Abstract
Introduction
Real-world evidence (RWE) data is increasingly important to generate rapid insights to effectively manage patient populations. Disruptions like the coronavirus disease 2019 (COVID-19) pandemic may negatively impact the choice of medications used for managing chronic diseases such as psoriasis (PSO). Here, we explored the effect of the COVID-19 pandemic on the sales volumes of treatment guideline-based PSO medication in Germany.
Methods
Patient-level pharmacy dispensing data from the Permea platform, covering approximately 44% of all community pharmacy dispensing in Germany, were analysed from 2019 through to 2021. Patient demographics and PSO indicated medication sales were assessed specifically before and during the pandemic in Germany.
Results
We included 6,865,852 sold PSO related drugs from April 2019 to March 2021. Medication sales increased during the pandemic compared with before the pandemic for treatment classes of first-line biological and second-line drugs. The increase was observed across all age groups, but monthly variations could not be detected. Furthermore, we observed increased sales in first-line biological and second-line medications when comparing low to high COVID-19 incidence state.
Conclusion
Throughout the COVID-19 pandemic the PSO indicated medication sales increased for first-line biological and second-line treatment. This shows that despite the pandemic impact, there continues to be an increase in sales volume for biologics. Only German federal states with intermittently very high COVID-19 incidences show a stagnation in sales volume. The reasons for this need to be investigated in further studies to possibly gain a better understanding of the concerns and uncertainties of patients with PSO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Value of real-world evidence (RWE) data for managing patient populations, especially during events like COVID-19 has grown. |
COVID-19 potentially affected choice and sales of psoriasis medication in Germany. |
Despite the COVID-19 pandemic, an increase in sales of first-line biological and second-line psoriasis (PSO) treatments was noted, except in German regions with very high COVID-19 incidences where sales stagnated. |
Further studies are required to understand the causes of this sales stagnation and potentially shed light on concerns and uncertainties of patients with PSO in areas heavily affected by COVID-19. |
Introduction
In March 2020 the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a global pandemic, which led to a major disruption in vast areas of daily life, affecting millions of lives worldwide. Vulnerable groups suffering from chronic diseases were especially faced with uncertainty as to whether they were at an increased risk of a severe life-threatening course of a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [1,2,3].
Psoriasis vulgaris – also known as chronic plaque psoriasis – is a relapsing chronic condition and is the most common form of psoriasis [4, 5], affecting at least 60 million individuals globally as of 2016 [6] and approximately 2 million individuals in Germany as of 2019 [7]. The disease can occur at any age, but is most prevalent within the age group of 55–75 years [7]. The pandemic has affected the treatment approach of PSO, not only for those already seeking treatment, but also for those beginning a new therapy to control their disease [1]. The treatment regimen depends on the severity and comorbidities of the disease [8]. While mild to moderate PSO can be treated topically with a combination of glucocorticoids, vitamin D analogues, and phototherapy, moderate to severe PSO often requires systemic treatment, including biologics and small molecules [9]. Although the German psoriasis experts like the National Psoriasis Foundation COVID-19 Task Force [10] still recommend that patients who are not infected with SARS-CoV-2 continue their biologics for PSO in most cases, patients fear that since immunosuppressant therapy inhibit immune-mediated pathways, they may be at increased risk for an infection [11]. These concerns increased during the outbreak of COVID-19 and the resulting media coverage increased. As a result, patients increasingly turned to healthcare providers for guidance regarding the use of biologic agents during the pandemic [11].
Existing research suggests that stress might trigger and increase the severity of psoriatic flares and symptoms [12, 13]. Evidence indicates that the ongoing effects of the global COVID-19 pandemic and subsequent preventative measures have increased stress levels in the general population, from both a physical and mental health perspective [14, 15]. Currently, there is no existing knowledge whether the impact of the pandemic on chronic diseases such as psoriasis alters the medication behaviour in patients. One of the possibilities to detect potential changes in therapy changes is the prescribed type of PSO treatment. The purpose of this research paper is to investigate the impact of the ongoing COVID-19 pandemic on prescription drug use in patients with a PSO diagnosis in Germany. This research will draw on insights derived from prescription and sales data obtained from pharmacies within Germany and aims to determine whether patients have changed their treatment regimen throughout the course of the COVID-19 pandemic.
