Abstract
Purpose
Preventing the spread of pathogens in the anesthesia work area reduces surgical site infections. Improved cleaning reduces the percentage of anesthesia machine samples with ≥ 100 colony-forming units (CFU) per surface area sampled. Targeting a threshold of < 100 CFU when cleaning anesthesia machines may be associated with a lower prevalence of bacterial pathogens. We hypothesized that anesthesia work area reservoir samples returning < 100 CFU would have a low (< 5%) prevalence of pathogens.
Methods
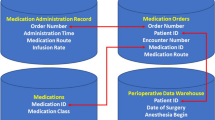
In this retrospective cohort study of bacterial count data from nine hospitals, obtained between 2017 and 2022, anesthesia attending and assistants’ hands, patient skin sites (nares, axilla, and groin), and anesthesia machine (adjustable pressure-limiting valve and agent dials) reservoirs were sampled at case start and at case end. The patient intravenous stopcock set was sampled at case end. The isolation of ≥ 1 CFU of Staphylococcus aureus, methicillin-resistant Staphylococcus aureus, Enterococcus, vancomycin-resistant Enterococcus, gram-negative (i.e., Klebsiella, Acinetobacter, Pseudomonas, and Enterobacter spp.) or coagulase-negative Staphylococcus was compared for reservoir samples returning ≥ 100 CFU vs those returning < 100 CFU.
Results
Bacterial pathogens were isolated from 24% (7,601/31,783) of reservoir samples, 93% (98/105) of operating rooms, and 83% (2,170/2,616) of cases. The ratio of total pathogen isolates to total CFU was < 0.0003%. Anesthesia machine reservoirs returned ≥ 100 CFU for 44% (2,262/5,150) of cases. Twenty-three percent of samples returning ≥ 100 CFU were positive for ≥ 1 bacterial pathogen (521/2,262; 99% lower confidence limit, 22%) vs 3% of samples returning < 100 CFU (96/2,888; 99% upper limit, 4%).
Conclusions
Anesthesia machine reservoir samples returning < 100 CFU were associated with negligible pathogen detection. This threshold can be used for assessment of terminal, routine, and between-case cleaning of the anesthesia machine and equipment. Such feedback may be useful because the 44% prevalence of ≥ 100 CFU was comparable to the 46% (25/54) reported earlier from an unrelated hospital.
Résumé
Objectif
La prévention de la propagation des agents pathogènes dans la zone de travail de l’anesthésie réduit les infections du site opératoire. L’amélioration du nettoyage réduit le pourcentage d’échantillons de l’appareil d’anesthésie présentant ≥ 100 unités de formation de colonie (UFC) par surface échantillonnée. Le fait de cibler un seuil < 100 UFC lors du nettoyage des appareils d’anesthésie pourrait être associé à une prévalence plus faible d’agents pathogènes bactériens. Nous avons émis l’hypothèse que les échantillons des réservoirs de la zone de travail d’anesthésie < 100 UFC résulteraient en une faible prévalence (< 5 %) d’agents pathogènes.
Méthode
Dans cette étude de cohorte rétrospective des données de décompte bactérien de neuf hôpitaux, obtenues entre 2017 et 2022, les mains des anesthésiologistes et des assistant·es en anesthésie, les sites cutanés des patient·es (narines, aisselles et aines) et les réservoirs de l’appareil d’anesthésie (soupape de réglage de limitation de pression et cadrans d’agent) ont été échantillonnés au début et à la fin de chaque cas. Les échantillons sur l’ensemble de robinets d’arrêt intraveineux des patient·es ont été prélevés à la fin de chaque cas. L’isolement de ≥ 1 UFC de staphylocoque doré, de staphylocoque doré résistant à la méthicilline, d’entérocoque, d’entérocoque résistant à la vancomycine, de staphylocoque à Gram négatif (c.-à-d. Klebsiella, Acinetobacter, Pseudomonas et Enterobacter spp.) ou à coagulase négative a été comparé pour les échantillons de réservoir retournant ≥ 100 UFC vs ceux qui comportaient < 100 UFC.
Résultats
Des bactéries pathogènes ont été isolées dans 24 % (7601/31 783) des échantillons de réservoir, 93 % (98/105) des salles d’opération et 83 % (2170/2616) des cas. Le rapport entre le nombre total d’isolats d’agents pathogènes et le nombre total d’UFC était de < 0,0003 %. Les échantillons pris sur les réservoirs d’appareils d’anesthésie ont retourné ≥ 100 UFC dans 44 % (2262/5150) des cas. Vingt-trois pour cent des échantillons retournés ≥ 100 UFC étaient positifs pour ≥ 1 agent pathogène bactérien (521/2262; limite de confiance inférieure à 99 %, 22 %) vs 3 % des échantillons retournant < 100 UFC (96/2888 ; 99 % de la limite supérieure, 4 %).
