Abstract
Purpose of Review
This paper aims to discuss the various work-related musculoskeletal disorders (WRMDs) among urologists and provide an overview of the latest recommendations to improve awareness of ergonomic principles that can be applied in the operating room, with special consideration of challenges faced during pregnancy.
Recent Findings
Urologists suffer from a large burden of WRMDs. The main drivers of pain associated with the various surgical approaches include repetitive movements, static and awkward body positions, and the use of burdensome equipment. Pregnant surgeons are at an even greater risk of WRMDs and face high rates of pregnancy complications.
Summary
Laparoscopy, endoscopy, robot-assisted surgeries, and open surgeries present unique ergonomic challenges for the practicing urologist. Proper posture and equipment use, optimal operating room setup, intraoperative stretching breaks, and an emphasis on teaching ergonomic principles can reduce the risk of WRMDs. Surgeons are also at increased risk of WRMDs during pregnancy but may continue to operate while taking measures to limit physical exertion and fatigue. Improving awareness of and incorporating ergonomic principles early in a urologist’s career may reduce the risk of injury and improve operative performance and longevity.


Similar content being viewed by others
Data Availability
Upon request, the authors of this manuscript are prepared to send relevant documentation in order to verify the validity of the data presented.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hannah KJ, Ball MJ, Edwards MJ. Ergonomics. Introduction to nursing informatics. Health Informatics. New York: Springer; 2006.
Karwowski W, Rizzo F, Rodrick D. Ergonomics. In: Bidgoli H, editor. Encyclopedia of information systems. Boston: Elsevier; 2003. p. 185–201.
Work-related musculoskeletal disorders and ergonomics. 2020. https://www.cdc.gov/workplacehealthpromotion/health-strategies/musculoskeletal-disorders/index.html. Accessed 8 Sept 2022.
Stucky CH, Cromwell KD, Voss RK, Chiang YJ, Woodman K, Lee JE, et al. Surgeon symptoms, strain, and selections: systematic review and meta-analysis of surgical ergonomics. Ann Med Surg (Lond). 2018;27:1–8. https://doi.org/10.1016/j.amsu.2017.12.013.
Epstein S, Sparer EH, Tran BN, Ruan QZ, Dennerlein JT, Singhal D, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153(2): e174947. https://doi.org/10.1001/jamasurg.2017.4947.
• Loeb S, Kerr RR. Practicing urology take a physical toll. Urology Times. 2019;47(8). Surveyed practicing urologists who read their publication and reported on the prevalence of work-related musculoskeletal disorders and the ways they have interfered with urologists' careers.
• Lloyd GL, Chung ASJ, Steinberg S, Sawyer M, Williams DH, Overbey D. Is your career hurting you? The ergonomic consequences of surgery in 701 urologists worldwide. J Endourol. 2019;33(12):1037–42. https://doi.org/10.1089/end.2019.0150. Surveyed a multinational cohort of more than 700 urologists to assess the prevalence of work-related pain and identify factors that increase or decrease the risk of pain.
Wolf JS Jr, Marcovich R, Gill IS, Sung GT, Kavoussi LR, Clayman RV, et al. Survey of neuromuscular injuries to the patient and surgeon during urologic laparoscopic surgery. Urology. 2000;55(6):831–6. https://doi.org/10.1016/s0090-4295(00)00488-x.
Dornbier R, Gonzalez CM. Workforce issues in urology. Urol Clin North Am. 2021;48(2):161–71. https://doi.org/10.1016/j.ucl.2021.01.001.
Plerhoples TA, Hernandez-Boussard T, Wren SM. The aching surgeon: a survey of physical discomfort and symptoms following open, laparoscopic, and robotic surgery. J Robot Surg. 2012;6(1):65–72. https://doi.org/10.1007/s11701-011-0330-3.
Tjiam IM, Goossens RH, Schout BM, Koldewijn EL, Hendrikx AJ, Muijtjens AM, et al. Ergonomics in endourology and laparoscopy: an overview of musculoskeletal problems in urology. J Endourol. 2014;28(5):605–11. https://doi.org/10.1089/end.2013.0654.