Methods
Analysis Design
The analysis was performed in a retrospective manner and included prescription sales data of PSO-specific medications.
Data Source and Data Collection
The data for this analysis was provided by the Permea data platform (Temedica GmbH), and were initially collected by the Noventi Health SE. The dataset encompassed the patient-level pharmacy dispensing data from 8246 pharmacies across Germany, covering approximately 44% of community pharmacy dispensing in Germany. Data was collected between April 2019 and March 2021 for all medications that were prescribed for the treatment of PSO according to the PSO German National Guidelines (S3-Guideline) [16]. After filtering for the study period and PSO medications, the data was stored in the Permea Data Platform in a General Data Protection Regulation (GDPR) compliant manner and no personal information, which might allow identification of individuals, was revealed. Age of the patient was only available if there was a minimum of seven patients related to the data source. Ethical approval was not needed for our analysis since the data analysed here retrospectively is anonymized prescription sales data.
Data Processing and Analysis
The data was further processed and analysed with Python 3.9. Statistical tests were conducted with Prism 9.3.1. We further classified the medication in different groups based on the current German guideline for the treatment of PSO [16] to better assess the sales of drugs (Table 1).
To account for the variability in participating pharmacies throughout our study period, we reported our results as a count per pharmacy (Supplementary Fig. 1). The number of unique pharmacies using the system served as a baseline for the denominator.
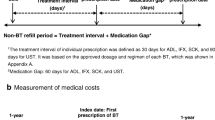
To assess the changes in sales data during the pandemic, we divided the dataset into two different time periods. The pre-pandemic dataset covered the period 04/2019 to 03/2020 and the pandemic dataset covered the period 04/2020 to 03/2021. The changes in the two periods studied for PSO drugs were calculated for the average prescription numbers per pharmacy per month. First, we performed a Kolmogorov–Smirnov test to examine the distribution of the data. Then we investigated the significance levels in the sales data by using a t-test.
Reported values represent mean ± standard error of the mean and the alpha level is set to 5%.
Impact of Incidence Rates
To find out whether the level of local COVID-19 incidence rates have an impact on sales data, we compared sales data from two German federal states. Since only the first two digits of the selling pharmacy’s postcode were available in our sales data due to data protection, we chose federal states whose state borders corresponded as closely as possible to the two-digit postcode regions. In addition, the two selected federal states should have a similar number of inhabitants and preferably different COVID-19 incidence rates within a certain period of time [17]. Based on the above-mentioned reasons, we decided on the federal states of Schleswig–Holstein [18] and Saxony [19]. We then examined how the sales data in both federal states changed during the period 10/19–02/20 before the pandemic to the pandemic period 10/20–02/21. Within the pandemic period, Schleswig–Holstein had a maximum 7-days incidence of 109.1 per 100,000 inhabitants, compared with Saxony’s maximum 7-days incidence of 504.4 per 100,000 inhabitants.
Results
The data set of sales included 8246 pharmacies with 6,865,852 sold PSO related drugs. The largest proportion of prescriptions was assigned to patients in the 66+ years age group with 2,551,880 (38.03%), followed by the 55–65 years age group with 1,336,825 prescriptions (19.92%) (Fig. 1A) (age group 46–55 years = 913,052; age group 36–45 years = 681,020; age group 26–35 years = 573,488; age group 18–25 years = 310,526; age group < 18 years = 342,829).
The largest share of the total 6,865,852 medicines prescribed fell in the group topical with 5,441,145 drug packages (79.25%) (Fig. 1B). The second largest group was first-line non-biological with 912,108 packages sold (13.28%). The difference between the number of absolute prescriptions and the number of absolute drugs sold results from the different number of drug packages prescribed per prescription.
