Abstract
Introduction
This study developed a simple algorithm based on clinical results described in medical literature and which allows one to simplify complex insulin regimes with IdegLira to avoid adverse events related to the complexity of some insulin treatments.
Methods
We conducted a systematic review of the literature that allowed us to identify studies that evaluated the clinical result of simplifying complex insulin regimes. The authors reviewed the common factors these simpler regimes had, including the type of patients who used them.
Results
We found nine clinical studies published between 2017 and 2022, eight performed in Europe and one in Latin America. The monitoring time of the studies ranged between 3 and 18 months. The size of the study populations was between 61 and 611 patients (the latter was in five countries). In all studies, HbA1c decreased by 0.6–1.7% and the weight decreased by 0.1–3.11 kg.
Conclusions
On the basis of the findings of these studies, we made some recommendations for clinical practice to simplify treatment. The results of these studies support an algorithm that simplifies the treatment of complex insulin regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Simplifying complex treatment regimens in patients with type 2 diabetes mellitus (T2DM) improves treatment adherence and clinical outcomes while reducing the risk of adverse events and healthcare costs. |
Multiple clinical practice guidelines exist for T2DM treatment, but they often do not address the challenges of simplifying therapy in patients who have achieved therapeutic objectives but experience adverse events. |
The authors conducted a literature review to evaluate the evidence and propose a strategy to simplify complex antidiabetic treatments in patients with T2DM. |
Patient selection criteria for simplified treatment regimens may include assessing beta cell reserve and considering insulin doses to achieve reasonable metabolic control without compromising glycemic outcomes. |
Introduction
Evidence pointing to the need to simplify complex treatment regimens in patients with type 2 diabetes mellitus (T2DM) has increased recently [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15]. This practice reduces the risk of adverse events, such as hypoglycemia, increases treatment adherence, and improves clinical results. The accumulated evidence of the available antidiabetic drugs makes it possible to guide the treatment of patients with T2DM on the basis of the potential benefits and risks of each group of drugs. We have observed that more straightforward treatment strategies are needed, which are helpful for health professionals who care for patients with T2DM and prescribe multiple antidiabetic medications due to the treatment inertia [16].
More complex treatments in patients with T2DM increase healthcare costs since they will need significantly more diagnostic tests to monitor clinical results and avoid adverse events [17, 18]. Therefore, if it is possible to return the patient with T2DM to primary healthcare caregivers, not only will greater comfort be obtained for the patient but it will also increase the efficiency of the health system by achieving similar results with lower costs [19, 20].
Multiple clinical practice guidelines (CPG) have been published [21,22,23,24,25,26] with different treatment strategies based on the best published evidence, which recommends the staggering use of antidiabetics to the extent that patients do not achieve the expected results. These kinds of CPGs are most valuable because they allow the rational use of medications but they lead to therapeutic inertia when adding drugs or increasing the frequency of their doses [27]. These CPGs allow for achieving therapeutic objectives. However, reaching this goal with complex treatments increases the risk of developing adverse events and decreases adherence to treatment. Furthermore, the guidelines do not usually address the clinical situation of how to treat the patient who has achieved the therapeutic objective but who, as a result of the complexity of the treatment, presents adverse events, especially hypoglycemia.
Simplifying the complex treatments received by patients with T2DM is a challenge doctors face when the patient has already achieved the proposed therapeutic objective. Therefore, these recommendations aim to present a simplification strategy for complex antidiabetic treatments by reviewing the available evidence and establishing arguments supporting the safest way to offer simpler regimens while maintaining the desired therapeutic objectives.
Methods
Literature Review
We designed a high-sensitivity search strategy to identify all possible articles of interest and filter them in the review. We search reviews and clinical trials in the MEDLINE, Embase, and CINAHL databases without limits on dates. The only search terms used were simplifying AND insulin, and the only search filter used was human species.
Article inclusion criteria were as follows: (1) randomized controlled trials, including open-label studies, (2) single-arm clinical trials, (3) observational studies with real-world evidence (RWE), both prospective and retrospective; and (4) revisions. In addition, two reviewers (medical epidemiologists) determined the eligibility status of each article identified by the search strategy.
Evaluation of the Evidence
The methodological evaluation of each article included in the review was carried out independently by two medical epidemiologists (JEO, Arlex Uriel Palacios (AUP)). We used the Consolidated Standards of Reporting Trials (CONSORT) [28] to evaluate randomized clinical trials, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement [29] to assess observational studies, and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [30] for systematic reviews. We discussed our assessment discrepancies in a meeting, and when we did not have a consensus, a third reviewer resolved any disagreement.
