Abstract
Purpose
This study aims to assess the advances brought by digital technologies in medical practices and uncover why the HC sector is reluctant to adopt DT.
Methodology
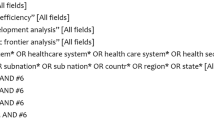
To answer these questions, a systematic literature review (SLR) was conducted covering the time frame from 2005-June 2022 and a total number of 1736 articles were gathered out of which 32 were selected and used for this study, adopting Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA).
Results
This study grouped and categorized areas that most of the research about the digitization of healthcare falls into Advances in the use of telemedicine and m-health; Advances in the use of AI and robotics; Advances in the use of EMR and blockchain; and finally, Advances in the use of other ICT. Our findings showed that the adoption of DT in healthcare can give more freedom and empower patients, ensure the security of patients’ data and information, enable remote COVID-19 and disease progression monitoring, and management, and lastly increase organizational and managerial efficiencies. The results, however, showed that healthcare is hesitant to the adoption of digitization because of organizational factors (e.g., unfavorable policies and culture); Technological factors (e.g., fear of security and reliability); Human factors (e.g., lack of skills and acceptance); and Economic factors (e.g., lack of capital and resources). Areas of further interest to scholars and practitioners were also provided.
Conclusion
This SLR has presented various applications of blockchain, EMRs, AI, robotics, telemedicine, etc. in the HC and how they are transforming and improving patient care delivery, increasing efficiency, disease monitoring and management, and expatiate on the organizational, technological, human, and economic factors as the main rationales behind HC reluctance to adopting DT despite the aforementioned benefits. Future research may investigate issues concerning data security, knowledge, skills, culture, and policy transformation of HC organizations to promote wider acceptance and adoption of DT in this sector.




Similar content being viewed by others
Availability of data and materials
Not applicable.
Code availability
Not applicable.
References
Chirumalla K. Building digitally-enabled process innovation in the process industries: A dynamic capabilities approach. Technovation. 2021:105–102256. https://www.sciencedirect.com/science/article/pii/S0166497221000377.
Hermes S, Riasanow T, Clemons EK, Böhm M, Krcmar H. The digital transformation of the healthcare industry: exploring the rise of emerging platform ecosystems and their influence on the role of patients. Bus Res. 2020;13(3):1033–69. https://doi.org/10.1007/s40685-020-00125-x.
Tian J, Coreynen W, Matthyssens P, Shen L. Platform-based servitization and business model adaptation by established manufacturers. Technovation. 2021;118:102222. https://www.sciencedirect.com/science/article/pii/S0166497221000031?casa_token.
Elton J, O’Riordan A. Healthcare disrupted: Next generation business models andstrategies. 2016. https://books.google.com/books?hl=it&lr=lang_en&id=ZBElCgAAQBAJ&oi=fnd&pg.
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC. Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res. 2021;123:557–67. https://doi.org/10.1016/j.jbusres.2020.10.030.
Vial G. Understanding digital transformation: A review and a research agenda. Manag Digit Trans. 2021:13–66. https://doi.org/10.4324/9781003008637-4/UNDERSTANDING-DIGITAL-TRANSFORMATION-GREGORY-VIAL.
Verhoef PTB. Marketing perspectives on digital business models: A framework and overview of the special issue. Int J Res Mark. 2019;36(3):341–9. https://www.sciencedirect.com/science/article/pii/S0167811619300497.
Cobianchi L, Dal Mas F, Peloso A, et al. Planning the full recovery phase: an antifragile perspective on surgery after COVID-19. Ann Surg. 2020a;272(6):E296–E299a. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7668329/.
Cobianchi L, Pugliese L, Peloso A, et al. To a new normal: surgery and COVID-19 during the transition phase. Ann Surg. 2020b;272(2):E49–E51b. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7268821/pdf/ansu-272-e049.pdf.
