Abstract
Purpose
This study aimed to provide a bibliometric analysis reviewing research trends and developments in wearable health sensors over the past decade. The goal was to map the research landscape to reveal maturation levels, translational gaps, and developmental arcs that can inform future inquiry.
Methods
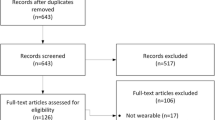
Database searches in Scopus and Web of Science identified 147 relevant English papers after duplication removal. Publication growth rates, active countries/institutions, subject areas, citation analysis, and keyword co-occurrence mapping were conducted using Biblioshiny, VOSviewer, and ScientoPy.
Results
Publication output exhibited a 20.7% average annual growth rate, demonstrating rising research interest. India, Singapore, and the US led country contributions, while MIT and technology universities were top institutions. Engineering dominated, but chemistry and materials science saw high growth. The journal Sensors published the most papers. Review and implementation papers were well-cited for consolidating knowledge. Analysis of keywords uncovered an arc from foundational to applied to translational research.
Conclusions
Wearable sensor research has rapidly expanded, led by technology-focused countries and institutions. While engineering innovation continues, interdisciplinary expansion is underway. Initial exploratory focus has progressed to health monitoring applications and clinical translation. However, technology readiness has outpaced clinical validation and real-world viability assessments. Strategic partnerships between technical and clinical stakeholders are vital to translate wearable sensors from bench to bedside. This bibliometric analysis provides a research landscape overview to guide future inquiry and stakeholder decision-making.





Similar content being viewed by others
References
Nan X, Wang X, Kang T, Zhang J, Dong L, Dong J, Wei D. Review of flexible wearable sensor devices for biomedical application. Micromachines. 2022;13(9):1395. https://doi.org/10.3390/mi13091395.
Di Pasquale V, De Simone V, Radano M, Miranda S. Wearable devices for health and safety in production systems: a literature review. IFAC-PapersOnLine. 2022;55(10):341–6. https://doi.org/10.1016/j.ifacol.2022.09.410.
Nasiri S, Khosravani MR. Progress and challenges in fabrication of wearable sensors for health monitoring. Sensors Actuators A Phys. 2020;312:112105. https://doi.org/10.1016/j.sna.2020.112105.
Liu B, Ridder A, Smith V, Thilaganathan B, Bhide A. Feasibility of antenatal ambulatory fetal electrocardiography: a systematic review. J Matern Fetal Neonatal Med. 2023;36(1):2204390. https://doi.org/10.1080/14767058.2023.2204390.
Boulif A, Ananou B, Ouladsine M, Delliaux S. A literature review: ECG-based models for arrhythmia diagnosis using artificial intelligence techniques. Bioinform Biol Insights. 2023;17:11779322221149600. https://doi.org/10.1177/11779322221149600.
dos Santos Silva A, Correia MV, Costa A, da Silva HP. Towards industrially feasible invisible electrocardiography (ECG) in sanitary facilities. In: 2023 IEEE 7th Portuguese meeting on bioengineering (ENBENG); 2023, June. p. 1–4. https://doi.org/10.1109/ENBENG58165.2023.10175356.
Rizqyawan MI, Nuryatno ET, Fakhrurroja H, Munandar A, Wibowo JW, Kusumandari DE, Salim TI. Exploration of ECG-based real-time arrhythmia detection: a systematic literature review. In: 2022 IEEE international conference advancement in data science, E-learning and information systems (ICADEIS); 2022, November. p. 01–8. https://doi.org/10.1109/ICADEIS56544.2022.10037399.
Hysing J, Gibbs C, Holla ØL, Thalamus J, Haugaa KH. Moderately prolonged QTc in computer-assessed ECG, random variation or significant risk factor? A Literature Review. Cardiogenetics. 2022;12(3):261–9. https://doi.org/10.3390/cardiogenetics12030025.
Ismail L, Karwowski W, Hancock PA, Taiar R, Fernandez-Sumano R. Electroencephalography (EEG) physiological indices reflecting human physical performance: a systematic review using updated PRISMA. J Integr Neurosci. 2023;22(3):62. https://doi.org/10.31083/j.jin2203062.