Although these instruments did not assess the methodological quality of the studies, they did make it possible to determine the risk of bias that the publications may have. We did not include articles with a high risk of bias because they did not fulfill several items proposed in the aforementioned evaluation guides. We sent selected papers to all authors who participated in this review, and we them to suggest any articles they felt were missing.
Characteristics of the Evidence
The articles selected for this consensus differ in the populations included, in the inclusion criteria, or the simplification strategies used, among others. That is the main challenge of this review, generating consensus recommendations in the different clinical scenarios described in the literature. The authors do not intend for these recommendations to be a definitive analysis of the evidence but rather a starting point from which continuous improvement is made on the basis of the clinical results that patients obtain from these recommendations (Table 1).
Definitions
Overtreatment
The Institute of Medicine defines overtreatment as treatment use even when the potential harms outweigh the possible benefits [31]. Its prevalence in older adults with T2DM is between 21% and 60.5% [32, 33]. The line that separates reasonable metabolic control in T2DM from overtreatment is usually very narrow [31]. There should be a special mention of patients who use insulin. These patients have the potential damage of excessive therapy, leading to a higher risk of severe hypoglycemia, weight gain, possible mortality, lower quality of life, and less adherence to treatment, especially in those on multiple-dose insulin (MDI) therapy [34]. Basal insulin overtreatment is called overbasalization and occurs when patients receive a dose > 0.5 IU/kg/day and have an HbA1c outside the target, recalling the ceiling effect of basal insulin [35]. Four of ten patients with T2DM using basal insulin have overbasalization [36].
Simplification
Simplification refers to the reduction in the complexity of a therapeutic regimen, including a lower number of administrations, a lower requirement for glucose measurement, or a reduction in the need for prandial insulin calculations about carbohydrate intake of a meal. In insulin-using patients, the term simplification includes any strategy that reduces the burden of complex insulin therapy, including lowering the insulin dose or the number of injections (especially prandial insulin) [34]. There is a direct correlation between simple treatment schemes and greater adherence by the patient [37], as well as between compliance and reasonable metabolic control [38]. Additionally, some evidence suggests that simplification in patients with complex insulin regimens is associated with equal or better metabolic control, less weight gain, and reduced hypoglycemia [1, 5].
Clinical Inertia
Clinical inertia is the failure of health personnel to initiate or intensify therapy when indicated. Clinical inertia comprises clinician-related factors (e.g., lack of time in care, lack of skills and confidence), patient characteristics (poor disease awareness, poor habits, fear of adverse events), and factors relating to the health system (poor communication in the care team, absence of management guidelines, or problems in the processing and delivery of medications) [39]. For example, a study in the UK that included 3185 patients treated with basal insulin with or without oral antidiabetics treated in primary care found almost 60% clinical inertia during 3 years of follow-up [40].
Reverse Clinical Inertia
Reverse clinical inertia is the lack of initiative or inability to reduce or suspend a therapy when it is no longer necessary [34]; in other words, it is the passive attitude of health personnel toward a patient with overtreatment. Contributing factors to reverse clinical inertia include the overscrupulous following of therapeutic guidelines and a lack of perception of the patient’s frailty [39]. The American College of Physicians recommends de-intensifying pharmacologic therapy in patients with HbA1c < 6.5%. Simplification is necessary to avoid the risk of hypoglycemia and polypharmacy, especially in the elderly population with complex insulin regimens [34].
Patient Selection
Beta Cell Reserve
Fixed combinations of glucagon-like peptide 1 receptor agonists (GLP-1 RAs) are only approved to use in people with T2DM use. GLP-1 RAs modulate insulin release from the pancreas, so their addition to treating people with type 1 diabetes mellitus (T1DM) results in only modest reductions in HbA1c [41]. Additionally, beta cell function declines over time in people with T2DM, and it is not uncommon to add fixed combinations such as insulin degludec/liraglutide (IdegLira) in people long after diagnosis of the disease [42]. As a result, some authors have suggested different methods to identify potential patient users of a fixed combination, those without T1DM or with beta cell reserve.
Measurement of C-peptide is a widely used method to estimate beta cell function. It is a proinsulin cleavage product and is therefore produced equimolarly to insulin. However, it has a slower degradation rate and a limited, predictable metabolism after passage through the liver, making it a better predictor than insulin. On the other hand, the detection capacity of current measurement methods allows for detecting concentrations up to 500 times lower than basal concentrations in healthy individuals [43]. We can measure C-peptide after an 8–10-h fast, randomly without fasting, or stimulated by various methods. However, the recommended way to assess beta cell function is C-peptide measurement enabled either by glucagon or a mixed meal test [44].
