Abstract
Purpose
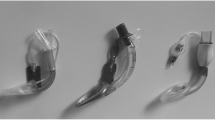
Supraglottic airway devices (SGAs) have been increasingly used as a primary airway in patients undergoing anesthesia as an alternative to endotracheal tubes. Second-generation devices have expanded their applicability to include uses in patients with obesity. Nevertheless, there is limited evidence of SGA suitability for patients with class 3 obesity (body mass index [BMI] ≥ 40 kg·m–2). As such, we compared rates of SGA functionality between patients with class 3 obesity and patients without class 3 obesity undergoing general anesthesia.
Methods
We performed a propensity score matching analysis using inverse probability of treatment weighting to compare the functionality of SGAs in adult patients with class 3 obesity vs without class 3 obesity. These patients underwent surgery at a hospital in Queensland, Australia from November 2017 to September 2020 and had a SGA inserted as part of their anesthetic care. All data were collected from patients’ electronic medical records. We included 321 patients in the cohort with class 3 obesity and 471 in the cohort without class 3 obesity (control/comparison). The estimated effect of class 3 obesity on SGAs was calculated using adjusted odds ratios (AORs) with their 95% confidence intervals (CIs).
Results
The overall weighted prevalence of nonfunctional SGAs was 3.2%, with a significantly higher rate in the class 3 obesity cohort compared with the control cohort (4.7% vs 2.1%) (P = 0.04). This adjusted analysis illustrates that class 3 obesity was associated with an almost four times higher odds of a nonfunctional SGA (odds ratio [OR], 2.3; 95% CI, 1.0 to 5.1; AOR, 3.9; 95% CI, 1.4 to 10.6) than patients without class 3 obesity.
Conclusion
Patients with class 3 obesity (BMI ≥ 40 kg·m–2) had greater than three-fold odds of nonfunctional intraoperative SGAs than patients without class 3 obesity.
Résumé
Objectif
Les dispositifs supraglottiques (DSG) sont de plus en plus utilisés comme accès primaire aux voies aériennes en tant qu’alternative aux sondes endotrachéales chez les patient·es bénéficiant d’une anesthésie. Les dispositifs de deuxième génération ont élargi leur applicabilité pour inclure des utilisations chez les personnes souffrant d’obésité. Néanmoins, il existe des données probantes limitées concernant l’adéquation des DSG pour la patientèle souffrant d’obésité de classe 3 (indice de masse corporelle [IMC] ≥ 40 kg·m–2). Pour cette raison, nous avons comparé les taux de fonctionnalité des DSG entre une patientèle souffrant d’obésité de classe 3 et une patientèle sans obésité de classe 3 bénéficiant d’une anesthésie générale.
Méthode
Nous avons réalisé une analyse d’appariement des scores de propension en utilisant la probabilité inverse de pondération du traitement pour comparer la fonctionnalité des DSG chez la patientèle adulte atteinte d’obésité de classe 3 vs sans obésité de classe 3. Ces patient·es ont bénéficié d’une intervention chirurgicale dans un hôpital du Queensland, en Australie, entre novembre 2017 et septembre 2020, et un DSG a été inséré dans le cadre de leurs soins anesthésiques. Toutes les données ont été recueillies à partir des dossiers médicaux informatisés des patient·es. Nous avons inclus 321 personnes dans la cohorte souffrant d’obésité de classe 3 et 471 dans la cohorte sans obésité de classe 3 (témoin/comparaison). L’effet estimé de l’obésité de classe 3 sur les DSG a été calculé à l’aide de rapports de cotes ajustés (RCA) avec leurs intervalles de confiance (IC) de 95%.
Résultats
La prévalence pondérée globale des DSG non fonctionnels était de 3,2 %, avec un taux significativement plus élevé dans la cohorte avec obésité de classe 3 que dans la cohorte témoin (4,7 % vs 2,1 %) (P = 0,04). Cette analyse ajustée illustre que l’obésité de classe 3 était associée à un risque presque quadruplé de non-fonctionnalité du DSG (rapport de cotes [RC], 2,3; IC 95 %, 1,0 à 5,1; RCA, 3,9; IC 95 %, 1,4 à 10,6) que chez des patient·es sans obésité de classe 3.