Drago C, Gatto A, Ruggeri M. Telemedicine as technoinnovation to tackle COVID-19: A bibliometric analysis. Technovation. 2021;102417:102–417. https://www.sciencedirect.com/science/article/pii/S016649722100198X?casa_token.
Madhavan S, Bastarache L, et al. Use of electronic health records to support a public health response to the COVID-19 pandemic in the United States: a perspective from 15 academic medical centers. J Am Med Inform Assoc. 2021;28(2):393–401. https://doi.org/10.1093/jamia/ocaa287.
Sarker S, Jamal L, Ahmed SF, Irtisam N. Robotics and artificial intelligence in healthcare during COVID-19 pandemic: Systematic Rev Robot Auton Syst. Elsevier B.V. 2021;146. https://doi.org/10.1016/j.robot.2021.103902.
Tortorella GL, Fogliatto FS, Saurin TA, Tonetto LM, McFarlane D. Contributions of healthcare 4.0 digital applications to the resilience of healthcare organizations during the COVID-19 outbreak. Technovation. 2022;111:102379. https://doi.org/10.1016/j.technovation.2021.102379.
Tortorella GL, Saurin TA, Fogliatto FS, Rosa VM, Tonetto LM, Magrabi F. Impacts of healthcare 4.0 digital technologies on the resilience of hospitals. Technol Forecast Soc Chang. 2021;166:120666. https://doi.org/10.1016/j.techfore.2021.120666.
Agarwal R, Gao GG, DesRoches C, Jha AK. The digital transformation of healthcare: current status and the road ahead. Inf Syst Res. 2010;21(4):796–809. https://doi.org/10.1287/isre.1100.0327.
Marques ICP, Ferreira JJM. Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. 2020;10(3):575–586. Springer. https://doi.org/10.1007/s12553-019-00402-8.
Massaro M. Digital transformation in the healthcare sector through blockchain technology. Insights from academic research and business developments. Technovation. 2021:102386. https://doi.org/10.1016/j.technovation.2021.102386.
Sousa M, Rocha Á. Digital learning: developing skills for digital transformation of organizations. Future Gener Comput Syst. 2019;91:327–34. https://www.sciencedirect.com/science/article/pii/S0167739X18311191?casa_token=.
Reis J, Amorim M, Melão N, Matos P. Digital transformation: a literature review and guidelines for future research. Springer; 2018. https://link.springer.com/chapter/10.1007/978-3-319-77703-0_41.
Sebastian IM, Moloney KG, Ross JW, Fonstad NO, Beath C, Mocker M. How big old companies navigate digital transformation. Strateg Inf Manag. 2017;16(3):133–150. Routledge.
Golinelli D, Boetto E, Carullo G, Nuzzolese AG, Landini MP, Fantini MP. Adoption of digital technologies in health care during the COVID-19 pandemic: systematic review of early scientific literature. J Med Internet Res. 2020;22(11). JMIR publications Inc. https://doi.org/10.2196/22280.
Budd J, Miller BS, Manning EM, Lampos V, Zhuang M, Edelstein M, Rees G, Emery VC, Stevens MM, Keegan N, Short MJ, Pillay D, Manley E, Cox IJ, Heymann D, Johnson AM, McKendry RA. Digital technologies in the public-health response to COVID-19. Nat Med Nat Res. 2020;26(8):1183–1192. https://doi.org/10.1038/s41591-020-1011-4.
Hee Lee D, Yoon SN. Application of artificial intelligence-based technologies in the healthcare industry: opportunities and challenges. Int J Environ Res Public Health. 2021;18(1):1–18. https://doi.org/10.3390/ijerph18010271.
White M. Digital workplaces: vision and reality. Bus Info Rev. 2012;29. https://scholar.google.com/scholar?hl=en&as_sdt=0%2C5&q=White%2C+M.+Digital+workplaces%3A+Vision+and+reality.+Bus.+Inf.+Rev.+2012%2C+&btnG=.