A random C-peptide measurement of less than 0.6 ng/mL (conversion units 1 nmol/L = 1 pmol/mL = 1000 pmol/L = 3 ng/mL) has a sensitivity of 100%, a specificity of 93%, and an area under the receptor operating characteristic (ROC) curve of 0.99 to detect severe insulin insufficiency [45,46,47]. On the other hand, a fasting C-peptide concentration of less than 0.96 ng/mL has proven helpful in differentiating between T2DM and T1DM in insulin-treated individuals [46]. Finally, some studies associate fasting C-peptide concentrations less than 0.96 ng/mL with a poor reduction in HbA1c response in patients treated with GLP-1 RAs [47].
The DUAL V [48] and DUAL VII [49] clinical trials did not use the beta cell reserve as an inclusion criterion. However, they did have exclusion criteria to withdraw participants if they had persistent fasting hyperglycemia. Two studies report using C-peptide as a criterion to decide the initiation of IdegLira therapy. In a single-arm clinical trial under standard clinical practice conditions, one inclusion criterion that participants had to have a randomly measured C-peptide greater than 1.1 ng/mL [5]. On the other hand, a single-cohort follow-up study evaluating the effect of switching from a multiple-dose insulin regimen to IdegLira included patients with a C-peptide measurement greater than 1 ng/mL; the authors did not specify whether the measure was randomized or after fasting. Finally, in a clinical trial conducted in Japan in patients treated with MDI, the authors randomized the patients to continue with their treatment schedule or to receive a combination of lixisenatide and insulin glargine; patients with a fasting C-peptide less than 0.5 ng/mL were excluded [4].
The effect observed with the medication in reducing blood glucose, hyperglycemic events, or hyperglycemic crises does not seem to differ between the studies that report some estimates of C-peptide as an inclusion criterion and those that do not.
The authors recommend that a fasting C-peptide measurement could be a valuable aid to the clinician when deciding to replace an MDI regimen with IdegLira, especially in those with a long-standing diagnosis of T2DM or with clinical features that suggest a different type of diabetes. We made this recommendation considering that C-peptide measurement is the method the American Diabetes Association recommended to assess beta cell function. In the same way, we can measure fasting or random C-peptide reliably and quickly. So, a fasting C-peptide value of less than 1 ng/mL is helpful to discriminate people treated with insulin with T1DM from those with T2DM. This value also correlates with a poor glycemic response to treatment with liraglutide. However, the results of multiple real-life studies that have reported IdegLira treatment in people treated with MDIs and have not included a C-peptide measurement suggest that this measurement is not always necessary. That is, it should fit the clinical criteria.
Insulin Dose
Simplifying IdegLira treatment for patients receiving MDIs implies a reduction in insulin dose at initiation and, as a result of the insulin dose limit with combination therapy, will also mean a lower final amount in some treated patients with high doses of insulin. This situation may concern clinicians because of the fear of poor glycemic control during the transition period or the impossibility of achieving reasonable metabolic control at the end of the IdegLira titration. However, patients treated with insulin in DUAL VII [49] and DUAL VIII [50] trials only had the basal component; these clinical trials do not fully answer this question.
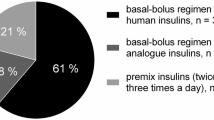
Multiple observational studies and those carried out in routine clinical practice, as well as a clinical trial, have addressed the situation of simplification from an MDI scheme. The BEYOND clinical trial [12] evaluated the effect of simplification from an MDI regimen. One of its arms included fixed combinations of GLP-1 RAs. Inclusion criteria did not include insulin or exclusion of a maximum dose of insulin before inclusion in the study. The average insulin daily dose (IDD) of the group assigned to the fixed combination was 0.59 units/kg/day.
One clinical trial without a control group defined an inclusion criterion for a “low” daily insulin dose as an IDD of less than 70 units/day or 0.6 units/kg/day. However, patients who had experienced multiple hypoglycemia episodes were allowed an IDD between 0.6 and 0.8 units/kg/day without exceeding 70 units/day. The mean IDD at the beginning of the study was 0.47 ± 0.13 units/kg/day. Finally, an observational study reported the results of the follow-up of patients in whom the simplification was made on the basis of an institutional protocol. In this previous study, the patients with an IDD greater than 50 units had a transition phase that added a second dose of long-acting insulin during the IdegLira titration; the average initial insulin dose was 0.57 units/kg/day [2].