Figure 1C shows the distribution of age groups based on medication groups. It can be seen that the percentage of the 66+ years age group is higher in the topical and first-line non-biological medication group than in the first-line biological and second-line medication group (38.70% and 44.02% versus 16.64% and 21.32%). The age groups 26–35 years and 18–25 years form the smallest proportion (3.59% and 1.51%, respectively) in the medication group first-line non-biological, the highest proportion of these age groups is shown in the medication groups first-line biological (13.48% and 4.06%) and second-line (12.76% and 5.52%). In the group of people under 18 years of age, the largest share per medication group is formed by topical medications (5.90%).
Since the number of reporting pharmacies varies per month (Supplementary Fig. 1), we analysed the monthly dispensing quantities based on the monthly dispensing quantity per pharmacy. An overview of the dispensing history during the period under investigation is provided by Fig. 2.
Impact of the Pandemic
The aim was to investigate the impact of the COVID-19 pandemic on the prescription of PSO drugs. For this purpose, we analysed the mean dispensing volume per pharmacy in the last year before the pandemic compared to the mean dispensing volume in the first year of the pandemic.
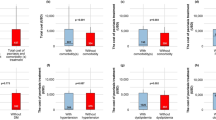
The results showed a significant increase in the amount of drugs prescribed in both the first-line biological group (1.43 drugs per pharmacy pre-pandemic versus 1.72 drugs per pharmacy during the pandemic, P = 0.0005) and the second-line group (1.14 drugs per pharmacy pre-pandemic versus 1.32 drugs per pharmacy during the pandemic, P = 0.0010) (Fig. 3C, D).
Mean number of drugs sold per pharmacy for medication groups A Topical drugs. B First-line non-biological drugs. C First-line biological drugs. D Second-line drugs. Pre-pandemic describes the time 04/19–03/20, pandemic describes the time 04/20–03/21; whiskers show the standard error of mean. ***P ≤ 0.001
The topical group also showed a slight, non-significant increase (30.97 versus 31.73, P = 0.4673), whereas the first-line non-biological group was the only group to show a slight decrease (5.29 versus 5.21, P = 0.6901) (Fig. 3A, B).
We also analysed the first-line biological and second-line medication groups regarding changes in the quantities dispensed in relation to the age groups: For the first-line biological medication group, there was a significant increase in the quantities dispensed in all age groups from before the pandemic compared to the first year of the pandemic (Fig. 4A). The largest increase was observed in groups 36–45 years (0.246 drugs sold per pharmacy pre-pandemic versus 0.306 drugs sold per pharmacy throughout the pandemic, P < 0.0001), 46–55 years (0.300 versus 0.359, P = 0.0006) and 56–65 years (0.362 versus 0.418, P < 0.0001). The increase was least in the < 18 years group (0.032 versus 0.045, P = 0.0001).
In the second-line medication group (Fig. 4B), the largest increase was seen in the age groups 26–35 years (0.154 drugs sold per pharmacy pre-pandemic versus 0.190 drugs sold per pharmacy throughout the pandemic, P < 0.0001) and 36–45 years (0.190 versus 0.225, P = 0.0003). The increase was not significant in the groups < 18 years (0.031 versus 0.034, P = 0.0636) and 65+ years (0.279 versus 0.301, P = 0.0891). All unmentioned values can be seen in Supplementary Table 1.
Impact of Incidence Rates
To evaluate whether the incidence values had a possible influence on prescribing behaviour during the pandemic, we analysed the dispensing quantities per pharmacy for the medication groups before and during the pandemic for two different federal states in Germany.
In this sub-analysis, in line with the nationwide analysis, there was a significant increase in the dispensing of first-line biological and second-line drugs in Schleswig–Holstein (2.35 versus 2.79 in the first-line biological group, P = 0.0167; 2.13 versus 2.50 in the second-line group, P = 0.0329) (Fig. 5A). In comparison, there was a slight but not significant increase in Saxony in the first-line biological and second-line drug groups (1.79 versus 2.12 in first-line biological, P = 0.1057; 1.77 versus 2.01 in second line, P = 0.2078) (Fig. 5B). All unmentioned values can be seen in Supplementary Table 1.