Mesin L, Cipriani GE, Amanzio M. Electroencephalography-Based Brain–Machine Interfaces in Older Adults: A Literature Review. Bioengineering. 2023;10(4):395. https://doi.org/10.3390/bioengineering10040395.
Astuti RD, Suhardi B, Laksono PW, Susanto N, Muguro J. Literature review: impact of noise on cognitive performance using electroencephalography. Appl Mech Mater. 2023;913:131–47. https://doi.org/10.4028/p-052746.
Anders C, Arnrich B. Wearable electroencephalography and multi-modal mental state classification: a systematic literature review. Comput Biol Med. 2022:106088. https://doi.org/10.1016/j.compbiomed.2022.106088.
Farizal A, Wibawa AD, Pamungkas Y, Pratiwi M, Mas A. Classifying known/unknown information in the brain using electroencephalography (EEG) signal analysis. In: 2022 11th IEEE electrical power, electronics, communications, controls and informatics seminar (EECCIS); 2022, August. p. 362–7. https://doi.org/10.1109/EECCIS54468.2022.9902928.
Alix JJ, Plesia M, Shaw PJ, Mead RJ, Day JC. Combining electromyography and Raman spectroscopy: optical EMG. Muscle Nerve. 2023. https://doi.org/10.1002/mus.27937.
Hassan ZU, Bashir N, Iltaf A. Electromyography and speech controlled prototype robotic Car using CNN based classifier for EMG. In: 2022 IEEE international conference on emerging trends in electrical, control, and telecommunication engineering (ETECTE); 2022, December. p. 1–5. https://doi.org/10.1109/ETECTE55893.2022.10007092.
Yuan W, Zou K, Zhao Y, Xi N. Detection of human action intention by electromyography (EMG). In: 2022 IEEE 12th international conference on CYBER Technology in Automation, control, and intelligent systems (CYBER); 2022, July. p. 750–4. https://doi.org/10.1109/CYBER55403.2022.9907225.
Toledo-Peral CL, Vega-Martínez G, Mercado-Gutiérrez JA, Rodríguez-Reyes G, Vera-Hernández A, Leija-Salas L, Gutiérrez-Martínez J. Virtual/augmented reality for rehabilitation applications using electromyography as control/biofeedback: systematic literature review. Electronics. 2022;11(14):2271. https://doi.org/10.3390/electronics11142271.
Wu D, Yang J, Sawan M. Transfer learning on electromyography (EMG) tasks: approaches and beyond. IEEE Transac Neural Syst Rehab Eng. 2023;31. https://doi.org/10.1109/TNSRE.2023.3295453.
Kim KB, Baek HJ. Photoplethysmography in wearable devices: a comprehensive review of technological advances, current challenges, and future directions. Electronics. 2023;12(13):2923. https://doi.org/10.3390/electronics12132923.
Lyzwinski LN, Elgendi M, Menon C. The use of Photoplethysmography in the assessment of mental health: scoping review. JMIR Mental Health. 2023;10:e40163. https://doi.org/10.2196/40163.
Sadaghiani SM, Bhadra S. Acquiring Photoplethysmography (PPG) signal without LED. In: 2023 IEEE international instrumentation and measurement technology conference (I2MTC); 2023, May. p. 1–6. https://doi.org/10.1109/I2MTC53148.2023.10175960.
Silverio AA, Suarez CG, Silverio LAA, Dino JY, Duran JB, Catambing GEG. An unobtrusive, wireless and wearable single-site blood pressure monitor based on an armband using electrocardiography (ECG) and reflectance Photoplethysmography (PPG) signal processing. Electronics. 2023;12(7):1538. https://doi.org/10.3390/electronics12071538.
Ebrahimi Z, Gosselin B. Ultra-low power Photoplethysmography (PPG) sensors: a methodological review. IEEE Sensors J. 2023; https://doi.org/10.1109/jsen.2023.3284818.
Ebrahimkhani M, Johnson EM, Sodhi A, Robinson JD, Rigsby CK, Allen BD, Markl M. A deep learning approach to using wearable Seismocardiography (SCG) for diagnosing aortic valve stenosis and predicting aortic hemodynamics obtained by 4D flow MRI. Ann Biomed Eng. 2023;51(12):2802–11.