The DUAL VII clinical trial [49] demonstrated that escalation from a basal insulin regimen to a fixed-combination regimen is effective and safe. Four weeks after starting therapy, the difference in fasting glucose was 11.16 mg/dL (95% CI 5.04–17.5) lower in the IdegLira group, highlighting that hyperglycemia should not be a concern with proper drug titration. In the treatment simplification of the BEYOND trial, simplification was performed without fear in patients with an IDD close to 0.6 units/kg/day. Studies conducted under usual clinical practice conditions have used strategies such as establishing a limit on the IDD at which a patient is not a candidate for treatment or transition phases with an additional insulin dose. This group considers that the current evidence is insufficient to recommend an IDD from which not to feel a patient is a candidate for therapy. However, the authors believe that an IDD of 0.6 units/kg/day is a sensible cutoff point to consider differential approaches to simplification, as proposed in the algorithm (Fig. 1).
Initial Dose
In the DUAL series of clinical trials, the initial dose of formulation with IdegLira is estimated on the basis of previous antidiabetic treatment. It means that are two scenarios: if the patient is taking oral antidiabetics, the initial amount will be 10 units, and if the patient is being treated with GLP-1 RAs or with basal insulin (BI), the initial dose will be 16 units [48,49,50,51]. This scheme has two pathways. The first is the initial dose of GLP-1 RAs (liraglutide), given the basal doses tested in clinical trials with monocomponent [52], which start with 0.6 mg/day. The second one, the initial amounts of the second-generation insulin analogue (insulin degludec), is also based on the titration algorithms previously explored as a monocomponent [53,54,55,56]. Given this context, it is intuitive to contemplate finding similar scenarios in RWE studies.
In the scenario that concerns this review (ongoing basal insulin or MDI), the authors found a basal starting dose of 16 units in different clinical studies [5, 7, 12,13,14]. In a study in Colombia, the authors specified the initial amount, but they followed the titration processes of the DUAL trials; that is, it is implicit that the initial dose was 16 units [42]. On the other hand, the REX study group describes initial amounts of 20 units with an interquartile range of 16–20 units [52], and Sofra [2] reports initial doses of 20 units. No study reported a starting amount of 10 units if the patient came from BI or MDI.
Studies such as the one published by the EXTRA study group with results from five European countries (Germany, Switzerland, the UK, Austria, and Sweden) propose broader ranges [3]. They started with initial doses from 10 units to more than 50 units per day. The average initial amount from oral antidiabetics was 17.2 units. If the patient came with GLP-1 RAs with or without oral antidiabetics, the average dose was 16.8 units. On the other hand, if, before the study, the patients received insulin + GLP-1 RAs with or without oral antidiabetics, the mean dose was 30.9 units. If they only had BI with or without oral antidiabetic drugs, it was 20 units. Finally, if they received MDI with or without oral antidiabetic drugs, the average dose was 21.2 units. Likewise, Di Loreto et al. [7] describe a mean amount of 16.2 units (SD 2.2) if patients were receiving BIs and oral antidiabetics; if they received GLP-1 RAs, the dose was 27 units (SD 12.2), and if they were receiving MDI treatment, the amount was 17 units (SD 4.3).
On the basis of the above and the literature review results, the authors recommend starting a dose of 20 units of IdegLira in patients receiving GLP-1 RAs with or without BIs with or without oral antidiabetics. Likewise, suppose patients receive BIs with or without oral antidiabetics or MDI with or without oral antidiabetics. In that case, the initial dose will be 16 units of IdegLira, insisting on the importance of dose titration as a fundamental strategy to achieve individualized therapeutic goals.
Titration
Regarding the titration component, the studies tended toward homogeneity. For example, five studies of RWE [5, 7, 12,13,14] recommend carrying out a titration as per the essential studies of IdegLira in the DUAL program [48], i.e., twice a week (every 3 days) with an average of three consecutive days and increments of 2 units per time [5, 7, 12,13,14, 42]. On the other hand, three studies do not specify the titration scheme. However, discussion items state that the manufacturer’s suggestions were followed [3, 7, 57], and only one study reports titration once a week [2]. On the basis of this argument, the authors recommend that the titration scheme for the therapeutic simplification process be twice a week (every 3 days), with an average of three consecutive days and increments of 2 units per time.
