Abstract
Purpose of review
The number of cancer patients grows globally. An important subset may develop heart failure.
Recent findings
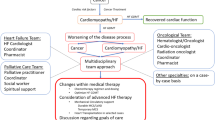
A paucity of data exists regarding outcomes and response to traditional intervention in cancer patients who develop heart failure. Advanced HF treatments in this population require special considerations. Since cancer treatment schedules are anticipated, emphasis should be placed on preventive interventions. Once left ventricular dysfunction ensues, early recognition and prompt treatment of heart failure may improve prognosis. Small studies have shown that guideline-directed medical therapies, cardiac resynchronization therapy, and implantable cardiac defibrillators are equally beneficial in cancer patients yet underutilized as a result of late recognition of heart failure and/or misconception of oncologic prognosis. Additionally, in carefully selected cancer survivors, clinical outcome after implantation of a left ventricular assist device and heart transplantation are comparable with other causes of heart failure.
Summary
Cancer survivors with acceptable prognosis should be evaluated for HF therapies in a timely manner. There remains an urgent need for larger-scale longitudinal studies to determine the best treatment strategies for heart failure in this population.
Similar content being viewed by others
Abbreviations
- ACE-inhibitor:
-
Angiotensin converter enzyme-inhibitor
- ARNI:
-
Angiotensin receptor blocker neprilysin inhibitor
- CCMP:
-
Chemotherapy induced cardiomyopathy
- CRT:
-
Cardiac resynchronization therapy
- HF:
-
Heart failure
- HFrEF:
-
Heart failure with reduced ejection fraction
- ICD:
-
Implantable cardiac defibrillator
- INTERMACS:
-
Interagency Registry for Mechanically Assisted Circulatory Support
- LV:
-
Left ventricle
- LVAD:
-
Left ventricular assist device
- MCS:
-
Mechanical circulatory support
- NICMP:
-
Non-ischemic cardiomyopathy
- NT-proBNP:
-
Amino-terminal pro B-type natriuretic peptide
- OHT:
-
Orthotopic heart transplant
- RV:
-
Right ventricle
- UNOS:
-
United Network for Organ Sharing
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Lyon AR, Dent S, Stanway S, et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: a position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur J Heart Fail. 2020;22:1945–60.
• Herrmann J. Adverse cardiac effects of cancer therapies: cardiotoxicity and arrhythmia. Nat Rev Cardiol. 2020;17:474–502.
Bristow MR, Billingham ME, Mason JW. Adriamycin cardiotoxicity. Am J Cardiol. 1984;53:263–4.
Nilsson G, Holmberg L, Garmo H, et al. Distribution of coronary artery stenosis after radiation for breast cancer. J Clin Oncol. 2012;30:380–6.
Jaworski C, Mariani JA, Wheeler G, Kaye DM. Cardiac complications of thoracic irradiation. J Am Coll Cardiol. 2013;61:2319–28.
Groarke JD, Nguyen PL, Nohria A, Ferrari R, Cheng S, Moslehi J. Cardiovascular complications of radiation therapy for thoracic malignancies: the role for non-invasive imaging for detection of cardiovascular disease. Eur Heart J. 2014;35:612–23.
•• Zamorano JL, Lancellotti P, Rodriguez Munoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016;37:2768–801.
de Boer RA, Hulot JS, Tocchetti CG, et al. Common mechanistic pathways in cancer and heart failure. A scientific roadmap on behalf of the Translational Research Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail 2020.
Meijers WC, Maglione M, Bakker SJL, et al. Heart failure stimulates tumor growth by circulating factors. Circulation. 2018;138:678–91.
Lenneman AJ, Wang L, Wigger M, et al. Heart transplant survival outcomes for adriamycin-dilated cardiomyopathy. Am J Cardiol. 2013;111:609–12.
Oliveira GH, Hardaway BW, Kucheryavaya AY, Stehlik J, Edwards LB, Taylor DO. Characteristics and survival of patients with chemotherapy-induced cardiomyopathy undergoing heart transplantation. J Heart Lung Transplant. 2012;31:805–10.
Al-Kindi SG, Oliveira GH. Heart transplantation outcomes in radiation-induced restrictive cardiomyopathy. J Card Fail. 2016;22:475–8.
Oliveira GH, Qattan MY, Al-Kindi S, Park SJ. Advanced heart failure therapies for patients with chemotherapy-induced cardiomyopathy. Circ Heart Fail. 2014;7:1050–8.
• Cardinale D, Colombo A, Lamantia G, et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J Am Coll Cardiol. 2010;55:213–20.
McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371:993–1004.
Martin-Garcia A, Lopez-Fernandez T, Mitroi C, et al. Effectiveness of sacubitril-valsartan in cancer patients with heart failure. ESC Heart Fail. 2020;7:763–7.
Mukku RB, Fonarow GC, Watson KE, et al. Heart failure therapies for end-stage chemotherapy-induced cardiomyopathy. J Card Fail. 2016;22:439–48.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Rev Esp Cardiol (Engl Ed). 2016;69:1167.