Kane GC, Palmer D, Phillips AN, Kiron D, Buckley N. Strategy, not technology, drives digital transformation, vol. 14. Birmingham, AL, USA: MIT Sloan Management Review and Deloitte University Press. 2015:1–25. https://sloanreview.mit.edu/projects/strategy-drives-digital-transformation/.
Udovita PVMVD. Conceptual review on dimensions of digital transformation in modern era. Int J Sci Res Publ. 2020;10(2):520–9. https://doi.org/10.29322/IJSRP.10.02.2020.p9873.
Bunduchi R, Tursunbayeva A, Pagliari C. Coping with institutional complexity: intersecting logics and dissonant visions in a nation-wide healthcare IT implementation project. Inf Technol People. 2020;33(1):311–39. https://doi.org/10.1108/ITP-08-2018-0373/FULL/HTML.
Gong C, Ribiere V. Developing a unified definition of digital transformation. Technovation. 2021;102:102217. https://doi.org/10.1016/J.TECHNOVATION.2020.102217.
Majchrzak A, Markus ML, Wareham J. Designing for digital transformation. MIS Quarterly. 2016;40(2):267–78. https://doi.org/10.25300/MISQ/2016/40:2.03.
Burton-Jones A, Akhlaghpour S, Ayre S, et al. Changing the conversation on evaluating digital transformation in healthcare: insights from an institutional analysis. Elsevier. 2020:100–255. https://www.sciencedirect.com/science/article/pii/S1471772718302689.
Haggerty E. Healthcare and digital transformation. Netw Secur. 2017;8:7–11. https://www.sciencedirect.com/science/article/pii/S1353485817300818.
Alloghani M, Al-Jumeily D, Hussain A. Healthcare services innovations based on the state of the art technology trend industry 4.0. 11th International Conference on Developments in ESystems Engineering (DeSE). 2018. https://ieeexplore.ieee.org/abstract/document/8648605/.
Sannino G, de Pietro G. A deep learning approach for ECG-based heartbeat classification for arrhythmia detection. Future Gener Comput. 2018;86:446–55. https://www.sciencedirect.com/science/article/pii/S0167739X17324548?casa_token=.
Rghioui A, et al. Challenges and opportunities of internet of things in healthcare. J Electr Comput Eng. 2018;8:2753–61. https://www.academia.edu/download/63986601/13_12sep_17_22des_17_8832-13307-1-ED.docx_Edit_I20200721-122916-1nqs2zv.pdf.
Sakr S, Elgammal A. Towards a comprehensive data analytics framework for smart healthcare services. Big Data Res. 2016;4:44–58. http://dx.doi.org/10.1016/j.bdr.2016.05.002.
Almulhim M, Islam N, Zaman N. A lightweight and secure authentication scheme for IoT based e-health applications. Int J Comp Sci Netw Secur. 2019;19(1). https://seap.taylors.edu.my/file/rems/publication/109566_5572_1.pdf.
Rajan J, Care SR. An internet of things based physiological signal monitoring and receiving system for virtual enhanced health care network. Technol Health. 2018;26(2):379–85. https://content.iospress.com/articles/technology-and-health-care/thc171173.
Pan J, Ding S, Wu D, Yang S, Yang J. Exploring behavioural intentions toward smart healthcare services among medical practitioners: a technology transfer perspective. Int J Prod Res. 2019;57(18):5801–20. https://doi.org/10.1080/00207543.2018.1550272.
Acharyulu GVRK. Information management in a health care system: knowledge management perspective. Int J Innov Manag Technol. 2011;2(6). http://www.ijimt.org/papers/187-M639.pdf.
Manogaran G, Thota C, Lopez D, Vijayakumar V, Abbas KM, Sundarsekar R. Big data knowledge system in healthcare. In: Internet of things and big data technologies for next generation healthcare. Springer; 2017:133–57. https://doi.org/10.1007/978-3-319-49736-5_7.
