactam as treatment of NDM-1-producing Klebsiella pneumoniae bacteraemia in a neutropenic patient: Last resort therapy? J Global Antimicrobial Resistance. 2020;23:417–9. https://doi.org/10.1016/j.jgar.2020.10.019.
Benchetrit L, Mathy V, Armand-Lefevre L, Bouadma L, Timsit J. Successful treatment of septic shock due to NDM-1-producing Klebsiella pneumoniae using ceftazidime/avibactam combined with aztreonam in solid organ transplant recipients: report of two cases. Int J Antimicrob Agents. 2020;55: 105842. https://doi.org/10.1016/j.ijantimicag.2019.10.023.
Yasmin M, Fouts D, Jacobs M, Haydar H, Marshall S, White R, et al. Monitoring Ceftazidime–avibactam and Aztreonam Concentrations in the Treatment of a Bloodstream Infection Caused by a Multidrug-Resistant Enterobacter sp. Carrying Both Klebsiella pneumoniae Carbapenemase-4 and New Delhi Metallo-β-Lactamase-1. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2020;711095–8. https://doi.org/10.1093/cid/ciz1155.
Sieswerda E, van den Brand M, van den Berg R, Sträter J, Schouls L, van Dijk K, et al. Successful rescue treatment of sepsis due to a pandrug-resistant, NDM-producing Klebsiella pneumoniae using aztreonam powder for nebulizer solution as intravenous therapy in combination with ceftazidime/avibactam. J Antimicrob Chemother. 2020;75:773–5. https://doi.org/10.1093/jac/dkz495.
Falcone M, Daikos G, Tiseo G, Bassoulis D, Giordano C, Galfo V, et al. Efficacy of ceftazidime–avibactam plus aztreonam in patients with bloodstream infections caused by MBL- producing Enterobacterales. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa586.
Bernhard M, Lichtenstern C, Eckmann C, Weigand M. The early antibiotic therapy in septic patients–milestone or sticking point? Crit Care. 2014;18:671. https://doi.org/10.1186/s13054-014-0671-1.
Falcone M, Bassetti M, Tiseo G, Giordano C, Nencini E, Russo A, et al. Time to appropriate antibiotic therapy is a predictor of outcome in patients with bloodstream infection caused by KPC-producing Klebsiella pneumoniae. Crit Care. 2020;24:29. https://doi.org/10.1186/s13054-020-2742-9.
Jorgensen S, Trinh T, Zasowski E, Lagnf A, Bhatia S, Melvin S, et al. Real-World Experience With Ceftazidime–avibactam for Multidrug-Resistant Gram-Negative Bacterial Infections. Open forum infectious diseases. 2019;6:ofz522. https://doi.org/10.1093/ofid/ofz522.
Guimarães T, Nouér S, Martins R, Perdigão Neto L, Martins W, Narciso Barbosa A, et al. EnterobacterialesCeftazidime–avibactam as Salvage Therapy for Infections Caused by Coresistant to Carbapenems and Polymyxins. Antimicrob Agents Chemother. 2019;63. https://doi.org/10.1128/aac.00528-19.
Onorato L, Di Caprio G, Signoriello S, Coppola N. Efficacy of ceftazidime/avibactam in monotherapy or combination therapy against carbapenem-resistant Gram-negative bacteria: a meta-analysis. Int J Antimicrob Agents. 2019;54:735–40. https://doi.org/10.1016/j.ijantimicag.2019.08.025.
Iannaccone M, Boattini M, Bianco G, Corcione S, Cavallo R, Costa C. EnterobacteralesCeftazidime–avibactam susceptible to resistant KPC-producing bloodstream infections: an observational study. J Chemotherapy (Florence, Italy). 2020;32:160–2. https://doi.org/10.1080/1120009x.2019.1709363.
Shields R, Chen L, Cheng S, Chavda K, Press E, Snyder A, et al. blaEmergence of Ceftazidime–avibactam Resistance Due to Plasmid-Borne Mutations during Treatment of Carbapenem-Resistant Klebsiella pneumoniae Infections. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.02097-16.
Shields R, Nguyen M, Press E, Chen L, Kreiswirth B, Clancy C. Klebsiella pneumonia emergence of ceftazidime–avibactam resistance and restoration of carbapenem susceptibility in carbapenemase-producing: a case report and review of literature. Open forum infectious diseases. 2017;4:ofx101. https://doi.org/10.1093/ofid/ofx101.