Balali P, Rabineau J, Hossein A, Tordeur C, Debeir O, Van De Borne P. Investigating cardiorespiratory interaction using ballistocardiography and seismocardiography—a narrative review. Sensors. 2022;22(23):9565. https://doi.org/10.3390/s22239565.
Ganti VG, Gazi AH, An S, Srivatsa AV, Nevius BN, Nichols CJ, Tandon A. Wearable Seismocardiography-based assessment of stroke volume in congenital heart disease. J Am Heart Assoc. 2022;11(18):e026067. https://doi.org/10.1161/JAHA.122.026067.
Peters C, Rocznik T, Yee SY, Duerichen R, Schnitzbauer VJ. Wearable health device system with normalized seismocardiography signals. U.S. patent application no. 16/975,010. 2021. https://patents.google.com/patent/US20210085216A1/.
Miljković, N., & Šekara, T. B. (2022). A new weighted time window-based method to detect B-point in ICG. https://arxiv.org/abs/2207.04490.
Chabchoub S, Mansouri S, Ben Salah R. Signal processing techniques applied to impedance cardiography ICG signals–a review. J Med Eng Technol. 2022;46(3):243–60. https://doi.org/10.1080/03091902.2022.2026508.
Cosoli G, Spinsante S, Scardulla F, D'Acquisto L, Scalise L. Wireless ECG and cardiac monitoring systems: state of the art, available commercial devices and useful electronic components. Measurement. 2021;177:109243. https://doi.org/10.1016/J.MEASUREMENT.2021.109243.
DeMarzo AP. Clinical use of impedance cardiography for hemodynamic assessment of early cardiovascular disease and management of hypertension. High Blood Pressure Cardiovasc Prevent. 2020;27(3):203–13. https://doi.org/10.1007/S40292-020-00383-0.
Min S, Kim DH, Joe DJ, Kim BW, Jung YH, Lee JH, Lee KJ. Clinical validation of a wearable piezoelectric blood-pressure sensor for continuous health monitoring. Adv Mater. 2023:2301627. https://doi.org/10.1002/adma.202301627.
El-Hajj C, Kyriacou PA. A review of machine learning techniques in photoplethysmography for the non-invasive cuff-less measurement of blood pressure. Biomed Signal Process Control. 2020;58:101870. https://doi.org/10.1016/j.bspc.2020.101870.
Wen L, Dong S, Zhang Z, Gu C, Mao J. Noninvasive continuous blood pressure monitoring based on wearable radar sensor with preliminary clinical validation. In: 2022 IEEE/MTT-S international microwave symposium-IMS 2022; 2022, June. p. 707–10. https://doi.org/10.1109/IMS37962.2022.9865440.
Islam SMS, Chow CK, Daryabeygikhotbehsara R, Subedi N, Rawstorn J, Tegegne T, et al. Wearable cuffless blood pressure monitoring devices: a systematic review and meta-analysis. Europ Heart J-Digital Health. 2022;3(2):323–37. https://doi.org/10.1093/ehjdh/ztac021.
Kumar A. Flexible and wearable capacitive pressure sensor for blood pressure monitoring. Sens Bio-Sens Res. 2021;33:100434. https://doi.org/10.1016/J.SBSR.2021.100434.
Athira S, Ardra S, Unnikrishnan A, Pradeep A, Rajeev SP, SD, B. S. Design of Piezoelectric Heart Rate Monitoring Sensor for wearable applications. In: 2022 IEEE 6th international conference on trends in electronics and informatics (ICOEI); 2022, April. p. 1–6. https://doi.org/10.1109/ICOEI53556.2022.9777147.
Hashim UN, Salahuddin L, Ikram RRR, Hashim UR, Ngo HC, Mohayat MHN. The design and implementation of Mobile heart monitoring applications using wearable heart rate sensor. Int J Adv Comput Sci Appl. 2021;12(1) https://doi.org/10.14569/IJACSA.2021.0120120.