Goals
The basal glucose goal to guide the titration proposed in the DUAL study program is 72–90 mg/dL [48]. The argument for such a strict objective is to seek better metabolic control with the safety offered by a second-generation insulin analogue such as degludec insulin. The results of monocomponent studies are convincing compared to those of a first-generation insulin analogue [53,54,55,56]; however, the real-life clinical landscape includes other considerations, which is why different studies have considerable heterogeneity.
Three studies included in this review do not specify the basal glucose goal [3, 12, 57]; however, in different sections, they argue that the treating clinician had the power to individualize the goal. On the other hand, only one study indicates that its goal is the same as that of the DUAL series of clinical trials, i.e., 72–90 mg/dL [14]. Taybani et al. set a goal of 5–6 mmol/L, corresponding to 90–108 mg/dL [5]; any other study does not assume this goal. Sofra adheres to the goals of the European Association for the Study of Diabetes, which, when publishing these recommendations, are consistent with those of the American Diabetes Association in 2022, i.e., 80–130 mg/dL [2]. An Italian study sets two goals, a common goal between 90 and 130 mg/dL and another of 130–160 mg/dL in “frail elderly.” However, this last term has no definition in the text since the choice of one or the other goal was made only on clinical grounds [13]. Ramírez-Rincón et al. did not have a single standard goal orientation. Given that in this study, every physician assumed their criteria, some patients were oriented on the basis of the goal established in the DUAL clinical trials (72–90 mg/dL), while others attempted to meet the ADA goal (80–130 mg/dL).
When performing a specific search in the population over 65, insulin simplification schemes set goals as lax as 90–150 mg/dL [1], an essential element to consider. Thus, the authors recommend that the treating clinician be the one to make a personalized decision according to the age and the specific clinical and social conditions of each patient, taking as a reference framework one of the following options:
-
Fasting blood glucose between 80 and 130 mg/dL [58]
-
Fasting blood glucose between 90 and 150 in older adults [1]
Although the REX [57] and Di Loreto [7] studies did not report transition schedules, we have included them in this review for the following reasons. The REX study says that the authors chose the therapy as a simplification strategy in two-thirds of the patients, which is why we have included it. In the study by Di Loreto et al. [7], the authors included outcomes due to changing therapy. Although both studies do not indicate how the change was made, the authors consider that the clinical results reported by both studies should not be ruled out, so we have included them in our review.
Limitations
The main limitation of this study is the heterogeneity of the types of studies included in this review. The authors know it is difficult to form conclusions from different studies, with varying observation periods and sometimes various outcome measures. Not many studies have evaluated the clinical results of the simplification of insulin treatment with IdegLira, so the challenge for the study was how these results could support a simplification process. Table 1 of the study presents the summary of the main clinical characteristics of each of the studies, as well as their clinical results so that the reader can identify the differences between the studies, which, in turn, allow supporting the treatment simplification process such as IdegLira as a strategy that makes it easier for the patient to achieve their treatment goals.
Conclusion
The purpose of this review is to propose a simplification scheme based on the available evidence from IdegLira. The chronic and progressive nature of diabetes gradually increases the complexity of therapeutic strategies, which aim to achieve specific goals. Unfortunately, this process is accompanied by greater patient demand, negatively impacting their quality of life. That is why implementing strategies that simplify treatment has the potential to be very important. Therefore, we carried out a literature review to contribute to constructing a scheme that meets this objective. Besides, we describe some definitions, pathophysiological principles, and technical scrutiny of the real-life studies’ specifications. In this order, we propose simplifying complex insulinization regimens with IDegLira in patients living with T2D, with elements of a logical sequence to promote the construction of an algorithm. Thus, constructing the process in question allows us to visualize the co-formulation with IDegLira for simplification as a simple, versatile, safe, and effective therapeutic tool.
Data Availability
The author took the data to build this article from secondary sources referenced in the manuscript.
References
Munshi MN, Slyne C, Segal AR, Saul N, Lyons C, Weinger K. Simplification of insulin regimen in older adults and risk of hypoglycemia. JAMA Intern Med. 2016;176(7):1023–5.
Sofra D. Glycemic control in a real-life setting in patients with type 2 diabetes treated with IDegLira at a single Swiss center. Diabetes Ther. 2017;8(2):377–84.
Price H, Blüher M, Prager R, et al. Use and effectiveness of a fixed-ratio combination of insulin degludec/liraglutide (IDegLira) in a real-world population with type 2 diabetes: results from a European, multicentre, retrospective chart review study. Diabetes Obes Metab. 2018;20(4):954–62.
