Abstract
Background and Objectives
Desidustat is a novel prolyl hydroxylase domain (PHD) inhibitor for the treatment of anemia. The objective of this study was to investigate the pharmacokinetics and drug–drug interaction properties of desidustat using in vitro and in vivo nonclinical models.
Methods
In vitro, Caco2 cell permeability, plasma protein binding, metabolism, cytochrome P450 (CYP) inhibition, and CYP induction were examined. In vivo, pharmacokinetic studies of oral bioavailability in mice, rats, dogs and monkeys, dose linearity, tissue distribution, and excretion in rats were conducted.
Results
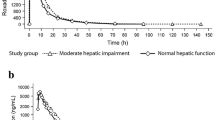
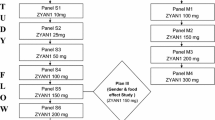
In Caco-2 cells, the apparent permeability of desidustat was high at low pH and low at neutral pH. The oral bioavailability (%F) of desidustat was 43–100% with a median time to reach peak concentration (Tmax) of about 0.25–1.3 h across species. Desidustat displayed a low mean plasma clearance (CL) of 1.3–4.1 mL/min/kg (approximately 1.8–7.4% of hepatic blood flow), and the mean steady-state volume of distribution (Vss) was 0.2–0.4 L/kg (approximately 30–61% of the total body water). Desidustat showed a dose-dependent increase in exposures over the 15–100 mg/kg dose range. It was rapidly distributed in various tissues, with the highest tissue-to-blood ratio in the liver (1.8) and kidney (1.7). Desidustat showed high plasma protein binding and was metabolically stable in human liver microsomes, hepatocytes, and recombinant CYPs. It did not show significant inhibition of major drug-metabolizing CYP enzymes (IC50 > 300 µM) or the potential to induce CYP1A2 and CYP3A4/5 (up to 100 µM) in HepG2 cells. It may have minimal potential of clinical drug–drug interaction when used in combination with iron supplements or phosphate binders. Desidustat was primarily excreted unchanged in urine (25% of the oral dose) and bile (25% of the oral dose) in rats. The mean elimination half-life of desidustat ranged from 1.0 to 5.3 h and 1.3 to 5.7 h across species after intravenous and oral administration, respectively.
Conclusion
Taken together, desidustat is well absorbed orally. It showed a dose-dependent increase in exposure, did not accumulate in tissue, and was eliminated via dual routes. It is metabolically stable, has minimal potential to cause clinical drug–drug interactions (DDIs), and demonstrates discriminable pharmacokinetic properties for the treatment of anemia.






Similar content being viewed by others
References
Campbell K. Anaemia: causes and treatment. Nurs Times. 2003;99(43):30–3.
Madu AJ, Ughasoro MD. Anaemia of chronic disease: an in-depth review. Med Princ Pract. 2017;26(1):1–9.
Le CH. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003–2012). PLoS One. 2016;11(11):e0166635.
Bonomini M, Del Vecchio L, Sirolli V, Locatelli F. New treatment approaches for the anemia of CKD. Am J Kidney Dis. 2016;67(1):133–42.
Santhanam AV, d’Uscio LV, Katusic ZS. Cardiovascular effects of erythropoietin: an update. Adv Pharmacol. 2010;1(60):257–85.
Bailey CK, Caltabiano S, Cobitz AR, Huang C, Mahar KM, Patel VV. A randomized, 29-day, dose-ranging, efficacy and safety study of daprodustat, administered three times weekly in patients with anemia on hemodialysis. BMC Nephrol. 2019;20(1):1–2.
Jain MR, Joharapurkar AA, Pandya V, Patel V, Joshi J, Kshirsagar S, Patel K, Patel PR, Desai RC. Pharmacological characterization of ZYAN1, a novel prolyl hydroxylase inhibitor for the treatment of anemia. Drug Res. 2016;66(02):107–12.
Joharapurkar AA, Pandya VB, Patel VJ, Desai RC, Jain MR. Prolyl hydroxylase inhibitors: a breakthrough in the therapy of anemia associated with chronic diseases. J Med Chem. 2018;61(16):6964–82.
Muchnik E, Kaplan J. HIF prolyl hydroxylase inhibitors for anemia. Expert Opin Investig Drugs. 2011;20(5):645–56.
López-Gómez JM, Abad S, Vega A. New expectations in the treatment of anemia in chronic kidney disease. Nefrología (English Edition). 2016;36(3):232–6.
Martin ER, Smith MT, Maroni BJ, Zuraw QC, deGoma EM. A clinical trial of vadadustat in patients with anemia secondary to stage 3 or 4 chronic kidney disease. Am J Nephrol. 2017;45(5):380–8.
Provenzano R, Besarab A, Sun CH, Diamond SA, Durham JH, Cangiano JL, Aiello JR, Novak JE, Lee T, Leong R, Roberts BK. Oral hypoxia-inducible factor prolyl hydroxylase inhibitor roxadustat (FG-4592) for the treatment of anemia in patients with CKD. Clin J Am Soc Nephrol. 2016;11(6):982–91.
Yamamoto H, Taguchi M, Matsuda Y, Iekushi K, Yamada T, Akizawa T. Molidustat for the treatment of renal anaemia in patients with non-dialysis-dependent chronic kidney disease: design and rationale of two phase III studies. BMJ Open. 2019;9(6):e026704.