Harraghy M, Calderon D, Lietz R, Brady J, Makedon F, Becker E. A review of wearable heart rate sensors in research. In: In proceedings of the 12th ACM international conference on PErvasive technologies related to assistive environments; 2019, June. p. 315–6. https://doi.org/10.1145/3316782.3321550.
Tang X, Yang A, Li L. Optimization of nanofiber wearable heart rate sensor module for human motion detection. Comput Mathematical Methods Med. 2022;2022. https://doi.org/10.1155/2022/1747822.
Shen S, Xiao X, Chen J. Wearable triboelectric nanogenerators for heart rate monitoring. Chem Commun. 2021;57(48):5871–9. https://doi.org/10.1039/D1CC02091A.
Huang N, Bian D, Zhou M, Mehta P, Shah M, Rajput KS, Selvaraj N. Pulse rate guided oxygen saturation monitoring using a wearable armband sensor. In: 2022 44th annual international conference of the IEEE engineering in Medicine & Biology Society (EMBC); 2022, July. p. 4303–7. https://doi.org/10.1109/EMBC48229.2022.9871461.
Phillips C, Liaqat D, Gabel M, de Lara E. WristO2: reliable peripheral oxygen saturation readings from wrist-worn pulse oximeters. In: 2021 IEEE international conference on Pervasive computing and communications workshops and other affiliated events (PerCom workshops); 2021, March. p. 623–9. https://doi.org/10.1109/PERCOMWORKSHOPS51409.2021.9430986.
Lim CJ, Park JW. Wearable transcutaneous oxygen sensor for health monitoring. Sensors Actuators A Phys. 2019;298:111607. https://doi.org/10.1016/J.SNA.2019.111607.
Patel V, Chesmore A, Legner CM, Pandey S. Trends in workplace wearable technologies and connected-worker solutions for next-generation occupational safety, health, and productivity. Adv Intelligent Syst. 2022;4(1):2100099. https://doi.org/10.1002/aisy.202100099.
Hearn EL, Byford J, Wolfe C, Agyei C, Hodkinson PD, Pollock RD, Smith TG. Measuring arterial oxygen saturation using wearable devices under varying conditions. Aerospace Med Human Perform. 2023;94(1):42–7. https://doi.org/10.3357/amhp.6078.2023.
Yi XI, Sun S, Su D. Wearable device and photoelectric pulse sensor component. U.S. patent application no. 17/622,517. 2022. https://patents.google.com/patent/US20220248968A1/.
Degala SKB, Pandey R, Mishra A, Tiwari AK, Tewari RP. IoT based low-cost pulse oximeter for remote health monitoring. In: International conference on advancements in interdisciplinary research. Cham: Springer Nature Switzerland; 2022, May. p. 191–8. https://doi.org/10.1007/978-3-031-23724-9_18.
Enoch AJ, English M, Shepperd S. Does pulse oximeter use impact health outcomes? A systematic review. Arch Dis Child. 2016;101(8):694–700. https://doi.org/10.1136/ARCHDISCHILD-2015-309638.
Boller, W. (2019). U.S. patent application no. 16/114,742.
Mota GC, López RL, Ramos CB. Pulse oximeter with internet data visualization. Sistemas Telemática. 2018;16(45):9–18. https://doi.org/10.18046/SYT.V16I45.2746.
Dolson CM, Harlow ER, Phelan DM, Gabbett TJ, Gaal B, McMellen C, Seshadri DR. Wearable sensor technology to predict Core body temperature: a systematic review. Sensors. 2022;22(19):7639. https://doi.org/10.3390/s22197639.
Kuzubasoglu BA, Sayar E, Cochrane C, Koncar V, Bahadir SK. Wearable temperature sensor for human body temperature detection. J Mater Sci Mater Electron. 2021;32:4784–97. https://doi.org/10.1007/S10854-020-05217-2.
Mansi SA, Barone G, Forzano C, Pigliautile I, Ferrara M, Pisello AL, Arnesano M. Measuring human physiological indices for thermal comfort assessment through wearable devices: a review. Measurement. 2021;183:109872. https://doi.org/10.1016/J.MEASUREMENT.2021.109872.
