Abstract
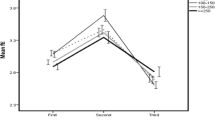
The study aims to establish trimester-specific reference ranges for serum iodine (SI) in Chinese pregnant women and explore its associations with maternal and infantile thyroid function. Apparently healthy pregnant women were enrolled during their first antenatal visit. Fasting venous and spot urine samples were collected for determining serum and urinary iodine (UI) levels by a validated inductively coupled plasma mass spectrometry. Serum free triiodothyronine (FT3), free thyroxine (FT4), thyrotropin (TSH), and neonatal TSH levels were tested by electro-chemiluminescent assay. The reference ranges of SI were established by percentile method and reported as 2.5–97.5%. ROC analysis was applied to compare the discriminative ability of SI, UI, and UI to urinary creatine ratio (UI /UCr) in early pregnancy for various thyroid conditions. The trimester-specific reference ranges of SI for Chinese pregnant women were 60.91–114.53 μg/L for the first trimester (T1, n = 1029), 54.57–103.42 μg/L for the second trimester (T2, n = 379), and 52.03–110.40 μg/L for the third trimester (T3, n = 455). Maternal SI at T1 but not UI and UI/UCr was significantly correlated with FT3 (r = 0.393, P < 0.001), FT4 (r = 0.637, P < 0.001), and TSH (r = −0.299, P<0.001). Maternal SI change% from T1 to T2 (but not SI change% from T1 to T3) had marginal correlation with neonatal TSH (r=−0.106, P=0.046). ROC analysis showed that maternal SI at T1 had better predictability for several thyroid conditions than UIC and UI/UCr.

Similar content being viewed by others
Data Availability
The original datasets are not publicly available due to ethical limitations publishing medical record data, but available from the corresponding author on reasonable request under strict confidential process.
References
Rodriguez-Diaz E, Pearce EN (2020) Iodine status and supplementation before, during, and after pregnancy. Best Pract Res Clin Endocrinol Metab 34(4):101430. https://doi.org/10.3945/jn.113.181974
WHO (2014) Guidelines approved by the Guidelines Review Committee. In: Guideline: fortification of food-grade salt with iodine for the prevention and control of iodine deficiency disorders. World Health Organization Copyright © World Health Organization 2014, Geneva
Pearce EN, Andersson M, Zimmermann MB (2013) Global iodine nutrition: where do we stand in 2013? Thyroid 23:523–528. https://doi.org/10.1089/thy.2013.0128
Nazarpour S, Ramezani Tehrani F, Behboudi-Gandevani S, Bidhendi Yarandi R, Azizi F (2020) Maternal urinary iodine concentration and pregnancy outcomes in euthyroid pregnant women: a systematic review and meta-analysis. Biol Trace Elem 197(2):411–420. https://doi.org/10.1007/s12011-019-02020-x
Zimmermann MB, Andersson M (2012) Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev 70(10):553–570. https://doi.org/10.1111/j.1753-4887.2012.00528.x
Doggui R, El Ati-Hellal M, Traissac P, El Ati J (2018) Pre-analytical factors influence accuracy of urine spot iodine assessment in epidemiological surveys. Biol Trace Elem Res 186(2):337–345. https://doi.org/10.1007/s12011-018-1317-y
Shi X, Han C, Li C, Mao J, Wang W, Xie X, Li C, Xu B, Meng T, Du J, Zhang S, Gao Z, Zhang X, Fan C, Shan Z, Teng W (2015) Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J Clin Endocrinol Metab 100(4):1630–1638. https://doi.org/10.1210/jc.2014-3704
König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB (2011) Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J Nutr 141(11):2049–2054. https://doi.org/10.3945/jn.111.144071
Pearce, E. N.; Caldwell, K. L., Urinary iodine, thyroid function, and thyroglobulin as biomarkers of iodine status. The American journal of clinical nutrition 2016, 104 Suppl 3 (Suppl 3), 898s-901s. https://doi.org/10.3945/ajcn.115.110395
Allain P, Berre S, Krari N, Lainé-Cessac P, Le Bouil A, Barbot N, Rohmer V, Bigorgne JC (1993) Use of plasma iodine assay for diagnosing thyroid disorders. J Clin Pathol 46(5):453–455. https://doi.org/10.1136/jcp.46.5.453
Michalke B, Witte H (2015) Characterization of a rapid and reliable method for iodide biomonitoring in serum and urine based on ion chromatography-ICP-mass spectrometry. J Trace Elem Med Biol 29:63–68. https://doi.org/10.1016/j.jtemb.2014.05.002
Liu ZM, Li G, Wu Y, Zhang D, Zhang S, Hao YT, Chen W, Huang Q, Li S, Xie Y, Ye M, He C, Chen P, Pan W (2022) Increased central and peripheral thyroid resistance indices during the first half of gestation were associated with lowered risk of gestational diabetes-analyses based on Huizhou birth cohort in South China. Front Endocrinol (Lausanne) 13:806256. https://doi.org/10.3389/fendo.2022.806256
Yu S, Yin Y, Cheng Q, Han J, Cheng X, Guo Y, Sun D, Xie S, Qiu L (2018) Validation of a simple inductively coupled plasma mass spectrometry method for detecting urine and serum iodine and evaluation of iodine status of pregnant women in Beijing. Scand J Clin Lab Invest 78(6):501–507. https://doi.org/10.1080/00365513.2018.1512150
C, B. J. (2010) Defining, establishing, and verifying reference intervals in the clinical laboratory; approved guidelines. CLSI Document 28(30):C28–CA3 https://community.clsi.org/media/1421/ep28a3c_sample.pdf
WHO/UNICEF/ICCIDD (2007). Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, 3rd ed (who.int). WHO Press, https://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827. Accessed 14 Sept 2023.