Giddins M, Macesic N, Annavajhala M, Stump S, Khan S, McConville T, et al. blaSuccessive emergence of ceftazidime–avibactam resistance through distinct genomic adaptations in -harboring klebsiella pneumoniae sequence type 307 isolates. Antimicrob Agents Chemother. 2018;62. https://doi.org/10.1128/aac.02101-17.
Castanheira M, Arends S, Davis A, Woosley L, Bhalodi A, MacVane S. Citrobacter freundiiAnalyses of a Ceftazidime–avibactam-Resistant Isolate Carrying Reveals a Heterogenous Population and Reversible Genotype. mSphere. 2018;3. https://doi.org/10.1128/mSphere.00408-18.
Athans V, Neuner E, Hassouna H, Richter S, Keller G, Castanheira M, et al. Klebsiella pneumoniaeMeropenem–vaborbactam as Salvage Therapy for Ceftazidime–avibactam-Resistant Bacteremia and Abscess in a Liver Transplant Recipient. Antimicrob Agents Chemother. 2019;63. https://doi.org/10.1128/aac.01551-18.
Hemarajata P, Humphries R. Ceftazidime/avibactam resistance associated with L169P mutation in the omega loop of KPC-2. J Antimicrob Chemother. 2019;74(5):1241–3. https://doi.org/10.1093/jac/dkz026.
Gaibani P, Campoli C, Lewis R, Volpe S, Scaltriti E, Giannella M, et al. In vivo evolution of resistant subpopulations of KPC-producing Klebsiella pneumoniae during ceftazidime/avibactam treatment. J Antimicrob Chemother. 2018;73:1525–9. https://doi.org/10.1093/jac/dky082.
Antonelli A, Giani T, Di Pilato V, Riccobono E, Perriello G, Mencacci A, et al. KPC-31 expressed in a ceftazidime/avibactam-resistant Klebsiella pneumoniae is associated with relevant detection issues. J Antimicrob Chemother. 2019;74:2464–6. https://doi.org/10.1093/jac/dkz156.
Venditti C, Nisii C, D’Arezzo S, Vulcano A, Capone A, Antonini M, et al. blaMolecular and phenotypical characterization of two cases of antibiotic-driven ceftazidime–avibactam resistance in -harboring. Infect Drug Resistance. 2019;12:1935–40. https://doi.org/10.2147/idr.S207993.
Gaibani P, Ambretti S, Campoli C, Viale P, Re M. Genomic characterization of a Klebsiella pneumoniae ST1519 resistant to ceftazidime/avibactam carrying a novel KPC variant (KPC-36). Int J Antimicrob Agents. 2020;55: 105816. https://doi.org/10.1016/j.ijantimicag.2019.09.020.
Galani I, Karaiskos I, Souli M, Papoutsaki V, Galani L, Gkoufa A, et al. Klebsiella pneumoniaeOutbreak of KPC-2-producing endowed with ceftazidime–avibactam resistance mediated through a VEB-1-mutant (VEB-25), Greece, September to October 2019. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 2020;25. https://doi.org/10.2807/1560-7917.Es.2020.25.3.2000028.
Galani I, Karaiskos I, Angelidis E, Papoutsaki V, Galani L, Souli M, et al. Emergence of ceftazidime–avibactam resistance through distinct genomic adaptations in KPC-2-producing Klebsiella pneumoniae of sequence type 39 during treatment. Euro J Clin Microbiol Infect Dis. 2021;40(1):219–24. https://doi.org/10.1007/s10096-020-04000-9.
Cano Á, Guzmán-Puche J, García-Gutiérrez M, Castón J, Gracia-Ahufinger I, Pérez-Nadales E, et al. Use of carbapenems in the combined treatment of emerging ceftazidime/avibactam-resistant and carbapenem-susceptible KPC-producing Klebsiella pneumoniae infections: Report of a case and review of the literature. J Global Antimicrobial Resistance. 2020;22:9–12. https://doi.org/10.1016/j.jgar.2019.11.007.
Guzmán-Puche J, Pérez-Nadales E, Pérez-Vázquez M, Causse M, Gracia-Ahufinger I, Mendez-Natera A, et al. In vivo selection of KPC-94 and KPC-95 in Klebsiella pneumoniae isolates from patients treated with ceftazidime/avibactam. Int J Antimicrob Agents. 2022;59: 106524. https://doi.org/10.1016/j.ijantimicag.2022.106524.