Hemal AK, Srinivas M, Charles AR. Ergonomic problems associated with laparoscopy. J Endourol. 2001;15(5):499–503. https://doi.org/10.1089/089277901750299294.
Gofrit ON, Mikahail AA, Zorn KC, Zagaja GP, Steinberg GD, Shalhav AL. Surgeons’ perceptions and injuries during and after urologic laparoscopic surgery. Urology. 2008;71(3):404–7. https://doi.org/10.1016/j.urology.2007.07.077.
Bagrodia A, Raman JD. Ergonomics considerations of radical prostatectomy: physician perspective of open, laparoscopic, and robot-assisted techniques. J Endourol. 2009;23(4):627–33. https://doi.org/10.1089/end.2008.0556.
Hubert N, Gilles M, Desbrosses K, Meyer JP, Felblinger J, Hubert J. Ergonomic assessment of the surgeon’s physical workload during standard and robotic assisted laparoscopic procedures. Int J Med Robot. 2013;9(2):142–7. https://doi.org/10.1002/rcs.1489.
Lawson EH, Curet MJ, Sanchez BR, Schuster R, Berguer R. Postural ergonomics during robotic and laparoscopic gastric bypass surgery: a pilot project. J Robot Surg. 2007;1(1):61–7. https://doi.org/10.1007/s11701-007-0016-z.
Guillotreau J, Gamé X, Mouzin M, Doumerc N, Mallet R, Sallusto F, et al. Radical cystectomy for bladder cancer: morbidity of laparoscopic versus open surgery. J Urol. 2009;181(2):554–9; discussion 9. https://doi.org/10.1016/j.juro.2008.10.011.
Al-Rashedy M, Dadibhai M, Shareif A, Khandelwal MI, Ballester P, Abid G, et al. Laparoscopic gastric bypass for gastric outlet obstruction is associated with smoother, faster recovery and shorter hospital stay compared with open surgery. J Hepatobiliary Pancreat Surg. 2005;12(6):474–8. https://doi.org/10.1007/s00534-005-1013-0.
Björnsson B, Larsson AL, Hjalmarsson C, Gasslander T, Sandström P. Comparison of the duration of hospital stay after laparoscopic or open distal pancreatectomy: randomized controlled trial. Br J Surg. 2020;107(10):1281–8. https://doi.org/10.1002/bjs.11554.
Etoh T, Honda M, Kumamaru H, Miyata H, Yoshida K, Kodera Y, et al. Morbidity and mortality from a propensity score-matched, prospective cohort study of laparoscopic versus open total gastrectomy for gastric cancer: data from a nationwide web-based database. Surg Endosc. 2018;32(6):2766–73. https://doi.org/10.1007/s00464-017-5976-0.
•• Gabrielson AT, Clifton MM, Pavlovich CP, Biles MJ, Huang M, Agnew J, et al. Surgical ergonomics for urologists: a practical guide. Nat Rev Urol. 2021;18(3):160–9. https://doi.org/10.1038/s41585-020-00414-4. Provided a comprehensive review of ergonomic recommendations for the practicing urologist and identified areas for future improvement.
Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung J. A comparison of surgeons’ posture during laparoscopic and open surgical procedures. Surg Endosc. 1997;11(2):139–42. https://doi.org/10.1007/s004649900316.
Nguyen NT, Ho HS, Smith WD, Philipps C, Lewis C, De Vera RM, et al. An ergonomic evaluation of surgeons’ axial skeletal and upper extremity movements during laparoscopic and open surgery. Am J Surg. 2001;182(6):720–4. https://doi.org/10.1016/s0002-9610(01)00801-7.
Frede T, Stock C, Renner C, Budair Z, Abdel-Salam Y, Rassweiler J. Geometry of laparoscopic suturing and knotting techniques. J Endourol. 1999;13(3):191–8. https://doi.org/10.1089/end.1999.13.191.