Berlinger N, Wynia M, Powell T, Micah Hester D, Milliken A, Fabi R, Cohn F, Guidry-Grimes LK, Carlin Watson J, Bruce L, Chuang EJ, Oei G, Abbott J, Piper Jenks N. Ethical framework for Health Care institutions responding to novel coronavirus SARS-CoV-2 (COVID-19) guidelines for institutional ethics services responding to COVID-19: Manag Uncertain Safeguar Comm Guid Pract. 2020.
Kuo C, Pilling L, Atkins J, et al. APOE e4 genotype predicts severe COVID-19 in the UK biobank community cohort. J Gerontol: Series A. 2020;75:2231–2. https://academic.oup.com/biomedgerontology/article-abstract/75/11/2231/5843454.
Siegel D, Reses H, et al. Trends in COVID-19 cases, emergency department visits, and hospital admissions among children and adolescents aged 0–17 years—United States, August 2020–August 2021. MMWR Morb Mortal Wkly Rep. 2020:1249–54. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8437056/.
Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy. 2014;3(2):77. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4122083/.
Hassounah M, Raheel H, Alhefzi M. Digital response during the COVID-19 pandemic in Saudi Arabia. J Med Internet Res. 2020;22(9):e19338. https://www.jmir.org/2020/9/e19338/.
Della VM. What is e-Health (2): the death of telemedicine? J Med Internet Res. 2001;3(2):E22. https://nursing.jmir.org/2001/2/e22/.
Doshi P. Will covid-19 vaccines save lives? Current trials aren’t designed to tell us. Bmj. 2020;371. https://doi.org/10.1136/bmj.m4037.
Kaminski. Informatics in the time of COVID-19. Can J Nurs Inform. 2020;15(1):1. https://cjni.net/journal/?p=6820.
Arni P, Laddha S. Adoption of digital Marketing in Health Industry. SIES J Manag. 2017. https://search.ebscohost.com/login.aspx?direct=true&profile=ehost&scope=site.
World Health Organization. Telemedicine: opportunities and developments in member states. Report on the second global survey on eHealth. 2010. https://www.cabdirect.org/cabdirect/abstract/20133159246.
Komorowski M, Celi LA. Will artificial intelligence contribute to overuse in healthcare? Crit Care Med. 2017;45(5):912–3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5679196/.
Khezr S, Moniruzzaman M, Yassine A, Benlamri R. Blockchain technology in healthcare: A comprehensive review and directions for future research. Appl Sci (Switzerland). 2019;9(9):1736. https://doi.org/10.3390/app9091736.
Nguar KDA. A systematic review of technological innovation and e-government on public management reforms in developing countries. Int J Electron Gov. 2022;14(3):339–60.
Chiuchisan I, Costin H-N, Geman O. Adopting the internet of things technologies in health care systems. Int Conf Expo Electr Power Eng (EPE). 2014. https://ieeexplore.ieee.org/abstract/document/6969965/?casa_token.
Aceto G, Persico V, Pescapé A. The role of information and communication technologies in healthcare: taxonomies, perspectives, and challenges. J Netw Comput Appl. 2018;107:125–54. https://doi.org/10.1016/J.JNCA.2018.02.008.
Nambiar R, Bhardwaj R, Sethi A. A look at challenges and opportunities of big data analytics in healthcare. IEEE Int Conf Big Data. 2013. https://ieeexplore.ieee.org/abstract/document/6691753/?cas.
Raghupathi W, Raghupathi V. Big data analytics in healthcare: promise and potential. Health Inf Sci Syst. 2014;2(1):1–10. https://doi.org/10.1186/2047-2501-2-3.
Margaret M, Hansen E, Hansen MM, Miron-Shatz T, Lau AYS, Paton C. Big data in Science and healthcare: A review of recent literature and perspectives. Yearb Med Inform. 2014;23:21–6. https://doi.org/10.15265/IY-2014-0004.