Discussion
In this study we evaluated the influence of the COVID-19 pandemic on the patient-level dispensing of pharmacies across Germany. We therefore analysed two distinct time periods in our data set – 1 year before the WHO declared the COVID-19 outbreak a global pandemic, and 1 year during the pandemic, which included a total of 6,709,620 of PSO related prescriptions.
Augustin et al. [7] showed that most people diagnosed with PSO are between 55 and 75 years old – this is also reflected in our prescription data where, taken together, the over 56-year-olds received more than 50% of PSO related medications, showing that our data set goes along with our data.
The treatment of PSO depends on the severity and comorbidities of the disease [8]. As reported by Vanderpuye-Orgle et al., 83.3% of patients suffer from mild and 11.4% from moderate PSO [20]. Mild PSO can be treated topically, which is reflected in our drug sales data, where topical medicines account for more than three-quarters of all sales. However, this high proportion of topical medicines may also be partly due to patients with moderate to severe PSO, where a combination of topical and systemic therapy may be used. Patients with moderate to severe PSO require systemic treatment, including biologics and small molecules [9]. According to the German National Guideline for PSO treatment patients suffering from a severe form of PSO should be treated with first-line non-biological drugs, including acitretin, ciclosporin, fumarate or methotrexate. However, there are also criteria for which it is recommended to treat immediately with a first-line biologic, such as a particularly severe manifestation or rapid worsening, or a heavy infestation of the nails, genital area or scalp [16]. The sales rate of about 13% appears to be considerably higher than the proportion of patients (5.3%) suffering from a severe form of the disease. This could be due to the fact that the drugs used here are also approved for other indications, e.g., to prevent graft rejection after organ transplantation or other rheumatological diseases, and that some of the purchases are made by patients who do not suffer from PSO. For the proportion of patients where the symptoms do not improve with first-line non-biological medication treatment or where there are contraindications for a specific active ingredient, medication regimen is either extended by first-line biological, replaced by first-line biological or second-line medication, respectively. Since only a comparably small proportion of patients are diagnosed with severe PSO, first-line biological and second-line medications represent the smallest part of the sales numbers.
During the two investigated years we were not able to see any significant monthly variations over time (Fig. 2). We observed specific peaks of sales – namely in the months of July and December, which could be due to patients’ bulk buying before vacations in Germany. Patients treated for PSO are treated with a specific therapy regime over a longer period of time to fully assess the effectiveness of the therapy. Most systematic medications have an induction phase of 10–16 weeks in the case of fast-acting medications, or 16–24 weeks for slow-acting medications [16]. Therefore, monthly variations in sales are unlikely.
Ninosu et al. [21] showed in their study on psoriasis care in a German university hospital that 9.8% of respondents changed their treatment regime during the COVID-19 pandemic. A 90% proportion of the therapy changes were related to treatment with biologics. Of these, 55% consisted of a pause or complete discontinuation of the current regimen. Based on these findings, we expected a decrease sales volume for PSO-specific biologics, when actually we observed the opposite. Interestingly, sales of first-line biologic and second-line drugs increased during the pandemic when comparing total sales before and during the pandemic. One could argue that this indicates an exacerbation of patients’ disease and symptoms during the pandemic. Sales volume for PSO-specific biologics has been increasing continuously over the past several years [22], and the options of treatment possibilities have widened. According to the Psoriasis Drugs Market Research Report the market for PSO-medication is growing due to a rapidly ageing population, increasing number of patients with PSO and surging number of research programmes and drug launches could be a driver for increased sales volume, not only in Germany, but worldwide [23]. During the pandemic in Germany, medications for intensive care units like propofol and arterenol, and also anti-depressants, antibiotics and pain medication, were scarce due to the impact the pandemic had on the manufacturing and supply chain [24]. Although the COVID-19 pandemic lead to major disruptions in healthcare sector and related infrastructure, the pandemic has not affected the market for PSO drug much, due to the recent launch of some major drugs and their increased sales [23]. Additionally, during the lockdown phases many physicians introduced online appointments, allowing a consultation from home and the prescription of medication via the phone, thereby enabling a continuous care of patients. These points could also contribute to the increase, not decrease, of sales for PSO-related medications.
