Abstract
Background
Hematopoietic stem cell transplantation (hereafter “HCT”) is a physically and psychologically difficult treatment for patients with hematological cancers. This study examined relationships among patients’ reports of pre-transplant social isolation, social constraints, and psychological distress.
Method
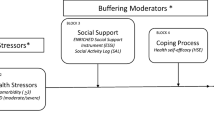
We used baseline data from a multisite randomized controlled trial evaluating the effects of expressive helping writing to reduce physical and emotional symptoms in HCT patients. We collected data prior to randomization and before either allogenic or autologous HCT using validated scales to assess social constraints, social isolation, anxiety, and depressive symptoms. We analyzed data using bivariate analysis and multivariate linear regression. We also explored whether social isolation mediated the effect of social constraints on both of our outcomes: anxiety and depressive symptoms.
Results
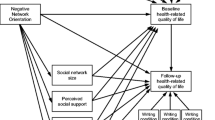
Among 259 adults recruited prior to transplant, 43.6% were women (mean age = 57.42 years, SD = 12.34 years). In multivariate analysis controlling for relevant covariates, both social isolation (β = 0.24, p < 0.001) and social constraints (β = 0.28, p < 0.001) were associated with anxiety. When both social constraints and social isolation were in the model, only greater social isolation (β = 0.79, p < 0.001) was associated with depressive symptoms. Social isolation fully mediated the association between social constraints and anxiety and depressive symptoms.
Conclusion
For patients awaiting either allogenic or autologous HCT, the negative association between social constraints and anxiety and depressive symptoms may be related, in part, to the mechanism of perceived social isolation. Interventions prior to and during HCT are needed to support patients’ psychological health and sense of social connectedness.



Similar content being viewed by others
Data Availability
For access to the data that supports our findings, individuals outside of the study team may submit a formal request, which will be reviewed by the executive committee. To ensure confidentiality, datasets distributed to any of these individuals will be de-identified by removing any identifying participant information.
References
Leukemia & Lymphoma Society. Facts and statistics overview. 2021. https://www.lls.org/facts-and-statistics/facts-and-statistics-overview#:~:text=Approximately%20every%203%20minutes%2C%20one%20person%20in%20the,diagnosed%20with%20leukemia%2C%20lymphoma%20or%20myeloma%20in%202021. Accessed 10 Aug 2022.
Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006;354(17):1813–26.
Hatzimichael E, Tuthill M. Hematopoietic stem cell transplantation. Stem Cells Cloning: Adv Appl. 2010;3:105–17.
Farhadfar N, Weaver MT, Al-Mansour Z, et al. Self-efficacy for symptom management in long-term adult hematopoietic stem cell survivors. Transplant Cell Ther. 2022;28(9):606.e1-606.e8.
CIBMTR. The US summary slides – HCT trends and survival data. https://www.cibmtr.org/ReferenceCenter/SlidesReports/SummarySlides/pages/index.aspx. Accessed 8 Dec 2022.
El-Jawahri AR, Vandusen HB, Traeger LN, et al. Quality of life and mood predict posttraumatic stress disorder after hematopoietic stem cell transplantation. Cancer. 2016;122(5):806–12.
Smith SR, Hobson ME, Haig AJ. Distress prior to undergoing hematopoietic stem cell transplantation: demographic and symptom correlations and establishing a baseline. Patient Relat Outcome Meas. 2016;7:137–44.
El-Jawahri A, Traeger L, Kuzmuk K, et al. Prognostic understanding, quality of life and mood in patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant. 2015;50(8):1119–24.
Wells KJ, Booth-Jones M, Jacobsen PB. Do coping and social support predict depression and anxiety in patients undergoing hematopoietic stem cell transplantation? J Psychosoc Oncol. 2009;27(3):297–315.
Amonoo HL, Johnson PC, Dhawale TM, et al. Sharing and caring: the impact of social support on quality of life and health outcomes in hematopoietic stem cell transplantation. Cancer. 2021;127(8):1260–5.
Beattie S, Lebel S, Tay J. The influence of social support on hematopoietic stem cell transplantation survival: a systematic review of literature. PLoS ONE. 2013;8(4): e61586.
Lepore SJ, Revenson TA. Social constraints on disclosure and adjustment to cancer. Soc Personal Psychol Compass. 2007;1(1):313–33.
Hyland KA, Small BJ, Gray JE, et al. Loneliness as a mediator of the relationship of social cognitive variables with depressive symptoms and quality of life in lung cancer patients beginning treatment. Psychooncology. 2019;28(6):1234–42.
Mosher CE, Lepore SJ, Wu L, et al. Social correlates of distress following hematopoietic stem cell transplantation: exploring the role of loneliness and cognitive processing. J Health Psychol. 2012;17(7):1022–32.
Lepore SJ. A social–cognitive processing model of emotional adjustment to cancer. In: Baum A, Andersen BL, editors. Psychosocial interventions for cancer. American Psychological Association; 2001. p. 99–116.
Rivera-Rivera JN, Badour CL, Burris JL. The association between psychological functioning and social support and social constraint after cancer diagnosis: a 30-day daily diary study. J Behav Med. 2021;44:355–67.
Liang Y, Hao G, Wu M, Hou L. Social isolation in adults with cancer: an evolutionary concept analysis. Front Psychol. 2022;13: 973640.
Health Measures. PROMIS social isolation. 2015. http://www.healthmeasures.net/images/promis/manuals/PROMIS_Social_Isolation_Scoring_Manual.pdf. Accessed 8 Dec 2022.