Li X, Quan J, Ke H, Wu W, Feng Y, Yu Y, et al. Klebsiella pneumonia emergence of a KPC variant conferring resistance to ceftazidime–avibactam in a widespread ST11 carbapenem-resistant clone in China. Front Microbiol. 2021;12: 724272. https://doi.org/10.3389/fmicb.2021.724272.
Shen S, Shi Q, Han R, Guo Y, Yang Y, Wu S, et al. blaIsolation of a Ceftazidime–avibactam-Resistant -Positive Klebsiella pneumoniae Clinical Isolate. Microbiology spectrum. 2022;10: e0184021. https://doi.org/10.1128/spectrum.01840-21.
Räisänen K, Koivula I, Ilmavirta H, Puranen S, Kallonen T, Lyytikäinen O, et al. Klebsiella pneumoniaeEmergence of ceftazidime–avibactam-resistant during treatment, Finland, December 2018. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 2019;24. https://doi.org/10.2807/1560-7917.Es.2019.24.19.1900256.
Göttig S, Frank D, Mungo E, Nolte A, Hogardt M, Besier S, et al. Emergence of ceftazidime/avibactam resistance in KPC-3-producing Klebsiella pneumoniae in vivo. J Antimicrob Chemother. 2019;74:3211–6. https://doi.org/10.1093/jac/dkz330.
Mueller L, Masseron A, Prod’Hom G, Galperine T, Greub G, Poirel L, et al. Phenotypic, biochemical and genetic analysis of KPC-41, a KPC-3 variant conferring resistance to ceftazidime–avibactam and exhibiting reduced carbapenemase activity. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/aac.01111-19.
Wang Y, Wang J, Wang R, Cai Y. Resistance to ceftazidime–avibactam and underlying mechanisms. J Global Antimicrobial Resistance. 2020;22:18–27. https://doi.org/10.1016/j.jgar.2019.12.009.
Galani I, Karaiskos I, Giamarellou H. Klebsiella pneumoniaeMultidrug-resistant : mechanisms of resistance including updated data for novel β-lactam-β-lactamase inhibitor combinations. Expert Rev Anti Infect Ther. 2021;19:1457–68. https://doi.org/10.1080/14787210.2021.1924674.
Winkler M, Papp-Wallace K, Bonomo R. Activity of ceftazidime/avibactam against isogenic strains of Escherichia coli containing KPC and SHV β-lactamases with single amino acid substitutions in the Ω-loop. J Antimicrob Chemother. 2015;70:2279–86. https://doi.org/10.1093/jac/dkv094.
Both A, Büttner H, Huang J, Perbandt M, Belmar Campos C, Christner M, et al. Emergence of ceftazidime/avibactam non-susceptibility in an MDR Klebsiella pneumoniae isolate. J Antimicrob Chemother. 2017;72:2483–8. https://doi.org/10.1093/jac/dkx179.
Livermore D, Mushtaq S, Doumith M, Jamrozy D, Nichols W, Woodford N. Selection of mutants with resistance or diminished susceptibility to ceftazidime/avibactam from ESBL- and AmpC-producing Enterobacteriaceae. J Antimicrob Chemother. 2018;73:3336–45. https://doi.org/10.1093/jac/dky363.
Porres-Osante N, Dupont H, Torres C, Ammenouche N, de Champs C, Mammeri H. Avibactam activity against extended-spectrum AmpC β-lactamases. J Antimicrob Chemother. 2014;69:1715–6. https://doi.org/10.1093/jac/dku002.
Fröhlich C, Sørum V, Thomassen A, Johnsen P, Leiros H, Samuelsen Ø. OXA-48-Mediated Ceftazidime–avibactam Resistance Is Associated with Evolutionary Trade-Offs. mSphere. 2019;4. https://doi.org/10.1128/mSphere.00024-19.
Nelson K, Hemarajata P, Sun D, Rubio-Aparicio D, Tsivkovski R, Yang S, et al. Resistance to Ceftazidime–avibactam Is Due to Transposition of KPC in a Porin-Deficient Strain of Klebsiella pneumoniae with Increased Efflux Activity. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.00989-17.
Shields R, Clancy C, Hao B, Chen L, Press E, Iovine N, et al. Effects of Klebsiella pneumoniae carbapenemase subtypes, extended-spectrum β-lactamases, and porin mutations on the in vitro activity of ceftazidime–avibactam against carbapenem-resistant K. pneumoniae. Antimicrob Agents Chemother. 2015;59:5793–7. https://doi.org/10.1128/aac.00548-15.