Henderson J, Condell J, Connolly J, Kelly D, Curran K. Review of wearable sensor-based health monitoring glove devices for rheumatoid arthritis. Sensors. 2021;21(5):1576. https://doi.org/10.3390/S21051576.
Duan Z, Jiang Y, Tai H. Recent advances in humidity sensors for human body related humidity detection. J Mater Chem C. 2021;9(42):14963–80. https://doi.org/10.1039/D1TC04180K.
Anisimov YA, Evitts RW, Cree DE, Wilson LD. Polyaniline/biopolymer composite systems for humidity sensor applications: a review. Polymers. 2021;13(16):2722. https://doi.org/10.3390/POLYM13162722.
Corchia L, Monti G, De Benedetto E, Tarricone L. A chipless humidity sensor for wearable applications. In: 2019 IEEE international conference on RFID technology and applications (RFID-TA); 2019, September. p. 174–7. https://doi.org/10.1109/RFID-TA.2019.8892048.
Nweke HF, Teh YW, Mujtaba G, Al-Garadi MA. Data fusion and multiple classifier systems for human activity detection and health monitoring: review and open research directions. Inform Fusion. 2019;46:147–70. https://doi.org/10.1016/j.inffus.2018.06.002.
Motti VG, Motti VG. Introduction to wearable computers. In: Wearable Interaction. Springer; 2020. p. 1–39.
Awolusi I, Marks E, Hallowell M. Wearable technology for personalized construction safety monitoring and trending: review of applicable devices. Autom Constr. 2018;85:96–106. https://doi.org/10.1016/j.autcon.2017.10.010.
Khurshid S, Weng LC, Nauffal V, Pirruccello JP, Venn RA, Al-Alusi MA, Lubitz SA. Wearable accelerometer-derived physical activity and incident disease. NPJ Digital Med. 2022;5(1):131. https://doi.org/10.1038/s41746-022-00676-9.
Rojas E, Schmidt SL, Chowdhury A, Pajic M, Turner DA, Won DS. A comparison of an implanted accelerometer with a wearable accelerometer for closed-loop DBS. In: 2022 44th annual international conference of the IEEE engineering in Medicine & Biology Society (EMBC); 2022, July. p. 3439–42. https://doi.org/10.1109/EMBC48229.2022.9871232.
Davoudi A, Manini TM, Bihorac A, Rashidi P. Role of wearable accelerometer devices in delirium studies: a systematic review. Critic Care Explor. 2019;1(9) https://doi.org/10.1097/CCE.0000000000000027.
Xia C, Sugiura Y. Wearable accelerometer optimal positions for human motion recognition. In: 2020 IEEE 2nd global conference on life sciences and technologies (LifeTech); 2020, March. p. 19–20. https://doi.org/10.1109/LIFETECH48969.2020.1570618961.
Veluvolu KC. Wearable accelerometer based Pseudo-ECG generation. In: 2019 international conference on data science and communication (IconDSC); 2019, March. p. 1–4. https://doi.org/10.1109/ICONDSC.2019.8817000.
Saifuzzaman M, Ananna TN, Chowdhury MJM, Ferdous MS, Chowdhury F. A systematic literature review on wearable health data publishing under differential privacy. Int J Inf Secur. 2022;21(4):847–72. https://doi.org/10.1007/s10207-021-00576-1.
Li C, Lin SH, Chib A. The state of wearable health technologies: a transdisciplinary literature review. Mobile Media Commun. 2021;9(2):353–76. https://doi.org/10.1177/2050157920966023.
Trovato V, Sfameni S, Rando G, Rosace G, Libertino S, Ferri A, Plutino MR. A review of stimuli-responsive smart materials for wearable Technology in Healthcare: retrospective, perspective, and prospective. Molecules. 2022;27(17):5709. https://doi.org/10.3390/molecules27175709.
Shin G, Jarrahi MH, Fei Y, Karami A, Gafinowitz N, Byun A, Lu X. Wearable activity trackers, accuracy, adoption, acceptance and health impact: a systematic literature review. J Biomed Inform. 2019;93:103153. https://doi.org/10.1016/j.jbi.2019.103153.