Miya A, Nakamura A, Miyoshi H, et al. Satisfaction of switching to combination therapy with lixisenatide and basal insulin in patients with type 2 diabetes receiving multiple daily insulin injection therapy: a randomized controlled trial. J Diabetes Investig. 2018;9(1):119–26.
Taybani Z, Bótyik B, Katkó M, Gyimesi A, Várkonyi T. Simplifying complex insulin regimens while preserving good glycemic control in type 2 diabetes. Diabetes Ther. 2019;10(5):1869–78.
Birmingham, Solihull, Sandwell, Environs Area Prescribing Committee (APC), and Diabetes Medicines Management Advisory Group (DMMAG). NHS. Type 2 diabetes mellitus. Guideline for the choice of oral and non-insulin antihyperglycaemic agents in adults. www.birminghamandsolihullccg.nhs.uk/about-us/publications/policies/2674-antidiabetics-therapy-guideline-for-type-2-diabetes/file Accessed July 2022.
Di Loreto C, Celleno R, Piastrella L, Del Sindaco P. IDegLira fixed-ratio combination in the real world: a retrospective observational single-center Italian experience. Eur Rev Med Pharmacol Sci. 2020;24(20):10671–9.
Harris S, Abrahamson MJ, Ceriello A, et al. Clinical considerations when initiating and titrating insulin degludec/liraglutide (IDegLira) in people with type 2 diabetes. Drugs. 2020;80(2):147–65.
Rosenstock J, Nino A, Soffer J, et al. Impact of a weekly glucagon-like peptide 1 receptor agonist, albiglutide, on glycemic control and on reducing prandial insulin use in type 2 diabetes inadequately controlled on multiple insulin therapy: a randomized trial. Diabetes Care. 2020;43(10):2509–18.
Abid S, Abdulhamid F. Importance of de-escalating antidiabetic medication to prevent hypoglycaemia. Diabetes Metab Syndr. 2020;14(6):2079.
Naing S, Ramesh G, Garcha J, Poliyedath A, Khandelwal S, Mills PK. Is the stepping-down approach a better option than multiple daily injections in obese patients with poorly controlled type 2 diabetes on advanced insulin therapy? Endocrinol Diabetes Metab. 2020;4(2):e00204.
Giugliano D, Longo M, Caruso P, et al. Feasibility of simplification from a basal-bolus insulin regimen to a fixed-ratio formulation of basal insulin plus a GLP-1RA or to basal insulin plus an SGLT2 inhibitor: BEYOND, a randomized. Pragmatic Trial Diabetes Care. 2021;44(6):1353–60.
Persano M, Nollino L, Sambataro M, et al. Real-world study on the effectiveness and safety of basal insulin IDegLira in type 2 diabetic patients previously treated with multi-injective insulin therapy. Eur Rev Med Pharmacol Sci. 2021;25(2):923–31.
Zenari L, Da Porto A, De Moliner L, et al. Real-world evaluation of glycemic outcomes and extra-glycemic parameters in diabetic patients treated with the combined formulation degludec-liraglutide (Ideglira). Diabetes Ther. 2021;12(1):197–209.
Boggild MK, Cheung AM. Basal insulin plus GLP-1 RA or SGLT2 inhibitor was noninferior to basal-bolus insulin intensification for HbA1c n T2DM. Ann Intern Med. 2021;174(9):JC106.
Böhm AK, Schneider U, Aberle J, Stargardt T. Regimen simplification and medication adherence: fixed-dose versus loose-dose combination therapy for type 2 diabetes. PLoS ONE. 2021;16(5):e0250993.
Sancho-Mestre C, Vivas-Consuelo D, Alvis-Estrada L, et al. Pharmaceutical cost and multimorbidity with type 2 diabetes mellitus using electronic health record data. BMC Health Serv Res. 2016;16(1):394.
Weng W, Liang Y, Kimball ES, et al. Drug usage patterns and treatment costs in newly-diagnosed type 2 diabetes mellitus cases, 2007 vs 2012: findings from a large US healthcare claims database analysis. J Med Econ. 2016;19(7):655–62.
Cannon AJ, Bargiota A, Billings L, et al. Evaluation of the short-term cost-effectiveness of IDegLira versus basal insulin and basal-bolus therapy in patients with type 2 diabetes based on attainment of clinically relevant treatment targets. J Manag Care Spec Pharm. 2020;26(2):143–53.