Zhang Y, Kashikar A, Brown C, Denys G, Bush K. In VitroUnusual Escherichia coli PBP 3 Insertion Sequence Identified from a Collection of Carbapenem-Resistant Enterobacteriaceae Tested with a Combination of Ceftazidime-, Ceftaroline-, or Aztreonam-Avibactam. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.00389-17.
Fontana C, Favaro M, Campogiani L, Malagnino V, Minelli S, Bossa M, et al. Klebsiella pneumoniaeCeftazidime/Avibactam-Resistant subsp. Isolates in a Tertiary Italian Hospital: Identification of a New Mutation of the Carbapenemase Type 3 (KPC-3) Gene Conferring Ceftazidime/Avibactam Resistance. Microorganisms. 2021;9. https://doi.org/10.3390/microorganisms9112356.
Sheu C, Chang Y, Lin S, Chen Y, Hsueh P. Enterobacteriaceae infections caused by carbapenem-resistant: an update on therapeutic options. Front Microbiol. 2019;10:80. https://doi.org/10.3389/fmicb.2019.00080.
Humphries RM, Yang S, Hemarajata P, Ward KW, Hindler JA, Miller SA, et al. First report of ceftazidime–avibactam resistance in a KPC-3-expressing <span class="named-content genus-species" id="named-content-1">Klebsiella pneumoniae</span> Isolate. Antimicrob Agents Chemother. 2015;59(10):6605. https://doi.org/10.1128/AAC.01165-15.
Gaibani P, Re M, Campoli C, Viale P, Ambretti S. Bloodstream infection caused by KPC-producing Klebsiella pneumoniae resistant to ceftazidime/avibactam: epidemiology and genomic characterization. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2020;26:516.e1-.e4. https://doi.org/10.1016/j.cmi.2019.11.011.
Corbella L, Boán J, San-Juan R, Fernández-Ruiz M, Carretero O, Lora D, et al. Effectiveness of ceftazidime–avibactam for the treatment of infections due to Pseudomonas aeruginosa. Int J Antimicrob Agents. 2022;59: 106517. https://doi.org/10.1016/j.ijantimicag.2021.106517.
Chen J, Liang Q, Chen X, Wu J, Wu Y, Teng G, et al. Pseudomonas aeruginosa ceftazidime/avibactam versus polymyxin B in the challenge of carbapenem-resistant infection. Infect Drug Resistance. 2022;15:655–67. https://doi.org/10.2147/idr.S350976.
Vena A, Giacobbe D, Castaldo N, Cattelan A, Mussini C, Luzzati R, et al. EnterobacteralesClinical Experience with Ceftazidime–avibactam for the Treatment of Infections due to Multidrug-Resistant Gram-Negative Bacteria Other than Carbapenem-Resistant. Antibiotics (Basel, Switzerland). 2020;9. https://doi.org/10.3390/antibiotics9020071.
Rodríguez-Núñez O, Ripa M, Morata L, de la Calle C, Cardozo C, Fehér C, et al. Evaluation of ceftazidime/avibactam for serious infections due to multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa. J Global Antimicrobial Resistance. 2018;15:136–9. https://doi.org/10.1016/j.jgar.2018.07.010.
Santevecchi B, Smith T, MacVane S. Clinical experience with ceftazidime/avibactam for treatment of antibiotic-resistant organisms other than Klebsiella pneumoniae. Int J Antimicrob Agents. 2018;51:629–35. https://doi.org/10.1016/j.ijantimicag.2018.01.016.
Meschiari M, Franconi I, Bacca E, Bianco V, Orlando G, Cuomo G, et al. Ceftazidime/avibactam and ceftolozane/tazobactam for the treatment of extensively drug-resistant Pseudomonas aeruginosa post-neurosurgical infections: three cases and a review of the literature. Infection. 2021;49:549–53. https://doi.org/10.1007/s15010-020-01539-9.
Almangour T, Alsubaie S, Ghonem L, Almohaini H, Mohammed Bakheet H, Altweijri I. Ceftazidime–avibactam for the treatment of multidrug-resistant Pseudomonas aeruginosa central nervous system infection in pediatric patient: a case report. Pediatr Infect Dis J. 2021. https://doi.org/10.1097/inf.0000000000003439.