Jin Z, Lee C, Zhang K, Jeong R, Gan TJ, Richman DC. Utilization of wearable pedometer devices in the perioperative period: a qualitative systematic review. Anesth Analg. 2023;136(4):646–54. https://doi.org/10.1213/ANE.0000000000006353.
Cheng Y, Wang K, Xu H, Li T, Jin Q, Cui D. Recent developments in sensors for wearable device applications. Anal Bioanal Chem. 2021;413(24):6037–57. https://doi.org/10.1007/S00216-021-03602-2.
Lin X, Luo J, Liao M, Su Y, Lv M, Li Q, Xiang J. Wearable sensor-based monitoring of environmental exposures and the associated health effects: a review. Biosensors. 2022;12(12):1131. https://doi.org/10.3390/bios12121131.
Yulianti ES, Intan N, Rahman SF, Basari B. Sweat sensing in wearable sensor: a review of the future non-invasive technology for real-time health monitoring system. AIP Conf Proc. 2022, August;2537(1). https://doi.org/10.1063/5.0097942.
Sharma Y, Djambazova KV, Marquez CD, Lyden K, Goldsack JC, Bakker JP. A systematic review assessing the state of analytical validation for connected, mobile, sensor-based digital health technologies. medRxiv. 2023. https://doi.org/10.1101/2023.05.22.23290371.
Zahid M, Rathore HA, Tayyab H, Rehan ZA, Rashid IA, Lodhi M, et al. Recent developments in textile based polymeric smart sensor for human health monitoring: a review. Arab J Chem. 2022;15(1):103480. https://doi.org/10.1016/J.ARABJC.2021.103480.
Long N, Lei Y, Peng L, Xu P, Mao P. A scoping review on monitoring mental health using smart wearable devices. Math Biosci Eng. 2022;19(8):7899–919. https://doi.org/10.3934/mbe.2022369.
Devi MP, Sathya T, Raja GB. Remote Human’s health and activities monitoring using wearable sensor-based system—a review. In: Efficient Data Handling for Massive Internet of Medical Things: Healthcare Data Analytics; 2021. p. 203–28. https://doi.org/10.1007/978-3-030-66633-0_9.
Vijayan V, Connolly JP, Condell J, McKelvey N, Gardiner P. Review of wearable devices and data collection considerations for connected health. Sensors. 2021;21(16):5589. https://doi.org/10.3390/S21165589.
Kim H, Song J, Kim S, Lee S, Park Y, Lee S, Kim J. Recent advances in multiplexed wearable sensor platforms for real-time monitoring lifetime stress: a review. Biosensors. 2023;13(4):470. https://doi.org/10.3390/bios13040470.
Rashid N, Mortlock T, Al Faruque MA. Stress detection using context-aware sensor fusion from wearable devices. IEEE Internet Things J. 2023. https://doi.org/10.1109/jiot.2023.3265768.
Namvari M, Lipoth J, Knight S, Jamali AA, Hedayati M, Spiteri RJ, Syed-Abdul S. Photoplethysmography enabled wearable devices and stress detection: a scoping review. J Personal Med. 2022;12(11):1792. https://doi.org/10.3390/jpm12111792.
Zheng H, Wang H, Yi K, Lin J, Chen A, Chen L, Lin Z. Wearable LIG flexible stress sensor based on spider web bionic structure. Coatings. 2023;13(1):155. https://doi.org/10.3390/coatings13010155.
Imura I, Gotoh Y, Sakai K, Ohara Y, Tazoe J, Miura H, Nomura Y. A method for estimating physician stress using wearable sensor devices. Sens Mater. 2022;34. https://doi.org/10.18494/sam3908.
Zijie F, Al-Shareeda MA, Saare MA, Manickam S, Karuppayah S. Wireless sensor networks in the internet of things: review, techniques, challenges, and future directions. Indonesian J Electric Eng Comput Sci. 2023;31(2):1190–200. https://doi.org/10.11591/ijeecs.v31.i2.pp1190-1200.