Lentini S, Kaiser A, Kapsa S, Matsuno K, van der Mey D. Effects of oral iron and calcium supplement on the pharmacokinetics and pharmacodynamics of molidustat: an oral HIF–PH inhibitor for the treatment of renal anaemia. Eur J Clin Pharmacol. 2020;76(2):185–97.
Negri AL, Ureña Torres PA. Iron-based phosphate binders: do they offer advantages over currently available phosphate binders? Clin Kidney J. 2015;8(2):161–7.
Jain M, Joharapurkar A, Patel V, Kshirsagar S, Sutariya B, Patel M, Patel H, Patel PR. Pharmacological inhibition of prolyl hydroxylase protects against inflammation-induced anemia via efficient erythropoiesis and hepcidin downregulation. Eur J Pharmacol. 2019;15(843):113–20.
Patel H, Joharapurkar AA, Pandya VB, Patel VJ, Kshirsagar SG, Patel P, Gevriya B, Jain MR, Srinivas NR, Patel PR, Desai RC. Influence of acute and chronic kidney failure in rats on the disposition and pharmacokinetics of ZYAN1, a novel prolyl hydroxylase inhibitor, for the treatment of chronic kidney disease-induced anemia. Xenobiotica. 2018;48(1):37–44.
Kansagra KA, Parmar D, Jani RH, Srinivas NR, Lickliter J, Patel HV, Parikh DP, Heading H, Patel HB, Gupta RJ, Shah CY. Phase I clinical study of ZYAN1, a novel prolyl-hydroxylase (PHD) inhibitor to evaluate the safety, tolerability and pharmacokinetics following oral administration in healthy volunteers. Clin Pharmacokinet. 2018;57(1):87–102.
Parmar DV, Kansagra KA, Patel JC, Joshi SN, Sharma NS, Shelat AD, Patel NB, Nakrani VB, Shaikh FA, Patel HV, ZYAN1 Trial Investigators. Outcomes of desidustat treatment in people with anemia and chronic kidney disease: a phase 2 study. Am J Nephrol. 2019;49(6):470–8.
Gad SC, Spainhour CB, Shoemake C, Pallman DR, Stricker-Krongrad A, Downing PA, Seals RE, Eagle LA, Polhamus K, Daly J. Tolerable levels of nonclinical vehicles and formulations used in studies by multiple routes in multiple species with notes on methods to improve utility. Int J Toxicol. 2016;35(2):95–178.
Strickley RG. Formulation in drug discovery. Annu Rep Med Chem. 2008;1(43):419–51.
Kumar KK, Karnati S, Reddy MB, Chandramouli R. Caco-2 cell lines in drug discovery—an updated perspective. J Basic Clin Pharm. 2010;1(2):63.
Kis O, Walmsley SL, Bendayan R. In vitro and in situ evaluation of pH-dependence of atazanavir intestinal permeability and interactions with acid-reducing agents. Pharm Res. 2014;31(9):2404–19.
Hirota K. HIF-α prolyl hydroxylase inhibitors and their implications for biomedicine: a comprehensive review. Biomedicines. 2021;9(5):46825.
Prescribing information: Everenzo; https://www.ema.europa.eu/en/documents/product-information/evrenzo-epar-product-information_en.pdf .
Acknowledgements
The authors would like to acknowledge the support received for the in-life study phase and the proficient analytical work of Hardik Soni, Shreesha Sukumaran, Bharat Patel, Janmay Shah, Nirmal Patel, Laxmikant Gupta, and Sanjay Singh. We are also thankful to Vanita Khatri for the critical review of all scientific data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research work was funded by Zydus Lifesciences Limited (ZLL).
Ethics Approval
The experiments on animals have been performed as per applicable ethical guidance. The procedures on mice (ZRC/DMPK/BP/005/07-2K13) and rats (ZRC/DMPK/BP/003/03-2K13) were approved by the Institutional Animal Ethics Committee (IAEC) of the Zydus Research Centre, Zydus Lifesciences Limited, Ahmedabad, India, and protocols for dog (ZRC/DMPK/NP/008/03-2K13) and monkey (ZRC/PRF/NP/015/12-2K12) were approved by the committee for the purpose of control and supervision of experiments on animals (CPCSEA), Government of India.
Conflict of Interest
All the authors are employees of Zydus Lifesciences Limited and have no conflicts of interest in the content of the research work (ZRC communication number 670).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Data Availability Statement
Data supporting the findings are available from the corresponding author upon request.
Code Availability
The proprietary software program Phoenix WinNonlin and GraphPad Prism was used for the data calculation and analysis reported here.
Author Contributions
Participated in research design, manuscript writing, and interpretation of the data: H.P., P.G., P.P., V.P., R.C., and M.J.; conducted experiments and data analysis: N.M., J.C., P.P., and H.P.
Rights and permissions
About this article
Cite this article
Patel, H., Modi, N., Chaudhari, J. et al. Nonclinical Pharmacokinetic Evaluation of Desidustat: a Novel Prolyl Hydroxylase Inhibitor for the Treatment of Anemia. Eur J Drug Metab Pharmacokinet 47, 725–740 (2022). https://doi.org/10.1007/s13318-022-00788-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-022-00788-3