Gatti M, Virgili G, Cojutti P, Gaibani P, Conti M, Sturiale C, et al. Real-Time Optimization of Pharmacodynamic Target Attainment at Infection Site during Treatment of Post-Neurosurgical Ventriculitis Caused by Carbapenem-Resistant Gram Negatives with Ceftazidime–avibactam-Based Regimens: A Report of Two Cases. Microorganisms. 2022;10. https://doi.org/10.3390/microorganisms10010154.
Ruedas-López A, Alonso-García I, Lasarte-Monterrubio C, Guijarro-Sánchez P, Gato E, Vázquez-Ucha J, et al. Selection of AmpC β-Lactamase variants and metallo-β-lactamases leading to ceftolozane/tazobactam and ceftazidime/avibactam resistance during treatment of MDR/XDR pseudomonas aeruginosa infections. Antimicrob Agents Chemother. 2022;66(2): e0206721. https://doi.org/10.1128/aac.02067-21.
Fraile-Ribot P, Fernández J, Gomis-Font M, Forcelledo L, Mulet X, López-Causapé C, et al. In Vivo Evolution of GES β-lactamases driven by ceftazidime/avibactam treatment of pseudomonas aeruginosa infections. Antimicrob Agents Chemother. 2021;65: e0098621. https://doi.org/10.1128/aac.00986-21.
Fraile-Ribot P, Mulet X, Cabot G, Del Barrio-Tofiño E, Juan C, Pérez J, et al. In Vivo Emergence of Resistance to Novel Cephalosporin-β-Lactamase Inhibitor Combinations through the Duplication of Amino Acid D149 from OXA-2 β-Lactamase (OXA-539) in Sequence Type 235 Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2017;61. https://doi.org/10.1128/aac.01117-17.
Boulant T, Jousset A, Bonnin R, Barrail-Tran A, Borgel A, Oueslati S, et al. Pseudomonas aeruginosaA 2.5-years within-patient evolution of a with acquisition of ceftolozane-tazobactam and ceftazidime–avibactam resistance upon treatment. Antimicrob Agents Chemother. 2019. https://doi.org/10.1128/aac.01637-19.
Arca-Suárez J, Lasarte-Monterrubio C, Rodiño-Janeiro B, Cabot G, Vázquez-Ucha J, Rodríguez-Iglesias M, et al. Molecular mechanisms driving the in vivo development of OXA-10-mediated resistance to ceftolozane/tazobactam and ceftazidime/avibactam during treatment of XDR Pseudomonas aeruginosa infections. J Antimicrob Chemother. 2021;76:91–100. https://doi.org/10.1093/jac/dkaa396.
Horcajada J, Montero M, Oliver A, Sorlí L, Luque S, Gómez-Zorrilla S, et al. Epidemiology and Treatment of Multidrug-Resistant and Extensively Drug-Resistant Pseudomonas aeruginosa Infections. Clin Microbiol Rev. 2019;32. https://doi.org/10.1128/cmr.00031-19.
Tu Y, Wang D, Zhu Y, Li J, Jiang Y, Wu W, et al. Emergence of a KPC-90 Variant that Confers Resistance to Ceftazidime–avibactam in an ST463 Carbapenem-Resistant Pseudomonas aeruginosa Strain. Microbiology spectrum. 2022;10: e0186921. https://doi.org/10.1128/spectrum.01869-21.
Zhu Y, Chen J, Shen H, Chen Z, Yang Q, Zhu J, et al. Emergence of Ceftazidime- and Avibactam-Resistant Klebsiella pneumoniae Carbapenemase-Producing Pseudomonas aeruginosa in China. mSystems. 2021;6:e0078721. https://doi.org/10.1128/mSystems.00787-21.
Funding
This work received grant from funding CAMS Innovation Fund for Medical Sciences (CIFMS) 2021-I2M-C&T-B-080 and 2021-I2M-017.
Author information
Authors and Affiliations
Contributions
SZ and HW drafted the manuscript, and Sizhou Feng critically revised and approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to report.
Ethical approval
Not required.
Rights and permissions
About this article
Cite this article
Zhen, S., Wang, H. & Feng, S. Update of clinical application in ceftazidime–avibactam for multidrug-resistant Gram-negative bacteria infections. Infection 50, 1409–1423 (2022). https://doi.org/10.1007/s15010-022-01876-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-022-01876-x