Schnell B, Moder P, Ehm H, Konstantinov M, Ismail M. Challenges in smart health applications using wearable medical internet-of-things—a review. In: In proceedings of sixth international congress on information and communication technology: ICICT 2021, London, volume 3. Singapore: Springer; 2022. p. 283–96. https://doi.org/10.1007/978-981-16-1781-2_27.
Singh A. A review about wireless sensor networks and the internet of things. J Internet Things. 2022;4(2). https://doi.org/10.32604/jiot.2022.026170.
Wang Y, Li T, Li Y, Yang R, Zhang G. 2D-materials-based wearable biosensor systems. Biosensors. 2022;12(11):936. https://doi.org/10.3390/bios12110936.
Zhang Y, Hu Y, Jiang N, Yetisen AK. Wearable artificial intelligence biosensor networks. Biosens Bioelectron. 2022:114825. https://doi.org/10.1016/j.bios.2022.114825.
Pai M, Batakurki S, Adimule V, Yallur BC. Optical graphene for biosensor application: a review. Appl Mech Mater. 2022;908:51–68. https://doi.org/10.4028/p-rs3qal.
Banerjee A, Maity S, Mastrangelo CH. Nanostructures for biosensing, with a brief overview on cancer detection, IoT, and the role of machine learning in smart biosensors. Sensors. 2021;21(4):1253. https://doi.org/10.3390/s21041253.
Zhu Y, Mo L. A review of wearable sensor-based human activity recognition using deep learning. In: 2022 IEEE international conference on sensing, Measurement & Data Analytics in the era of artificial intelligence (ICSMD); 2022, November. p. 1–6. https://doi.org/10.1109/ICSMD57530.2022.10058422.
Chitra B, Kumar VA. A comprehensive review: cardiac disease detection using IoT based wearable sensor and deep learning techniques. In: 2022 IEEE third international conference on intelligent computing instrumentation and control technologies (ICICICT); 2022, August. p. 924–30. https://doi.org/10.1109/ICICICT54557.2022.9917731.
Zhang S, Suresh L, Yang J, Zhang X, Tan SC. Augmenting sensor performance with machine learning towards smart wearable sensing electronic systems. Adv Intelligent Syst. 2022;4(4):2100194. https://doi.org/10.1002/aisy.202270016.
Soangra R, Sivakumar R, Anirudh ER, Reddy YSV, John EB. Evaluation of surgical skill using machine learning with optimal wearable sensor locations. PLoS One. 2022;17(6):e0267936. https://doi.org/10.1371/journal.pone.0267936.
Jing W, Xiaolong Z. Wearable sensor-based motion data analysis and dance performance using images and cloud computing. Mob Inf Syst. 2022;2022. https://doi.org/10.1155/2022/4305073.
Joshi J, Kurian D, Bhasin S, Mukherjee S, Awasthi P, Sharma S, Mittal S. Health monitoring using wearable sensor and cloud computing. In: 2016 IEEE international conference on cybernetics, robotics and control (CRC); 2016, August. p. 104–8. https://doi.org/10.1109/CRC.2016.031.
Panigrahi CR, Sarkar JL, Pati B, Buyya R, Mohapatra P, Majumder A. Mobile cloud computing and wireless sensor networks: a review, integration architecture, and future directions. IET Networks. 2021;10(4):141–61. https://doi.org/10.1049/NTW2.12013.
Fortino G, Gravina R, Galzarano S. Wearable computing: from modeling to implementation of wearable systems based on body sensor networks. John Wiley & Sons; 2018.
Doukas C, Maglogiannis I. Managing wearable sensor data through cloud computing. In: 2011 IEEE third international conference on cloud computing technology and science; 2011, November. p. 440–5. https://doi.org/10.1109/CLOUDCOM.2011.65.
Elsevier. Data | Curated. Connected Complete Elseviercom Published 2019. https://www.elsevier.com/solutions/scopus
Clarivate. Web of Science - Web of Science Group. Web of Science Group. Published 2019. https://clarivate.com/webofsciencegroup/solutions/web-of-science/
Mongeon P, Paul-Hus A. The journal coverage of web of science and Scopus: a comparative analysis. Scientometrics. 2016;106(1):213–28. https://doi.org/10.1007/s11192-015-1765-5.