Conclusion
Les échantillons pris sur les réservoirs de l’appareil d’anesthésie comportant < 100 UFC étaient associés à une détection négligeable d’agents pathogènes. Ce seuil peut être utilisé pour l’évaluation du nettoyage final, de routine et entre les cas de l’appareil et de l’équipement d’anesthésie. Une telle rétroaction peut être utile parce que la prévalence de 44 % de ≥ 100 UFC était comparable aux 46 % (25/54) rapportés précédemment dans un autre hôpital.

Similar content being viewed by others
Notes
The relative risk of pathogens cultured from the adjustable pressure-limiting valve and agent dial of the anesthesia machine with ≥ 100 CFU was 6.93 relative to those same sites with < 100 CFU (99% confidence interval, 5.25 to 9.14; P < 0.0001). Given that we lacked prior data, we calculated how many more samples with bacterial pathogens could have been obtained for the < 100 CFU samples to continue to have upper 99% confidence limit < 5%. That would have been 21 more samples, because 117/2,888 has an upper 99% limit of 4.99%.
References
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 2022; 399: 629–55. https://doi.org/10.1016/s0140-6736(21)02724-0
Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis 2009; 48: 1–12. https://doi.org/10.1086/595011
Loftus RW, Dexter F, Brown JR. Transmission of Staphylococcus aureus in the anaesthesia work area has greater risk of association with development of surgical site infection when resistant to the prophylactic antibiotic administered for surgery. J Hosp Infect 2023; 134: 121–8. https://doi.org/10.1016/j.jhin.2023.01.007
Menzel J, Kühn A, Beck D, Schock B, Chaberny IF. Hand hygiene in the operating room (OR)-(not) an issue? [German]. Unfallchirurgie (Heidelb) 2023; 126: 563–8. https://doi.org/10.1007/s00113-022-01181-0
Dexter F, Loftus RW. Estimation of the contribution to intraoperative pathogen transmission from bacterial contamination of patient nose, patient groin and axilla, anesthesia practitioners' hands, anesthesia machine, and intravenous lumen. J Clin Anesth 2024; 92: 111303. https://doi.org/10.1016/j.jclinane.2023.111303
Loftus RW, Dexter F, Robinson AD. High-risk Staphylococcus aureus transmission in the operating room: a call for widespread improvements in perioperative hand hygiene and patient decolonization practices. Am J Infect Control 2018; 46: 1134–41. https://doi.org/10.1016/j.ajic.2018.04.211
Loftus RW, Dexter F, Robinson AD, Horswill AR. Desiccation tolerance is associated with Staphylococcus aureus hypertransmissibility, resistance and infection development in the operating room. J Hosp Infect 2018; 100: 299–308. https://doi.org/10.1016/j.jhin.2018.06.020
Jian Y, Zhao L, Zhao N, et al. Increasing prevalence of hypervirulent ST5 methicillin susceptible Staphylococcus aureus subtype poses a serious clinical threat. Emerg Microbes Infect 2021; 10: 109–22. https://doi.org/10.1080/22221751.2020.1868950
Zhong L, Men TY, Li H, et al. Multidrug-resistant gram-negative bacterial infections after liver transplantation—spectrum and risk factors. J Infect 2012; 64: 299–310. https://doi.org/10.1016/j.jinf.2011.12.005
Chea N, Sapiano MR, Zhou L, et al. Rates and causative pathogens of surgical site infections attributed to liver transplant procedures and other hepatic, biliary, or pancreatic procedures, 2015–2018. Transpl Infect Dis 2021; 23: e13589. https://doi.org/10.1111/tid.13589
Dexter F, Loftus RW. Retrospective cohort study of anaesthesia machines shows low bacterial contamination can be achieved with surface disinfection. Br J Anaesth 2023; 131: e109–11. https://doi.org/10.1016/j.bja.2023.07.016
Ochoa SA, Cruz-Córdova A, Mancilla-Rojano J, et al. Control of methicillin-resistant Staphylococcus aureus strains associated with a hospital outbreak involving contamination from anesthesia equipment using UV-C. Front Microbiol 2020; 11: 600093. https://doi.org/10.3389/fmicb.2020.600093
Loftus RW, Dexter F, Robinson AD. Methicillin-resistant Staphylococcus aureus has greater risk of transmission in the operating room than methicillin-sensitive S. aureus. Am J Infect Control 2018; 46: 520–5. https://doi.org/10.1016/j.ajic.2017.11.002
Clark C, Taenzer A, Charette K, Whitty M. Decreasing contamination of the anesthesia environment. Am J Infect Control 2014; 42: 1223–5. https://doi.org/10.1016/j.ajic.2014.07.016