Conclusion
Les personnes atteintes d’obésité de classe 3 (IMC ≥ 40 kg·m–2) présentaient plus de trois fois plus de risque de non-fonctionnalité péropératoire de DSG que les personnes sans obésité de classe 3.


Similar content being viewed by others
References
Jagannathan N, Sohn LE, Sawardekar A, Gordon J, Langen KE, Anderson K. A randomised comparison of the LMA Supreme™ and LMAProSeal™ in children. Anaesthesia 2012; 67: 632–9. https://doi.org/10.1111/j.1365-2044.2012.07088.x
Schälte G, Stoppe C, Aktas M, et al. Laypersons can successfully place supraglottic airways with 3 minutes of training. A comparison of four different devices in the manikin. Scand J Trauma Resusc Emerg Med 2011; 19: 60. https://doi.org/10.1186/1757-7241-19-60
Verghese C, Brimacombe JR. Survey of laryngeal mask airway usage in 11,910 patients: safety and efficacy for conventional and nonconventional usage. Anesth Analg 1996; 82: 129–33. https://doi.org/10.1097/00000539-199601000-00023
Brimacombe J. The advantages of the LMA over the tracheal tube or facemask: a meta-analysis. Can J Anesth 1995; 42: 1017–23. https://doi.org/10.1007/bf03011075
Mao S, Du X, Ma J, Zhang G, Cui J. A comparison between laryngeal mask airway and endotracheal intubation for anaesthesia in adult patients undergoing NUSS procedure. J Thorac Dis 2018; 10: 3216–24. https://doi.org/10.21037/jtd.2018.05.74
Maltby JR, Beriault MT, Watson NC, Fick GH. Gastric distension and ventilation during laparoscopic cholecystectomy: LMA-Classic vs. tracheal intubation. Can J Anesth 2000; 47: 622–6. https://doi.org/10.1007/bf03018993
Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011; 106: 617–31. https://doi.org/10.1093/bja/aer058
Ng A, Smith G. Gastroesophageal reflux and aspiration of gastric contents in anesthetic practice. Anesth Analg 2001; 93: 494–513. https://doi.org/10.1097/00000539-200108000-00050
Brimacombe JR, Berry A. The incidence of aspiration associated with the laryngeal mask airway: a meta-analysis of published literature. J Clin Anesth 1995; 7: 297–305. https://doi.org/10.1016/0952-8180(95)00026-e
Cook TM, Kelly FE. Time to abandon the ‘vintage’ laryngeal mask airway and adopt second-generation supraglottic airway devices as first choice. Br J Anaesth 2015; 115: 497–9. https://doi.org/10.1093/bja/aev156
Prabha R, Raman R, Khan MP, Kaushal D, Siddiqui AK, Abbas H. Comparison of i-gel® for general anesthesia in obese and nonobese patients. Saudi J Anaesth 2018; 12: 535–9. https://doi.org/10.4103/sja.sja_79_18
Farouk I, Abdelhamid BM, Wishahy MK, Mohamed H, Hassan MM. Efficiency of i-gel® supraglottic airway device during mechanical ventilation in supine and lateral decubitus position in obese patient; prospective observational study. Egypt J Anaesth 2020; 36: 126–33. https://doi.org/10.1080/11101849.2020.1789811
National Health and Medical Research Council. Clinical practice guidelines for the management of overweight and obesity in adults, adolescents and children in Australia, 2013. Available from URL: https://www.nhmrc.gov.au/about-us/publications/clinical-practice-guidelines-management-overweight-and-obesity (accessed April 2023).