Patients on immunosuppressive medications especially fear their therapy may place them at an increased risk of infection [11]. These critical points raised the concern that PSO-patients could be at higher risk for a severe SARS-CoV-2 infection and worse outcome [25,26,27,28,29]. Contrary to the fears, recent data shows that patients with PSO who receive oral or biologic treatment seem to have similar SARS-CoV-2 infection rates and outcomes as the general population [30,31,32].
The government took drastic measures to control the spread of COVID-19. In Germany, the government introduced restrictions including closing public facilities, educational institutions and boarders to the neighbouring countries. Additionally, contact prohibitions to enforce physical distancing and private quarantine to reduce the risk of infection affected most people in the country [33]. Furthermore, mental health institutions were also seeing patients at limited capacity, many of them shifting their appointments to online-based settings. Stress and mental health burden is also likely to impact the symptoms and the therapeutic efficacy of treatments in PSO [34, 35], therefore potentially explaining the increase of first-line biological and second-line medication sales due to stress-related worsening of the disease. We observed an increase in biologic sales volume across all age groups, indicating that every age group was affected similarly.
During large parts of the pandemic, restrictions were enforced based on infection incident rates, meaning a town or city with high infection rates would have stricter pandemic restrictions compared with low infection rate areas. Specifically, in our period of observation, the state of Schleswig–Holstein had a maximum 7-day-incidence rate of 109.1 per 100,000 inhabitants, whereas Saxony had a maximum 7-day-incidence rate of 504.4 per 100,000 inhabitants. Contrary to our assumption that high infection rates would increase the level of stress and therefore worsen patients’ symptoms, the medication sales only increased in Schleswig–Holstein – the state with lower infection rates. However, this observation is in line with the already discussed observation that about 9% of the patients paused or interrupted PSO treatment due to the pandemic. One explanation could be that due to the high infection rates, practitioners decided against giving their patients immunosuppressants and adapting the treatment plan or the patients themselves decided against changes in medication out of an increased fear of a COVID-19 infection or a worsening of the outcome in case of an infection. Another explanation could be that due to the lockdown restrictions and fear of infection, patients were unwilling to visit doctor’s offices or hospitals, thereby avoiding a change in disease treatment. Ninosu et al. showed that 19.5% of patients in a German university hospital missed an appointment during the pandemic and 62.5% reported missing appointments because of fear of COVID-19 infection [21]
Limitations
Clearly our analysis had some limitations. The active substances we examined are not solely approved for the treatment of PSO, but also for other rheumatological diseases. Additionally, it was not possible to calculate the exact number of syringes or infusions sold, so part of the changes could also be due to changes in pack sizes or to smaller or larger pack sizes being prescribed more frequently.
Conclusion
In summary, our study shows that during the pandemic, despite the proportion of patients who stopped or paused their treatment reported in other studies, there was a significant increase in drug sales for first-line and second-line biologics for all age groups. This shows that despite the pandemic impact, there continues to be an increase in sales volume for biologics.
Only German federal states with intermittently very high COVID-19 incidences show a stagnation in sales volume. The reasons for this need to be investigated in further studies to possibly gain a better understanding of the concerns and uncertainties of patients with PSO.
Data Availability
The data analysed in this work is part of the Permea Data Platform, which is owned by Temedica GmbH, therefore no permission was required. Permea is not a publicly available database, but a Product of Temedica GmbH, which among other data types contains German prescription sales data. It is therefore not possible to send a link for accessing it.