Primack BA, Shensa A, Sidani JE, Whaite EO, Lin LY, Rosen D, Colditz JB, Radovic A, Miller E. Social media use and perceived social isolation among young adults in the U.S. Am J Prev Med. 2017;53(1):1–8.
Richardson A, König HH, Hajek A. Volunteering, loneliness and perceived social isolation: evidence from a representative sample of middle-aged and older adults in Germany. Aging Ment Health. 2023;14:1–6.
O’Sullivan R, Burns A, Leavey G, Leroi I, Burholt V, Lubben J, Holt-Lunstad J, Victor C, Lawlor B, Vilar-Compte M, Perissinotto CM, Tully MA, Sullivan MP, Rosato M, Power JM, Tiilikainen E, Prohaska TR. Impact of the COVID-19 pandemic on loneliness and social isolation: a multi-country study. Int J Environ Res Public Health. 2021;18(19):9982.
Brandão T. A systematic review on social constraints in the context of cancer. Psychol Health Med. 2021;26(7):787–804.
Shen Z, Xie J, Ruan C, Li C. Mediating effect of ill perception on the relationship between social constraints and fear of cancer recurrence among adolescent and young adult survivors who underwent hematopoietic stem cell transplantation. Asia Pac J Oncol Nurs. 2022;9(5): 100060.
Llave K, Hoyt MA. Social constraints and cancer-related quality of life in single and partnered young adult testicular cancer survivors: a contextual approach. J Psychosoc Oncol. 2022;40(6):743–55.
Whitmore L, Schulte T, Bovbjerg K, et al. Efficacy of expressive helping in adult hematologic cancer patients undergoing stem cell transplant: protocol for the Writing for Insight, Strength, and Ease (WISE) study’s two-arm randomized controlled trial. Trials. 2021;22:722.
Rini C, Austin J, Wu LM, et al. Harnessing benefits of helping others: a randomized controlled trial testing expressive helping to address survivorship problems after hematopoietic stem cell transplant. Health Psychol. 2014;33(12):1541-51.
Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94.
Best AL, Roberson ML, Plascak JJ, et al. Structural racism and cancer: calls to action for cancer researchers to address racial/ethnic cancer inequity in the United States. Cancer Epidemiol Biomarkers Prev. 2022;31(6):1243–6.
Flanagin A, Frey T, Christiansen SL, AMA Manual of Style Committee. Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. JAMA. 2021;326(7):621–627.
Hahn EA, Beaumont JL, Pilkonis PA, et al. The PROMIS satisfaction with social participation measures demonstrated responsiveness in diverse clinical populations. J Clin Epidemiol. 2016;73:135–41.
Hahn EA, DeWalt DA, Bode RK, et al. New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychol. 2014;33(5):490–9.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7.
Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–25.
Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–74.
Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients. Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). J. Psychosom. Res. 1999;46:437–443.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach (3rd edition). New York, NY: The Guilford Press; 2022.
Cavalcanti IDL, Soares JCS. Impact of COVID-19 on cancer patients: a review. Asia Pac J Clin Oncol. 2021;17(3):186–92.
Mihic-Góngora L, Rodriguez-Gonzalez A, Velasco V, et al. Impact of the COVID-19 pandemic on care and psychological impact on cancer patients. Curr Opin Support Palliat Care. 2022;16(3):138–43.
Arrato NA, Lo SB, Coker CA, et al. Cancer treatment during COVID-19: resilience of individuals with advanced non-small cell lung cancer versus community controls. J Natl Compr Canc Netw. 2022;20(2):118–25.
Rotz SJ, Yi JC, Hamilton BK, et al. Health-related quality of life in young adult survivors of hematopoietic cell transplantation. Transplant Cell Ther. 2022;28(10):701.e1-701.e7.
Janicsák H, Ungvari GS, Gazdag G. Psychosocial aspects of hematopoietic stem cell transplantation. World J Transplant. 2021;11(7):263–76.
Jaremka LM, Andridge RR, Fagundes CP, et al. Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol: Off J Div Health Psychol, Am Psychol Assoc. 2014;33(9):948–57.
Yanez B, Taub CJ, Waltz M, et al. Stem cell transplant experiences among Hispanic/Latinx patients: a qualitative analysis. Int J Behav Med. 2022:1–11.
Kim WS, Langer S, Todd M, et al. Feasibility of a digital storytelling intervention for hematopoietic cell transplant patients. J Cancer Educ. 2022;37(5):1275–85.
Bovbjerg K, Graves K, Waltz M, et al. Expanding access to cancer peer support: development of a website to deliver written peer support that meets patients’ individual emotional and informational needs while reducing potential harms. Procedia Comput Sci. 2022;206:195–205.
Acknowledgements
We wish to thank all of the study participants who contributed their time to study activities prior to a hematopoietic stem cell transplant. Thank you to Lauren Whitmore, MS, Taylor Schulte, MS, Rebecca Thompson, BS, Madison Hartstein, BS, Kendyll Poth, MS, and Joanne Assarsson, LCSW for their support of this work.
Funding
This study was funded by the National Cancer Institute of the National Institutes of Health under award number R01CA223963 (PI: Rini). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding body had no role in the study design, data collection and analysis, decision to publish, or preparation of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval and Consent to Participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study has been approved by the Georgetown-MedStar Institutional Review Board (#2018–1306) and has received administrative approval from the review boards at all study sites. All participants completed an informed consent document to participate. Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shahrour, L., Martinez, J., Chicaiza, A. et al. Greater Social Isolation and Social Constraints Prior to Hematopoietic Stem Cell Transplant Are Associated with Greater Anxiety and Depressive Symptoms. Int.J. Behav. Med. (2023). https://doi.org/10.1007/s12529-023-10232-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s12529-023-10232-8