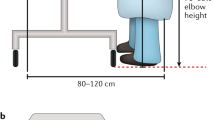
Berguer R, Smith WD, Davis S. An ergonomic study of the optimum operating table height for laparoscopic surgery. Surg Endosc. 2002;16(3):416–21. https://doi.org/10.1007/s00464-001-8190-y.
van Veelen MA, Kazemier G, Koopman J, Goossens RH, Meijer DW. Assessment of the ergonomically optimal operating surface height for laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 2002;12(1):47–52. https://doi.org/10.1089/109264202753486920.
Manasnayakorn S, Cuschieri A, Hanna GB. Ergonomic assessment of optimum operating table height for hand-assisted laparoscopic surgery. Surg Endosc. 2009;23(4):783–9. https://doi.org/10.1007/s00464-008-0068-9.
van Veelen MA, Nederlof EA, Goossens RH, Schot CJ, Jakimowicz JJ. Ergonomic problems encountered by the medical team related to products used for minimally invasive surgery. Surg Endosc. 2003;17(7):1077–81. https://doi.org/10.1007/s00464-002-9105-2.
van Det MJ, Meijerink WJ, Hoff C, Totté ER, Pierie JP. Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc. 2009;23(6):1279–85. https://doi.org/10.1007/s00464-008-0148-x.
Omar AM, Wade NJ, Brown SI, Cuschieri A. Assessing the benefits of “gaze-down” display location in complex tasks. Surg Endosc. 2005;19(1):105–8. https://doi.org/10.1007/s00464-004-8141-5.
Turville KL, Psihogios JP, Ulmer TR, Mirka GA. The effects of video display terminal height on the operator: a comparison of the 15 degree and 40 degree recommendations. Appl Ergon. 1998;29(4):239–46. https://doi.org/10.1016/s0003-6870(97)00048-3.
Medicare physician and other practioners - by geography and service. 2019. https://data.cms.gov/provider-summary-by-type-of-service/medicare-physician-other-practitioners/medicare-physician-other-practitioners-by-geography-and-service/data. Accessed 9 Aug 2022.
Spaner SJ, Warnock GL. A brief history of endoscopy, laparoscopy, and laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 1997;7(6):369–73. https://doi.org/10.1089/lap.1997.7.369.
Luttmann A, Sökeland J, Laurig W. Muscular strain and fatigue among urologists during transurethral resections using direct and monitor endoscopy. Eur Urol. 1998;34(1):6–13; discussion 4. https://doi.org/10.1159/000019670.
Omar M, Sultan MF, El Sherif E, Abdallah MM, Monga M. Ergonomics and musculoskeletal symptoms in surgeons performing endoscopic procedures for benign prostatic hyperplasia. Ther Adv Urol. 2020;12:1756287220904806. https://doi.org/10.1177/1756287220904806.
• Alnadhari I, Ali O, Abdeljaleel O, Sampige VRP, Shamsodini A, Salah M. Ergonomics and surgeon comfort during flexible ureteroscopy. Res Rep Urol. 2021;13:415–24. https://doi.org/10.2147/rru.S317347. Conducted a narrative review of ergonomic issues during flexible ureteroscopy and made recommendations for ergonomic surgical equipment and operating room setup.
• Wright HC, Gheordunescu G, O’Laughlin K, Sun A, Fulla J, Kachroo N, et al. Ergonomics in the OR: an electromyographic evaluation of common muscle groups used during simulated flexible ureteroscopy - a pilot study. Urology. 2022. https://doi.org/10.1016/j.urology.2022.08.028. Compared ureteroscope type and sitting vs. standing position by utilizing surface EMG to measure muscle activation patterns in the upper trunk and extremities during simulated flexible ureteroscopy.
Luttmann A, Jäger M, Sökeland J. Ergonomic assessment of the posture of surgeons performing endoscopic transurethral resections in urology. J Occup Med Toxicol. 2009;4:26. https://doi.org/10.1186/1745-6673-4-26.
van Veelen MA, Jakimowicz JJ, Kazemier G. Improved physical ergonomics of laparoscopic surgery. Minim Invasive Ther Allied Technol. 2004;13(3):161–6. https://doi.org/10.1080/13645700410033193.