References
Elmas ÖF, Demirbaş A, Kutlu Ö, Bağcıer F, Metin MS, Özyurt K, et al. Psoriasis and COVID-19: a narrative review with treatment considerations. Dermatol Ther. 2020;33: e13858. https://doi.org/10.1111/dth.13858.
Bsteh G, Bitschnau C, Hegen H, Auer M, Di Pauli F, Rommer P, et al. Multiple sclerosis and COVID-19: How many are at risk? Eur J Neurol. 2021;28:3369–74. https://doi.org/10.1111/ene.14555.
Gao Y-D, Ding M, Dong X, Zhang J-J, Kursat Azkur A, Azkur D, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021;76:428–55. https://doi.org/10.1111/all.14657.
Visser MJE, Kell DB, Pretorius E. Bacterial dysbiosis and translocation in psoriasis vulgaris. Front Cell Infect Microbiol. 2019;9:7. https://doi.org/10.3389/fcimb.2019.00007.
Griffiths CEM, Armstrong AW, Gudjonsson JE, Barker JNWN. Psoriasis. Lancet. 2021;397:1301–15. https://doi.org/10.1016/S0140-6736(20)32549-6.
Parisi R, Iskandar IYK, Kontopantelis E, Augustin M, Griffiths CEM, Ashcroft DM, et al. National, regional, and worldwide epidemiology of psoriasis: systematic analysis and modelling study. BMJ. 2020;369: m1590. https://doi.org/10.1136/bmj.m1590.
Augustin M, Glaeske G, Hagenström K. Psoriasis Report - Ergebnisse von Routinedaten-Analysen der Techniker Krankenkasse aus den Jahren 2017–2019 n.d. https://www.tk.de/resource/blob/2105142/fcbbc585441b5652a0e64d7daeaa464b/hautreport-psoriasis-lang-data.pdf
Tokuyama M, Mabuchi T. New treatment addressing the pathogenesis of psoriasis. Int J Mol Sci. 2020;21:E7488. https://doi.org/10.3390/ijms21207488.
Rendon A, Schäkel K. Psoriasis pathogenesis and treatment. Int J Mol Sci. 2019;20:E1475. https://doi.org/10.3390/ijms20061475.
Augustin M, Kiedrowski von R, Körber A, Mrowietz U, Reich K, Thaci D. Verfahrensweise bei der Systemtherapie von Patienten mit Psoriasis während der pandemischen Phase von SARS-CoV-2 (Coronavirus) 2020. https://www.psobest.de/wp-content/uploads/2020/03/RundschreibenPsoBestPsoNetCoronafinal1.0.pdf
Brownstone ND, Thibodeaux QG, Reddy VD, Myers BA, Chan SY, Bhutani T, et al. Novel Coronavirus Disease (COVID-19) and biologic therapy in psoriasis: infection risk and patient counseling in uncertain times. Dermatol Ther (Heidelb). 2020. https://doi.org/10.1007/s13555-020-00377-9.
Yang H, Zheng J. Influence of stress on the development of psoriasis. Clin Exp Dermatol. 2020;45:284–8. https://doi.org/10.1111/ced.14105.
Rousset L, Halioua B. Stress and psoriasis. Int J Dermatol. 2018;57:1165–72. https://doi.org/10.1111/ijd.14032.
Salim S. The stress of the COVID-19 pandemic: beyond the data. Curr Neuropharmacol. 2021;19:1161–3. https://doi.org/10.2174/1570159X19666210311103136.
Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23:741–8. https://doi.org/10.1007/s00737-020-01092-2.
Nast A, Altenburg A, Augustin M, Boehncke W-H, Härle P, Klaus J, et al. Deutsche S3-Leitlinie zur Therapie der Psoriasis vulgaris, adaptiert von EuroGuiDerm - Teil 1: Therapieziele und Therapieempfehlungen. J Dtsch Dermatol Ges. 2021;19:934–51. https://doi.org/10.1111/ddg.14508_g.