Chakravorty T, Jha K, Barthwal S. Linking EHR and ERP adoption with flexibility in Care-delivery and operational performance: A conceptual review in hospital supply chain. Indian J Public Health Res Dev. 2019;10(6). https://doi.org/10.5958/0976-5506.2019.01363.9.
Evans DS, Matchmakers R. The new economics of multisided platforms. 2016. https://books.google.com/books?hl=it&lr=lan.
Yang CT, Shih WC, Chen LT, Kuo CT, Jiang FC, Leu FY. Accessing medical image file with co-allocation HDFS in cloud. Futur Gener Comput Syst. 2015;43–44:61–73. http://dx.doi.org/10.1016/j.future.2014.08.008.
World Health Organization. (2011). mHealth: new horizons for health through mobile technologies. Cabdirect.Org. https://www.cabdirect.org/cabdirect/abstract/20113217175.
Kumar M, Shankar Mukherjee P, Mohan Misra N. Advancement and current status of wear debris analysis for machine condition monitoring: a review. Ind Lubr Tribol. 2013;65(1):3–11. https://doi.org/10.1108/00368791311292756/FULL/HTML.
Topol E, Steinhubl S, Jama AT. Digital medical tools and sensors. JAMA. 2015;313(4):353–4. https://jamanetwork.com/journals/jama/article-abstract/2091997?casa_.
Silva B, Rodrigues J, de la Torre Díez I. Mobile-health: A review of current state in 2015. J Biomed Inform. 2015:265–72. https://www.sciencedirect.com/science/article/pii/S1532046415001136.
Denyer D, Neely A. Introduction to special issue: innovation and productivity performance in the UK. Int J Manag Rev. 2004;5–6(3–4):131–5. https://doi.org/10.1111/J.1460-8545.2004.00100.X.
Kivimaa P, Boon W, Hyysalo S, Klerkx L. Towards a typology of intermediaries in sustainability transitions: A systematic review and a research agenda. Res Policy. 2019:1062–75. https://www.sciencedirect.com/science/article/pii/S0048733318302385.
Tranfield D, Denyer D, Smart P. Towards a methodology for developing evidence-informed management knowledge by means of systematic review. Br J Manag. 2003;14(3):207–22. https://doi.org/10.1111/1467-8551.00375.
Kraus S, Breier M, Dasí-Rodríguez S. The art of crafting a systematic literature review in entrepreneurship research. Int Entrep Manag. 2020;16:1023–1042. https://link.springer.com/article/10.1007/s11365-020-00635-4.
de Jong JM, Ogink PAM, van Bunningen CGM, Driessen RJB, Engelen LJLPG, Heeren B, et al. A cloud-based virtual outpatient clinic for patient-centered care: proof-of-concept study. J Med Internet Res. 2018;20(9).
Dicuonzo G, Donofrio F, Fusco A, Shini M. Healthcare system: moving forward with artificial intelligence. Technovation. 2022. https://doi.org/10.1016/j.technovation.2022.102510.
Laurenza E, Quintano M, Schiavone F, Vrontis D. The effect of digital technologies adoption in healthcare industry: A CASE based analysis. 2018.
Yin R. Case study research: design and methods. 2009. https://books.google.com/books?hl=it&lr=lang_en&id=FzawIAdilHkC&oi=fnd&pg=PR1&dq=yin+2009+case+study&ots=l_3Q0ajW4q&sig=9_dRprKymaRnnFqVx0Q6cljGa.
Bokolo AJ. Application of telemedicine and eHealth technology for clinical services in response to COVID-19 pandemic. Health Technol. 2021;11(2):359–66. https://doi.org/10.1007/s12553-020-00516-4.
Baudier P, Kondrateva G, Ammi C, Chang V, Schiavone F. Digital transformation of healthcare during the COVID-19 pandemic: patients’ teleconsultation acceptance and trusting beliefs. Technovation. 2022. https://doi.org/10.1016/j.technovation.2022.102547.