Yu S, Wang D, Cheng X, Zhang Q, Wang M, Guo H, Yu B, Zhang X, Xia L, Sun D, Cheng Q, Li P, Yin Y, Ma C, Hou L, Zou Y, Li H, Li D, Qiu L, Ichihara K (2020) Establishing reference intervals for urine and serum iodine levels: a nationwide multicenter study of a euthyroid Chinese population. Clin Chim Acta 502:34–40. https://doi.org/10.1016/j.cca.2019.11.038
Li C, Peng S, Zhang X, Xie X, Wang D, Mao J, Teng X, Shan Z, Teng W (2016) The urine iodine to creatinine as an optimal index of iodine during pregnancy in an iodine adequate area in China. J Clin Endocrinol Metab 101(3):1290–1298. https://doi.org/10.1210/jc.2015-3519
Pan Z, Cui T, Chen W, Gao S, Pearce EN, Wang W, Chen Y, Guo W, Tan L, Shen J, Zhang W (2019) Serum iodine concentration in pregnant women and its association with urinary iodine concentration and thyroid function. Clin Endocrinol (Oxf) 90(5):711–718. https://doi.org/10.1111/cen.13945
Cui T, Wang W, Chen W, Pan Z, Gao S, Tan L, Pearce EN, Zimmermann MB, Shen J, Zhang W (2019) Serum iodine is correlated with iodine intake and thyroid function in school-age children from a sufficient-to-excessive iodine intake area. J Nutr 149(6):1012–1018. https://doi.org/10.1093/jn/nxy325
Han JH, Wu L, Yu SL, Fang HL, Kamg WM, Cheng XQ, Lu J, Yu JC, Qiu L (2015) Values of iodine metabolism biomarkers in assessing the iodine nutrition status in surgically treated patients with thyroid disease. Zhongguo yi xue ke xue yuan xue bao Acta Academiae Medicinae Sinicae 37(2):221–225. https://doi.org/10.3881/j.issn.1000-503X.2015.02.014
Liberman CS, Pino SC, Fang SL, Braverman LE, Emerson CH (1998) Circulating iodide concentrations during and after pregnancy. J Clin Endocrinol Metab 83(10):3545–3549. https://doi.org/10.1210/jcem.83.10.5163
Manousou S, Eggertsen R, Hulthén L, Filipsson Nyström H (2021) A randomized, double-blind study of iodine supplementation during pregnancy in Sweden: pilot evaluation of maternal iodine status and thyroid function. Eur J Nutr 60(6):3411–3422. https://doi.org/10.1007/s00394-021-02515-1
Chan SS, Hams G, Wiley V, Wilcken B, McElduff A (2003) Postpartum maternal iodine status and the relationship to neonatal thyroid function. Thyroid : official journal of the American Thyroid Association 13(9):873–876. https://doi.org/10.1089/105072503322401078
Jaruratanasirikul S, Chukamnerd J, Koranantakul O, Chanvitan P, Ruaengrairatanaroj P, Sriplung H (2006) The relationship of maternal iodine status and neonatal thyrotropin concentration: a study in Southern Thailand. J Pediatr Endocr Met 19(5):727–732. https://doi.org/10.1515/jpem.2006.19.5.727
Candido AC, Vieira AA, de Souza Ferreira E, Moreira TR, do Carmo Castro Franceschini S, Cotta RMM (2022) Prevalence of excessive iodine intake in pregnancy and its health consequences: systematic review and meta-analysis. Biol Trace Elem Res. https://doi.org/10.1007/s12011-022-03401-5
Acknowledgments
Both ZML and YW conceptualized the topic, made results explanation, and drafted the manuscript; HHL, SJZ, and MML researched data, made data collection and analysis; Dr. WJP coordinated the study investigation and approved data utility; CGC, CW, YBY, ZYS, and SYZ provided professional consultations, helped in data interpretation, critically reviewed, and commented on the manuscript. All authors read and approved the final manuscript.
We are grateful to research members for their efforts in field investigation and data collection. We greatly appreciate the doctors and nurses in the Huizhou Hospital for their keen assistance in facilitating participants’ recruitment and investigation and data coordination. We acknowledge the Department of Clinical Laboratory and Department of Hospital Information Management of Huizhou First Mother-infant Hospital for providing great support in analyzing bio-specimens and approval of the data utility.
Funding
The research was funded by the “Hundred Talents Program” of Sun Yat-sen University (Grant No: 51000-18841203) and the National Natural Science Foundation of China (NSFC, No.82073533).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by The Ethics Committees of Huizhou First Mother and Child Health-care Hospital (protocol code: 2018002 and date of approval: 9, March, 2018).
Consent to Participate
Informed consent has been obtained from all women at enrolment in the Huizhou Birth Cohort.
Conflict of Interest
The authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, Y., Long, Hh., Zhang, Sj. et al. Reference Intervals of Serum Iodine Concentration in Chinese Pregnant Women. Biol Trace Elem Res 202, 2457–2465 (2024). https://doi.org/10.1007/s12011-023-03859-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-023-03859-x