Bundesländer | RKI COVID-19 Germany n.d. https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4/page/Bundesl%C3%A4nder/ (accessed Aug 22, 2022).
Schleswig-Holstein - Zahlen zur Bevölkerung. schleswig-holstein.de n.d. https://www.schleswig-holstein.de/DE/landesportal/land-und-leute/zahlen-fakten/bevoelkerung/bevoelkerung_node.html (accessed Aug 22, 2022).
Sachsen SL des F. Bevölkerungsstand - Statistik - Statistik - sachsen.de n.d. https://www.statistik.sachsen.de/html/bevoelkerungsstand-einwohner.html (accessed Aug 22, 2022).
Vanderpuye-Orgle J, Zhao Y, Lu J, Shrestha A, Sexton A, Seabury S, et al. Evaluating the economic burden of psoriasis in the United States. J Am Acad Dermatol. 2015;72:961–7. https://doi.org/10.1016/j.jaad.2015.02.1099. (e5).
Ninosu N, Roehrich F, Diehl K, Peitsch WK, Schaarschmidt M-L. Psoriasis care during the time of COVID-19: real-world data on changes in treatments and appointments from a German university hospital. Eur J Dermatol. 2021;31:183–91. https://doi.org/10.1684/ejd.2021.4016.
Psoriasis drives autoimmune sales growth n.d. https://www.iqvia.com/blogs/2019/03/psoriasis-drives-autoimmune-sales-growth (accessed Aug 23, 2022).
Psoriasis Drugs MArket Research Report n.d. https://www.psmarketresearch.com/market-analysis/psoriasis-drugs-market-outlook.
Corona-Krise: Lieferengpass bei Medikamenten n.d. https://www.ndr.de/ratgeber/gesundheit/Corona-Krise-Lieferengpass-bei-Medikamenten,coronavirus1532.html.
Takeshita J, Shin DB, Ogdie A, Gelfand JM. Risk of serious infection, opportunistic infection, and herpes zoster among patients with Psoriasis in the United Kingdom. J Invest Dermatol. 2018;138:1726–35. https://doi.org/10.1016/j.jid.2018.01.039.
Yeung H, Takeshita J, Mehta NN, Kimmel SE, Ogdie A, Margolis DJ, et al. Psoriasis severity and the prevalence of major medical comorbidity: a population-based study. JAMA Dermatol. 2013;149:1173–9. https://doi.org/10.1001/jamadermatol.2013.5015.
Gelfand JM, Dommasch ED, Shin DB, Azfar RS, Kurd SK, Wang X, et al. The risk of stroke in patients with psoriasis. J Invest Dermatol. 2009;129:2411–8. https://doi.org/10.1038/jid.2009.112.
Ogdie A, Kay McGill N, Shin DB, Takeshita J, Jon Love T, Noe MH, et al. Risk of venous thromboembolism in patients with psoriatic arthritis, psoriasis and rheumatoid arthritis: a general population-based cohort study. Eur Heart J. 2018;39:3608–14. https://doi.org/10.1093/eurheartj/ehx145.
Garshick MS, Tawil M, Barrett TJ, Salud-Gnilo CM, Eppler M, Lee A, et al. Activated platelets induce endothelial cell inflammatory response in psoriasis via COX-1. Arterioscler Thromb Vasc Biol. 2020;40:1340–51. https://doi.org/10.1161/ATVBAHA.119.314008.
Gisondi P, Bellinato F, Chiricozzi A, Girolomoni G. The risk of COVID-19 pandemic in patients with moderate to severe plaque psoriasis receiving systemic treatments. Vaccines (Basel). 2020;8:E728. https://doi.org/10.3390/vaccines8040728.
Talamonti M, Galluzzo M, Chiricozzi A, Quaglino P, Fabbrocini G, Gisondi P, et al. Characteristic of chronic plaque psoriasis patients treated with biologics in Italy during the COVID-19 Pandemic: Risk analysis from the PSO-BIO-COVID observational study. Expert Opin Biol Ther. 2021;21:271–7. https://doi.org/10.1080/14712598.2021.1853698.