Agnihothri S, Cui L, Delasay M, Rajan B. The value of mHealth for managing chronic conditions. Health Care Manag Sci. 2020;23(2):185–202. https://doi.org/10.1007/s10729-018-9458-2.
Yousaf K, Mehmood Z, Awan IA, Saba T, Alharbey R, Qadah T, Alrige MA. A comprehensive study of mobile-health based assistive technology for the healthcare of dementia and Alzheimer’s disease (AD). Health Care Manag Sci. 2020;23(2):287–309. https://doi.org/10.1007/s10729-019-09486-0.
Thrall JH. Teleradiology. Part II. Limitations, risks, and opportunities. Radiology. 2007;244(2):325–8.
Barneveld Binkhuysen FH, Ranschaert ER. Teleradiology: evolution and concepts. Eur J Radiol. 2011;78(2):205–9. https://doi.org/10.1016/j.ejrad.2010.08.027.
Rigotti NA, Taylor KL, Beneventi D, King A, Kotsen C, Fleisher L, Goldstein AO, Park ER, Sherman SE, Steinberg MB, Albert DA, Cox LS, Hayes RB, Hohl SD, Sheffer CE, Shoenbill KA, Simmons VN, Warren GW, Adsit R, et al. Telehealth delivery of tobacco cessation treatment in Cancer Care: an ongoing innovation accelerated by the COVID-19 pandemic. J Natl Compr Canc Netw. 2021;19:S21–4. https://doi.org/10.6004/JNCCN.2021.7092.
Shaheen MY. Article title: applications of artificial intelligence (AI) in healthcare: A review applications of artificial intelligence (AI) in healthcare: A review. 2021. https://doi.org/10.14293/S2199-1006.1.SOR-.PPVRY8K.v1.
Khan ZH, Siddique A, Lee CW. Robotics utilization for healthcare digitization in global COVID-19 management. Int J Environ Res Public Health. 2020;17:3819. https://doi.org/10.3390/IJERPH17113819.
Zemmar A, Lozano AM, Nelson BJ. The rise of robots in surgical environments during COVID-19. Nat Mach Intell. 2020;2(10):566–72. https://doi.org/10.1038/s42256-020-00238-2.
Cerchione R, Centobelli P, Riccio E, Abbate S, Oropallo E. Blockchain’s coming to hospital to digitalize healthcare services: designing a distributed electronic health record ecosystem. Technovation. 2022;120:102480. https://doi.org/10.1016/j.technovation.2022.102480.
Galligioni E, Berloffa F, Caffo O, Tonazzolli G, Ambrosini G, Valduga F, Eccher C, Ferro A, Forti S. Development and daily use of an electronic oncological patient record for the total management of cancer patients: 7 years’ experience. Ann Oncol. 2009;20(2):349–52. https://doi.org/10.1093/ANNONC/MDN567.
Chaplin B, Meloni S, Eisen G, Jolayemi T, Banigbe B, Adeola J, Wen C, Reyes Nieva H, Chang C, Okonkwo P, Kanki P. Scale-up of networked HIV treatment in Nigeria: creation of an integrated electronic medical records system. Int J Med Inform. 2015;84(1):58–68. https://doi.org/10.1016/J.IJMEDINF.2014.09.006.
Pahl C, Zare M, Nilashi M, de Faria Borges MA, Weingaertner D, Detschew V, Supriyanto E, Ibrahim O. Role of OpenEHR as an open source solution for the regional modelling of patient data in obstetrics. J Biomed Inform. 2015;55:174–87. https://doi.org/10.1016/J.JBI.2015.04.004.
Knake LA, Ahuja M, McDonald EL, Ryckman KK, Weathers N, Burstain T, Dagle JM, Murray JC, Nadkarni P. Quality of EHR data extractions for studies of preterm birth in a tertiary care center: guidelines for obtaining reliable data. BMC Pediatr. 2016;16(1):1–8. https://doi.org/10.1186/S12887-016-0592-Z/TABLES/3.