Loftus RW, Koff MD, Burchman CC, et al. Transmission of pathogenic bacterial organisms in the anesthesia work area. Anesthesiology 2008; 109: 399–407. https://doi.org/10.1097/aln.0b013e318182c855
Loftus RW, Brown JR, Koff MD, et al. Multiple reservoirs contribute to intraoperative bacterial transmission. Anesth Analg 2012; 114: 1236–48. https://doi.org/10.1213/ane.0b013e31824970a2
Loftus RW, Dexter F, Goodheart MJ, et al. The effect of improving basic preventive measures in the perioperative arena on Staphylococcus aureus transmission and surgical site infections, a randomized clinical trial. JAMA Netw Open 2020; 3: e201934. https://doi.org/10.1001/jamanetworkopen.2020.1934
Wall RT, Datta S, Dexter F, et al. Effectiveness and feasibility of an evidence-based intraoperative infection control program targeting improved basic measures; a post-implementation prospective case-cohort study. J Clin Anesth 2022; 77: 110632. https://doi.org/10.1016/j.jclinane.2021.110632
Spertini V, Borsoi L, Berger J, Blacky A, Dieb-Elschahawi M, Assadian O. Bacterial contamination of anesthesia machines' internal breathing-circuit-systems. GMS Krankenhhyg Interdiszip 2011; 6: Doc14. https://doi.org/10.3205/dgkh000171
Biddle CJ, George-Gay B, Prasanna P, Hill EM, Davis TC, Verhulst B. Assessing a novel method to reduce anesthesia machine contamination: a prospective, observational trial. Can J Infect Dis Med Microbiol 2018; 2018: 1905360. https://doi.org/10.1155/2018/1905360
Robinson AD, Dexter F, Renkor V, Reddy S, Loftus RW. Operating room PathTrac analysis of current intraoperative Staphylococcus aureus transmission dynamics. Am J Infect Control 2019; 47: 1240–7. https://doi.org/10.1016/j.ajic.2019.03.028
Dexter F, Epstein RH, Gostine AL, Penning DH, Loftus RW. Benefit of systematic selection of pairs of cases matched by surgical specialty for surveillance of bacterial transmission in operating rooms. Am J Infect Control 2020; 48: 682–7. https://doi.org/10.1016/j.ajic.2019.09.025
Datta S, Dexter F, Ledolter J, Wall RT, Loftus RW. Sample times for surveillance of S. aureus transmission to monitor effectiveness and provide feedback on intraoperative infection control. Perioper Care Oper Room Manag 2020; 21: 100137. https://doi.org/10.1016/j.pcorm.2020.100137
Zuckerman JB, Zuaro DE, Prato BS, et al. Bacterial contamination of cystic fibrosis clinics. J Cyst Fibro 2009; 8: 186–92. https://doi.org/10.1016/j.jcf.2009.01.003
Loftus RW, Muffly MK, Brown JR, et al. Hand contamination of anesthesia providers is an important risk factor for intraoperative bacterial transmission. Anesth Analg 2011; 112: 98–105. https://doi.org/10.1213/ane.0b013e3181e7ce18
Charnin JE, Griffiths SA, Loftus CP, Dexter F, Loftus RW. Bacterial contamination of syringe tips after anaesthesia care with use of disinfectable needleless closed connector devices. Br J Anaesth 2023; 131: e112–4. https://doi.org/10.1016/j.bja.2023.06.060
Larson EL, Strom MS, Evans CA. Analysis of three variables in sampling solutions used to assay bacteria of hands: type of solution, use of antiseptic neutralizers, and solution temperature. J Clin Microbiol 1980; 12: 355–60. https://doi.org/10.1128/jcm.12.3.355-360.1980
Datta S, Dexter F, Suvarnakar A, Abi-Najm D, Wall RT, Loftus RW. Estimating costs of anesthesia supplies for intraoperative infection control. Am J Infect Control 2023; 51: 619–23. https://doi.org/10.1016/j.ajic.2022.07.028
Wilson AP, Smyth D, Moore G, et al. The impact of enhanced cleaning within the intensive care unit on contamination of the near-patient environment with hospital pathogens: a randomized crossover study in critical care units in two hospitals. Crit Care Med 2011; 39: 651–8. https://doi.org/10.1097/ccm.0b013e318206bc66
Dexter F, Brown JR, Wall RT, Loftus RW. The efficacy of multifaceted versus single anesthesia work area infection control measures and the importance of surgical site infection follow-up duration. J Clin Anesth 2023; 85: 111043. https://doi.org/10.1016/j.jclinane.2022.111043
Birnbach DJ, Rosen LF, Fitzpatrick M, Carling P, Arheart KL, Munoz-Price LS. Double gloves: a randomized trial to evaluate a simple strategy to reduce contamination in the operating room. Anesth Analg 2015; 120: 848–52. https://doi.org/10.1213/ane.0000000000000230
Dexter F, Parra MC, Brown JR, Loftus RW. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth Analg 2020; 131: 37–42. https://doi.org/10.1213/ane.0000000000004829