Raya PM, Blasco FJA, Hunt B, et al. Evaluating the long-term cost-effectiveness of fixed-ratio combination insulin degludec/liraglutide (IDegLira) for type 2 diabetes in Spain based on real-world clinical evidence. Diabetes Obes Metab. 2019;21(6):1349–56.
American Diabetes Association Professional Practice Committee, Draznin B, Aroda VR, et al. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S125–43.
Buse JB, Wexler DJ, Tsapas A, et al. 2019 update to: management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2020;63(2):221–8 (Erratum in Diabetologia. 2020 Aug;63(8):1667).
Diabetes Canada Clinical Practice Guidelines Expert Committeee, Lipscombe L, Butalia S, et al. Pharmacologic glycemic management of type 2 diabetes in adults: 2020 UPDATE. Can J Diabetes. 2020;44(7):575–91.
Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. Diabetol Int. 2020;11(3):165–223.
The Royal Australian College of General Practitioners. Management of type 2 diabetes: a handbook for general practice. East Melbourne, Vic: RACGP, 2020.
Ministerio de Salud y Protección Social, departamento administrativo de Ciencia, tecnología e innovación – Colciencias. Guía de práctica clínica para el diagnóstico, tratamiento y seguimiento de la diabetes mellitus tipo 2 en la población mayor de 18 años. Bogotá D.C.: Minsalud, 2016.
ElSayed NA, Aleppo G, American Diabetes Association, et al. 9 pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140–57.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010;1(2):100–7.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372):n71.
Makam AN, Nguyen OK. An evidence-based medicine approach to antihyperglycemic therapy in diabetes mellitus to overcome overtreatment. Circulation. 2017;135(2):180–95.
Lega IC, Campitelli MA, Austin PC, et al. Potential diabetes overtreatment and risk of adverse events among older adults in Ontario: a population-based study. Diabetologia. 2021;64(5):1093–102.
Al-Musawe L, Torre C, Guerreiro JP, et al. Overtreatment and undertreatment in a sample of elderly people with diabetes. Int J Clin Pract. 2021;75(11):e14847.
Giugliano D, Scappaticcio L, Longo M, et al. Simplification of complex insulin therapy: a story of dogma and therapeutic resignation. Diabetes Res Clin Pract. 2021;178:108958.
Cowart K. Overbasalization: addressing hesitancy in treatment intensification beyond basal insulin. Clin Diabetes. 2020;38(3):304–10.
Cowart K, Updike WH, Pathak R. Prevalence of and characteristics associated with overbasalization among patients with type 2 diabetes using basal insulin: a cross-sectional study. Clin Diabetes. 2021;39(2):173–5.
Paes AH, Bakker A, Soe-Agnie CJ. Impact of dosage frequency on patient compliance. Diabetes Care. 1997;20(10):1512–7.
Rozenfeld Y, Hunt JS, Plauschinat C, Wong KS. Oral antidiabetic medication adherence and glycemic control in managed care. Am J Manag Care. 2008;14(2):71–5.
Giugliano D, Maiorino MI, Bellastella G, Esposito K. Clinical inertia, reverse clinical inertia, and medication non-adherence in type 2 diabetes. J Endocrinol Invest. 2019;42(5):495–503.
Blak BT, Smith HT, Hards M, Curtis BH, Ivanyi T. Optimization of insulin therapy in patients with type 2 diabetes mellitus: beyond basal insulin. Diabet Med. 2012;29(7):e13–20.
Guyton J, Jeon M, Brooks A. Glucagon-like peptide 1 receptor agonists in type 1 diabetes mellitus. Am J Health Syst Pharm. 2019;76(21):1739–48.
Ramírez-Rincón A, Builes-Montaño CE, Hincapié-García JA, Blanco VM, Botero-Arango JF. Short-term effectiveness and reduction in insulin requirements in patients with type 2 diabetes treated with IdegLira in a real-world setting. Front Endocrinol (Lausanne). 2022;28(13): 828607.
Kuhtreiber WM, Washer SL, Hsu E, et al. Low levels of C-peptide have clinical significance for established type 1 diabetes. Diabet Med. 2015;32(10):1346–53.
Palmer JP, Fleming GA, Greenbaum CJ, et al. C-peptide is the appropriate outcome measure for type 1 diabetes clinical trials to preserve beta-cell function: report of an ADA workshop, 21–22 october 2001. Diabetes. 2004;53(1):250–64.
Hope SV, Knight BA, Shields BM, Hattersley AT, McDonald TJ, Jones AG. Random non-fasting C-peptide: bringing robust assessment of endogenous insulin secretion to the clinic. Diabet Med. 2016;33(11):1554–8.