Ozdemir Z, Barron J, Bandyopadhyay S. An analysis of the adoption of digital Health records under switching costs. Inf Syst Res. 2011;22(3):491–503. https://doi.org/10.1287/ISRE.1110.0349.
Abdel-Basset M, Chang V, Nabeeh NA. An intelligent framework using disruptive technologies for COVID-19 analysis. Technol Forecast Soc Chang. 2021;163. https://doi.org/10.1016/j.techfore.2020.120431.
Raimo N, de Turi I, Albergo F, Vitolla F. The drivers of the digital transformation in the healthcare industry: an empirical analysis in Italian hospitals. Technovation. 2022;121:–102558. https://doi.org/10.1016/j.technovation.2022.102558.
Li JPO, Liu H, Ting DSJ, Jeon S, Chan RVP, Kim JE, Sim DA, Thomas PBM, Lin H, Chen Y, Sakomoto T, Loewenstein A, Lam DSC, Pasquale LR, Wong TY, Lam LA, Ting DSW. Digital technology, tele-medicine and artificial intelligence in ophthalmology: A global perspective. In: Progress in retinal and eye research, vol. 82. Elsevier Ltd.; 2021. https://doi.org/10.1016/j.preteyeres.2020.100900.
Sun TQ, Medaglia R. Artificial intelligence entering public healthcare ecosystems: do policies matter? 2018. https://core.ac.uk/download/pdf/211745609.pdf.
Belliger A, Krieger DJ. The digital transformation of healthcare. In: Management in Digital Change: New Findings and Practical Cases; 2018. p. 311–26. https://doi.org/10.1007/978-3-319-73546-7_19.
Imison C, Castle-Clarke S, Watson R, Edwards N. Delivering the benefits of digital health care. London: Nuffield Trust. 2016. https://www.atmedics.com/wp-content/uploads/2016/02/nuffield-trust-delivering-the-benefits-of-digital-care-17-02-2016.pdf.
IMDRF. International medical device regulators forum. 2017. https://www.imdrf.org.
ISO (2013) ISO/IEC 27001:2013. Information technology-Security techniques-Information security management system-Requirements. 2014. https://www.iso27001security.com/html/27001.html.
French-Mowat E, Burnett J. How are medical devices regulated in the European union? J R Soc Med. 2012;105(1):22–8.
European Parliament and Council of the European Union. General data protection regulation. 2017. https://gdpr-info.eu/.
European Commission. A proposal for regulation of the European Parliament and of the council laying down harmonised rules on artificial intelligence (artificial intelligence act) and Amending Certain Union Legislative Acts. 2021.
US FDA. Mobile medical applications: guidance for industry and Food and Drug Administration staff. 2023.
FDA. Artificial Intelligence and Machine Learning in Software as a Medical Device 2021. 2022. https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-software-medical-device.
American Academy of Dermatology. (2013). https://www.aad.org/forms/policies/uploads/ps/ps-telemedicine%206–15–07.
American College of Radiology. American College of Radiology Task Force on International Teleradiology. 2013. https://www.acr.org/membership/megal-business-practices/telemedicine-teleradiology/report-ofthe-acr-task-force-on-international-teleradiology/.
American Medical Association. 2013. https://www.ama-assn.org/resources/doc/councilon-med-ed/res317a08.pdf.
American Telemedicine Association Standards & Guidelines. 2013. https://www.americantelemed.org/practice/standards/ata-standards-suidelines/.
Funding
None.
Author information
Authors and Affiliations
Contributions
Not applicable.
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kakale, M.M. Of digital transformation in the healthcare (systematic review of the current state of the literature). Health Technol. 14, 35–50 (2024). https://doi.org/10.1007/s12553-023-00803-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-023-00803-w