Jense HG, Dubin SA, Silverstein PI, O’Leary-Escolas U. Effect of obesity on safe duration of apnea in anesthetized humans. Anesth Analg 1991; 72: 89–93. https://doi.org/10.1213/00000539-199101000-00016
Asai T. Editorial II: who is at increased risk of pulmonary aspiration? Br J Anaesth 2004; 93: 497–500. https://doi.org/10.1093/bja/aeh234
Ramachandran SK, Mathis MR, Tremper KK, Shanks AM, Kheterpal S. Predictors and clinical outcomes from failed laryngeal mask airway unique™: a study of 15,795 patients. Anesthesiology 2012; 116: 1217–26. https://doi.org/10.1097/aln.0b013e318255e6ab
Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg 2015; 18: 184–90. https://doi.org/10.1016/j.ijsu.2015.04.079
Daabiss M. American Society of Anaesthesiologists physical status classification. Indian J Anaesth 2011; 55: 111–5. https://doi.org/10.4103/0019-5049.79879
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 2011; 46: 399–424. https://doi.org/10.1080/00273171.2011.568786
Barnieh L, James MT, Zhang J, Hemmelgarn BR. Propensity score methods and their application in nephrology research. J Nephrol 2011; 24: 256–62. https://doi.org/10.5301/jn.2011.6429
Ali MS, Prieto-Alhambra D, Lopes LC, et al. propensity score methods in health technology assessment: principles, extended applications, and recent advances. Front Pharmacol 2019; 10: 973. https://doi.org/10.3389/fphar.2019.00973
Stürmer T, Wyss R, Glynn RJ, Brookhart MA. Propensity scores for confounder adjustment when assessing the effects of medical interventions using nonexperimental study designs. J Intern Med 2014; 275: 570–80. https://doi.org/10.1111/joim.12197
Nicholson A, Cook TM, Smith AF, Lewis SR, Reed SS. Supraglottic airway devices versus tracheal intubation for airway management during general anaesthesia in obese patients. Cochrane Database Syst Rev 2013; 9: CD010105. https://doi.org/10.1002/14651858.cd010105.pub2
Reinius H, Jonsson L, Gustafsson S, et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 2009; 111: 979–87. https://doi.org/10.1097/aln.0b013e3181b87edb
Talab HF, Zabani IA, Abdelrahman HS, et al. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg 2009; 109: 1511–6. https://doi.org/10.1213/ane.0b013e3181ba7945
Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth 2009; 102: 862–8. https://doi.org/10.1093/bja/aep084
Verghese C, Ramaswamy B. LMA-Supreme™—a new single-use LMA with gastric access: a report on its clinical efficacy. Br J Anaesth 2008; 101: 405–10. https://doi.org/10.1093/bja/aen174
Littleton SW. Impact of obesity on respiratory function. Respirology 2012; 17: 43–9. https://doi.org/10.1111/j.1440-1843.2011.02096.x
Grieco DL, Anzellotti GM, Russo A, et al. Airway closure during surgical pneumoperitoneum in obese patients. Anesthesiology 2019; 131: 58–73. https://doi.org/10.1097/aln.0000000000002662
Author contributions
Patrick Hartsuyker and Marcelo E. Kanczuk contributed to the study conception, study design, and data collection and writing of the manuscript. Matthew Hiskens contributed to the study design and writing of the manuscript. Tesfaye S. Mengistu developed the study design, performed the statistical analysis, and contributed to writing of the manuscript. Matthew Hiskens, Marcelo E. Kanczuk, David Lawn, and Salwa Beg contributed to the writing and revised the manuscript for important intellectual content. All authors read and approved the final version.
Disclosures
None.
Funding statement
None.
Data availability
Data related to this work are available as tables, figures, and supplementary files.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hartsuyker, P., Kanczuk, M.E., Lawn, D. et al. The effect of class 3 obesity on the functionality of supraglottic airway devices: a historical cohort analysis with propensity score matching. Can J Anesth/J Can Anesth 70, 1744–1752 (2023). https://doi.org/10.1007/s12630-023-02582-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-023-02582-4