Gjessing HJ, Matzen LE, Faber OK, Frøland A. Fasting plasma C-peptide, glucagon stimulated plasma C-peptide, and urinary C-peptide in relation to clinical type of diabetes. Diabetologia. 1989;32(5):305–11.
Jones AG, McDonald TJ, Shields BM, et al. Markers of β-cell failure predict poor glycemic response to GLP-1 receptor agonist therapy in type 2 diabetes. Diabetes Care. 2016;39(2):250–7.
Lingvay I, Harris S, Jaeckel E, Chandarana K, Ranthe MF, Jódar E. Insulin degludec/liraglutide (IDegLira) was effective across a range of dysglycaemia and body mass index categories in the DUAL V randomized trial. Diabetes Obes Metab. 2018;20(1):200–5.
Billings LK, Doshi A, Gouet D, et al. Efficacy and safety of IDegLira versus basal-bolus insulin therapy in patients with type 2 diabetes uncontrolled on metformin and basal insulin: the DUAL VII randomized clinical trial. Diabetes Care. 2018;41(5):1009–16.
Aroda VR, González-Galvez G, Grøn R, et al. Durability of insulin degludec plus liraglutide versus insulin glargine U100 as initial injectable therapy in type 2 diabetes (DUAL VIII): a multicentre, open-label, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7(8):596–605.
Gough SC, Bode B, Woo V, et al. Efficacy and safety of a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with its components given alone: results of a phase 3, open-label, randomised, 26-week, treat-to-target trial in insulin-naive patients with type 2 diabetes. Lancet Diabetes Endocrinol. 2014;2(11):885–93.
Nauck M, Frid A, Hermansen K, et al. Efficacy and safety comparison of liraglutide, glimepiride, and placebo, all in combination with metformin, in type 2 diabetes: the LEAD (liraglutide effect and action in diabetes)-2 study. Diabetes Care. 2009;32(1):84–90.
Heller S, Buse J, Fisher M, et al. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 1 diabetes (BEGIN basal-bolus type 1): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1489–97.
Garber AJ, King AB, Del Prato S, et al. Insulin degludec, an ultra-longacting basal insulin, versus insulin glargine in basal-bolus treatment with mealtime insulin aspart in type 2 diabetes (BEGIN basal-bolus type 2): a phase 3, randomised, open-label, treat-to-target non-inferiority trial. Lancet. 2012;379(9825):1498–507.
Zinman B, Philis-Tsimikas A, Cariou B, et al. Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: a 1-year, randomized, treat-to-target trial (BEGIN Once Long). Diabetes Care. 2012;35(12):2464–71.
Mathieu C, Hollander P, Miranda-Palma B, et al. Efficacy and safety of insulin degludec in a flexible dosing regimen vs insulin glargine in patients with type 1 diabetes (BEGIN: Flex T1): a 26-week randomized, treat-to-target trial with a 26-week extension. J Clin Endocrinol Metab. 2013;98(3):1154–62.
Fadini GP, Buzzetti R, Fittipaldi MR, et al. IDegLira for the real-world treatment of type 2 diabetes in Italy: protocol and interim results from the REX observational study. Diabetes Ther. 2022;13(8):1483–97.
American Diabetes Association. 12. Older adults: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl 1):S168–79.
Medical Writing/Editorial Assistance
Jaime Ordóñez from True Consulting provided editorial assistance, part of the medical writing, and translation into English. Novo Nordisk Colombia financed this service.
Funding
Novo Nordisk Colombia funded this study and the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
JEO wrote the “abstract,” “summary bullet points,” “introduction,” “methods” and “conclusion” sections; CB-M wrote the “definitions” and “beta cell reserve” sections; AR wrote the “insulin dose” and “initial dose” sections; and EW wrote the “titration” and “goals” units. CB-M made the table. CB-M, AR, and EW made the figure. All the authors read and approved the manuscript, the table, and the figure.
Corresponding author
Ethics declarations
Conflict of Interest
Jaime Ordóñez, Carlos Builes-Montaño, Edwin Wandurraga, and Alex Ramírez have nothing to disclose.
Ethical Approval
This article is based on previous studies and contains no new studies with human participants or animals performed by authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Builes-Montaño, C., Wandurraga, E., Ramírez, A. et al. Simplification of Complex Insulin Regimens with IdegLira in People with Type 2 Diabetes: Literature Review and Clinical Recommendations. Diabetes Ther 14, 1959–1976 (2023). https://doi.org/10.1007/s13300-023-01471-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01471-9