Dexter F, Marcon E, Aker J, Epstein RH. Numbers of simultaneous turnovers calculated from anesthesia or operating room information management system data. Anesth Analg 2009; 109: 900–5. https://doi.org/10.1213/ane.0b013e3181b08855
Goebel U, Gebele N, Ebner W, et al. Bacterial contamination of the anesthesia workplace and efficiency of routine cleaning procedures: a prospective cohort study. Anesth Analg 2016; 122: 1444–7. https://doi.org/10.1213/ane.0000000000001220
Schmidt E, Dexter F, Herrmann J, Godding JD, Hadder B, Loftus RW. Assessment of anesthesia machine redesign on cleaning of the anesthesia machine using surface disinfection wipes. Am J Infect Control 2020; 48: 675–81. https://doi.org/10.1016/j.ajic.2019.09.016
Epstein RH, Dexter F, Loftus RW. Most hospital patients at risk for bacterial infection undergo an anesthetic: implications for infection control practices related to the anesthesia workspace. Can J Anesth 2023; 70: 1330–9. https://doi.org/10.1007/s12630-023-02515-1
Loftus RW, Brindeiro BS, Kispert DP, et al. Reduction in intraoperative bacterial contamination of peripheral intravenous tubing through the use of a passive catheter care system. Anesth Analg 2012; 115: 1315–23. https://doi.org/10.1213/ane.0b013e31826d2aa4
Bode LG, Kluytmans JA, Wertheim HF, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med 2010; 362: 9–17. https://doi.org/10.1056/nejmoa0808939
Owens CD, Stoessel K. Surgical site infections: epidemiology, microbiology and prevention. J Hosp Infect 2008; 70: 3–10. https://doi.org/10.1016/s0195-6701(08)60017-1
Loftus RW, Dexter F, Evans LC, Robinson AD, Odle A, Perlman S. An assessment of the impact of recommended anesthesia work area cleaning procedures on intraoperative SARS-CoV-2 contamination, a case-series analysis. J Clin Anesth 2021; 73: 110350. https://doi.org/10.1016/j.jclinane.2021.110350
Loftus R, Dexter F, Evans L, Robinson A, Odle A, Perlman S. Evidence-based intraoperative infection control measures plus feedback are associated with attenuation of SARS-CoV-2 detection in operating rooms. Br J Anaesth 2022; 129: e29–32. https://doi.org/10.1016/j.bja.2022.04.018
Nante N, Ceriale E, Messina G, Lenzi D, Manzi P. Effectiveness of ATP bioluminescence to assess hospital cleaning: a review. J Prev Med Hyg 2017; 58: E177–83.
Author contributions
Franklin Dexter helped with investigation, validation, formal analysis, data curation, writing original draft, and reviewing and editing. Kaitlin M. Walker, Carmen Troncoso Brindeiro, Chase P. Loftus, and Cornelie C. L. Banguid helped with reviewing and editing. Randy W. Loftus helped with conceptualization, methodology, writing the original draft, and reviewing and editing.
Disclosures
Dr. Dexter serves as Guest Editor (Statistics) for the Canadian Journal of Anesthesia/Journal canadien d’anesthésie; he had no involvement in the handling of this manuscript. He is the Director of the Division of Management Consulting of the University of Iowa Department of Anesthesia, which provides consultations to corporations, hospitals, and individuals, including RDB Bioinformatics. He receives no funds personally other than his salary and allowable expense reimbursements from the University of Iowa. His family and he have no financial holdings in any company related to his work. A list of all the Division’s consults is available in his posted curriculum vitae at https://FranklinDexter.net/Contact_Info.htm. Ms. Walker, Dr. Brindeiro, Mr. Loftus, and Ms. Banguid are employees of RDB Bioinformatics. Dr. Loftus received research funding from Sage Medical Inc., BBraun, Draeger, Surfacide and Kenall, has one or more patents pending, and is a partner of RDB Bioinformatics, LLC, at 1055 N 115th St #301 (Omaha, NE, USA), the company that owns OR PathTrac. He receives no funds personally from his involvement in RDB. He has spoken at educational meetings sponsored by Kenall and BBraun.
Funding statement
Departmental funding.
Prior conference presentations
This work was presented at the International Anesthesia Research Society 2023 Annual Meeting (13–16 April 2023, Denver, CO, USA).
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dexter, F., Walker, K.M., Brindeiro, C.T. et al. A threshold of 100 or more colony-forming units on the anesthesia machine predicts bacterial pathogen detection: a retrospective laboratory-based analysis. Can J Anesth/J Can Anesth 71, 600–610 (2024). https://doi.org/10.1007/s12630-024-02707-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-024-02707-3