Zamorano JL, Lancellotti P, Rodriguez Munoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur J Heart Fail. 2017;19:9–42.
Negishi K, Negishi T, Haluska BA, Hare JL, Plana JC, Marwick TH. Use of speckle strain to assess left ventricular responses to cardiotoxic chemotherapy and cardioprotection. Eur Heart J Cardiovasc Imaging. 2014;15:324–31.
Finet JE. Management of heart failure in cancer patients and cancer survivors. Heart Fail Clin. 2017;13:253–88.
Yancy CW, Jessup M, Bozkurt B, et al. 2016 ACC/AHA/HFSA focused update on new pharmacological therapy for heart failure: an update of the 2013 ACCF/AHA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2016;68:1476–88.
Rickard J, Kumbhani DJ, Baranowski B, Martin DO, Tang WH, Wilkoff BL. Usefulness of cardiac resynchronization therapy in patients with adriamycin-induced cardiomyopathy. Am J Cardiol. 2010;105:522–6.
Singh JP, Solomon SD, Fradley MG, et al. Association of cardiac resynchronization therapy with change in left ventricular ejection fraction in patients with chemotherapy-induced cardiomyopathy. JAMA. 2019;322:1799–805.
Ajijola OA, Nandigam KV, Chabner BA, et al. Usefulness of cardiac resynchronization therapy in the management of doxorubicin-induced cardiomyopathy. Am J Cardiol. 2008;101:1371–2.
Christensen AM, Bjerre J, Schou M, et al. Clinical outcome in patients with implantable cardioverter-defibrillator and cancer: a nationwide study. Europace. 2019;21:465–74.
Bianco CM, Al-Kindi SG, Oliveira GH. Advanced heart failure therapies for cancer therapeutics-related cardiac dysfunction. Heart Fail Clin. 2017;13:327–36.
Musci M, Loebe M, Grauhan O, et al. Heart transplantation for doxorubicin-induced congestive heart failure in children and adolescents. Transplant Proc. 1997;29:578–9.
Oliveira GH, Dupont M, Naftel D, et al. Increased need for right ventricular support in patients with chemotherapy-induced cardiomyopathy undergoing mechanical circulatory support: outcomes from the INTERMACS Registry (Interagency Registry for Mechanically Assisted Circulatory Support). J Am Coll Cardiol. 2014;63:240–8.
Tanindi A, Demirci U, Tacoy G, et al. Assessment of right ventricular functions during cancer chemotherapy. Eur J Echocardiogr. 2011;12:834–40.
Grover S, Leong DP, Chakrabarty A, et al. Left and right ventricular effects of anthracycline and trastuzumab chemotherapy: a prospective study using novel cardiac imaging and biochemical markers. Int J Cardiol. 2013;168:5465–7.
DePasquale EC, Nasir K, Jacoby DL. Outcomes of adults with restrictive cardiomyopathy after heart transplantation. J Heart Lung Transplant. 2012;31:1269–75.
Opelz G, Henderson R. Incidence of non-Hodgkin lymphoma in kidney and heart transplant recipients. Lancet. 1993;342:1514–6.
•• Mancini D, Lietz K. Selection of cardiac transplantation candidates in 2010. Circulation. 2010;122:173–83.
•• Al-Adra DP, Hammel L, Roberts J, et al. Pretransplant solid organ malignancy and organ transplant candidacy: a consensus expert opinion statement. Am J Transplant. 2021;21:460–74.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med. 2004;351:2817–26.
Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–34.
Zhou Z, Sehn LH, Rademaker AW, et al. An enhanced International Prognostic Index (NCCN-IPI) for patients with diffuse large B-cell lymphoma treated in the rituximab era. Blood. 2014;123:837–42.
Al-Adra DP, Hammel L, Roberts J, et al. Preexisting melanoma and hematological malignancies, prognosis, and timing to solid organ transplantation: a consensus expert opinion statement. Am J Transplant. 2021;21:475–83.
Lateef N, Abdul Basit K, Abbasi N, Kazmi SM, Ansari AB, Shah M. Malignancies after heart transplant. Exp Clin Transplant. 2016;14:12–6.
Rinaldi M, Pellegrini C, D’Armini AM, et al. Neoplastic disease after heart transplantation: single center experience. Eur J Cardiothorac Surg. 2001;19:696–701.
Mancini D, Rakita V. Malignancy post heart transplantation: no free lunch. J Am Coll Cardiol. 2018;71:50–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Petra Nijst and W. H. Wilson Tang declare that they have no conflict of interest. W. H. Wilson Tang is a Section Editor for the journal and was not involved in the review of this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Heart Failure
Rights and permissions
About this article
Cite this article
Nijst, P., Tang, W.H.W. Managing Cancer Patients and Survivors With Advanced Heart Failure. Curr Treat Options Cardio Med 23, 73 (2021). https://doi.org/10.1007/s11936-021-00953-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s11936-021-00953-y