Azliyana A, Zaki A. Educational insights from bibliometric patterns: examining depression research in Malaysia. Asian J Res Educ Soc Sci. 2023;5(3):33–47. https://myjms.mohe.gov.my/index.php/ajress/article/view/23192
Azizan A, Abdullah KH, Rahayu SR, Rusli NS, Tarmidzi N. Reshaping healthcare: a bibliometric analysis of lessons learned in post-COVID-19 health policy. Kesmas. 2023;18(3):18–24. https://doi.org/10.21109/kesmas.v18i3.7060.
Hou H, Kretschmer H, Liu Z. The structure of scientific collaboration networks in Scientometrics. Scientometrics. 2007;75(2):189–202. https://doi.org/10.1007/s11192-007-1771-3.
Hu CP, Hu JM, Deng SL, Liu Y. A co-word analysis of library and information science in China. Scientometrics. 2013;97(2):369–82. https://doi.org/10.1007/s11192-013-1076-7.
van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2009;84(2):523–38. https://doi.org/10.1007/s11192-009-0146-3.
Pantelopoulos A, Bourbakis NG. A survey on wearable sensor-based systems for health monitoring and prognosis. IEEE Trans Syst Man Cybern Part C Appl Rev. 2010;40(1):1–12. https://doi.org/10.1109/tsmcc.2009.2032660.
Majumder S, Mondal T, Deen M. Wearable sensors for remote health monitoring. Sensors. 2017;17(12):130. https://doi.org/10.3390/s17010130.
Banaee H, Ahmed M, Loutfi A. Data Mining for Wearable Sensors in health monitoring systems: a review of recent trends and challenges. Sensors. 2013;13(12):17472–500. https://doi.org/10.3390/s131217472.
Neethirajan S. Recent advances in wearable sensors for animal health management. Sens Bio-Sens Res. 2017;12:15–29. https://doi.org/10.1016/j.sbsr.2016.11.004.
Kakria P, Tripathi NK, Kitipawang P. A real-time health monitoring system for remote cardiac patients using smartphone and wearable sensors. Int J Telemed Appl. 2015;2015:1–11. https://doi.org/10.1155/2015/373474.
Rodgers MM, Pai VM, Conroy RS. Recent advances in wearable sensors for health monitoring. IEEE Sensors J. 2015;15(6):3119–26. https://doi.org/10.1109/jsen.2014.2357257.
Al-khafajiy M, Baker T, Chalmers C, Asim M, Kolivand H, Fahim M, Waraich A. Remote health monitoring of elderly through wearable sensors. Multimed Tools Appl. 2019;78(17):24681–706. https://doi.org/10.1007/s11042-018-7134-7.
Sano A, Taylor S, McHill AW, Phillips AJ, Barger LK, Klerman E, Picard R. Identifying objective physiological markers and modifiable behaviors for self-reported stress and mental health status using wearable sensors and Mobile phones: observational study. J Med Internet Res. 2018;20(6):e210. https://doi.org/10.2196/jmir.9410.
Wang Y, Cang S, Yu H. A survey on wearable sensor modality centred human activity recognition in health care. Expert Syst Appl. 2019;137:167–90. https://doi.org/10.1016/j.eswa.2019.04.057.
Jarneving B. Bibliographic coupling and its application to research-front and other core documents. J Informetrics. 2007;1(4):287–307. https://doi.org/10.1016/j.joi.2007.07.004.
Acknowledgements
Authors acknowledge the Universiti Teknologi MARA for funding under the Geran Penyelidikan Inovasi Sosial 600-RMC/GIS 5/3 (006/2023).
Author information
Authors and Affiliations
Contributions
AA – Writing - original draft preparation, methodology, formal analysis, and funding acquisition. WA – Writing - review and editing, and investigation. AHAR – Conceptualization, writing - review and editing, and investigation. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Azizan, A., Ahmed, W. & Razak, A.H.A. Sensing health: a bibliometric analysis of wearable sensors in healthcare. Health Technol. 14, 15–34 (2024). https://doi.org/10.1007/s12553-023-00801-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-023-00801-y