Gisondi P, Piaserico S, Naldi L, Dapavo P, Conti A, Malagoli P, et al. Incidence rates of hospitalization and death from COVID-19 in patients with psoriasis receiving biological treatment: a Northern Italy experience. J Allergy Clin Immunol. 2021;147:558-560.e1. https://doi.org/10.1016/j.jaci.2020.10.032.
Bäuerle A, Teufel M, Musche V, Weismüller B, Kohler H, Hetkamp M, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health (Oxf). 2020;42:672–8. https://doi.org/10.1093/pubmed/fdaa106.
Breuer K, Göldner FM, Jäger B, Werfel T, Schmid-Ott G. Chronic stress experience and burnout syndrome have appreciable influence on health-related quality of life in patients with psoriasis. J Eur Acad Dermatol Venereol. 2015;29:1898–904. https://doi.org/10.1111/jdv.12999.
Vardy D, Besser A, Amir M, Gesthalter B, Biton A, Buskila D. Experiences of stigmatization play a role in mediating the impact of disease severity on quality of life in psoriasis patients. Br J Dermatol. 2002;147:736–42. https://doi.org/10.1046/j.1365-2133.2002.04899.x.
Funding
This work and rapid service fee was funded by Temedica GmbH.
Author information
Authors and Affiliations
Contributions
Conceptualization: Maria Kahn, Steffeni Papukchieva, Markus Eberl, Benjamin Friedrich. Methodology: Maria Kahn, Steffeni Papukchieva. Formal analysis: Maria Kahn, Steffeni Papukchieva. Investigation: Maria Kahn, Steffeni Papukchieva. Data curation: Maria Kahn, Steffeni Papukchieva, Markus Eberl. Writing—Original Draft: Maria Kahn, Steffeni Papukchieva, Elizabeth Jacyshyn-Owen, Marina Otten. Writing—review and editing: Stefan Grimm, Markus Eberl, Sebastian Schneeweiss, Marina Otten, Matthias Augustin, Benjamin Friedrich. Visualization: Maria Kahn, Steffeni Papukchieva, Marina Otten.
Corresponding author
Ethics declarations
Conflict of Interest
M.K., S.P., E.J.O., M.E. and B.F. are employed by the Temedica GmbH. M.O. does not have any conflicts of interests to declare. M.A. has served as a consultant, lecturer, researcher, and/or has received research grants from companies manufacturing drugs for chronic skin diseases, including AbbVie, ALK-Abelló, Almirall, Amgen, AOK Bundesverband, AOK BW, Bayer, Beiersdorf, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, BSN, Celgene, Centocor, DAK Gesundheit, Dermira, Desitin, Eli Lilly, Flen,Galderma, Genzyme, GlaxoSmithKline, Hexal, Incyte, Janssen, LEO Pharma, Medac, Menlo, Moelnlycke, MSD, Mylan, Novartis, Pfizer, Regeneron, Sandoz, Sanofi, Stallergenes, Trevi, and Urgo und XenoPort. S.G. has no conflict of interest. S. Schneeweis (ORCID# 0000-0003-2575-467X) is participating in investigator-initiated grants to the Brigham and Women’s Hospital from Boehringer Ingelheim and UCB unrelated to the topic of this study. He is a consultant to Aetion Inc., a software manufacturer of which he owns equity. His interests were declared, reviewed, and approved by the Brigham and Women’s Hospital in accordance with their institutional compliance policies.
Ethical Approval
Ethical approval was not needed for our analysis since the data analysed here retrospectively is anonymized prescription sales data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kahn, M., Papukchieva, S., Jacyshyn-Owen, E. et al. The IMPACT of the COVID-19 Pandemic on Prescription Drug Use in Patients with Psoriasis Vulgaris in Germany. Dermatol Ther (Heidelb) 13, 2609–2620 (2023). https://doi.org/10.1007/s13555-023-01023-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-023-01023-w