Pelz DM. Low back pain, lead aprons, and the angiographer. AJNR Am J Neuroradiol. 2000;21(7):1364.
• Golan R, Shah O. Performance optimization strategies for complex endourologic procedures. Urology. 2020;139:44–9. https://doi.org/10.1016/j.urology.2020.01.033. Reviewed a number of important ergonomic factors during endoscopic surgery, including operating room setup, monitor positioning, and type of ureteroscope.
Fakhoury E, Provencher JA, Subramaniam R, Finlay DJ. Not all lightweight lead aprons and thyroid shields are alike. J Vasc Surg. 2019;70(1):246–50. https://doi.org/10.1016/j.jvs.2018.07.055.
Ludwig WW, Lee G, Ziemba JB, Ko JS, Matlaga BR. Evaluating the ergonomics of flexible ureteroscopy. J Endourol. 2017;31(10):1062–6. https://doi.org/10.1089/end.2017.0378.
Talso M, Proietti S, Emiliani E, Gallioli A, Dragos L, Orosa A, et al. Comparison of flexible ureterorenoscope quality of vision: an in vitro study. J Endourol. 2018;32(6):523–8. https://doi.org/10.1089/end.2017.0838.
Healy KA, Pak RW, Cleary RC, Colon-Herdman A, Bagley DH. Hand problems among endourologists. J Endourol. 2011;25(12):1915–20. https://doi.org/10.1089/end.2011.0128.
Okada S, Hamamoto S, Inoue T, Minagawa S, Morikawa H, Matsuda T, et al. One- versus two-surgeon active stone retrieval procedures for flexible ureteroscopy: an off-site simulator comparative study. Int J Urol. 2021;28(6):665–71. https://doi.org/10.1111/iju.14534.
Anan G, Hattori K, Hatakeyama S, Ohyama C, Sato M. Efficacy of one-surgeon basketing technique for stone extraction during flexible ureteroscopy for urolithiasis. Arab J Urol. 2021;19(4):447–53. https://doi.org/10.1080/2090598x.2021.1889943.
Lee MR, Lee GI. Does a robotic surgery approach offer optimal ergonomics to gynecologic surgeons?: a comprehensive ergonomics survey study in gynecologic robotic surgery. J Gynecol Oncol. 2017;28(5): e70. https://doi.org/10.3802/jgo.2017.28.e70.
Avila D, Link RE. Robotic and laparoscopic radical prostatectomy. In: Su L, editor. Early Diagnosis and Treatment of Cancer Series: Prostate Cancer. W.B. Saunders; 2010. p. 121–35.
Abiri A, Tao A, LaRocca M, Guan X, Askari SJ, Bisley JW, et al. Visual-perceptual mismatch in robotic surgery. Surg Endosc. 2017;31(8):3271–8. https://doi.org/10.1007/s00464-016-5358-z.
Esposito MP, Ilbeigi P, Ahmed M, Lanteri V. Use of fourth arm in da Vinci robot-assisted extraperitoneal laparoscopic prostatectomy: novel technique. Urology. 2005;66(3):649–52. https://doi.org/10.1016/j.urology.2005.03.061.
Pierorazio PM, Patel HD, Feng T, Yohannan J, Hyams ES, Allaf ME. Robotic-assisted versus traditional laparoscopic partial nephrectomy: comparison of outcomes and evaluation of learning curve. Urology. 2011;78(4):813–9. https://doi.org/10.1016/j.urology.2011.04.065.
BIFMA-G1. Ergonomics guideline for furniture used in office work spaces designed for computer use. Business & Institutional Furniture Manufacturers Association. 2013.
Lux MM, Marshall M, Erturk E, Joseph JV. Ergonomic evaluation and guidelines for use of the daVinci Robot system. J Endourol. 2010;24(3):371–5. https://doi.org/10.1089/end.2009.0197.
Body measurements. 2021. https://www.cdc.gov/nchs/fastats/body-measurements.htm. Accessed 12 Sept 2022.
Catanzarite T, Tan-Kim J, Menefee SA. Ergonomics in gynecologic surgery. Curr Opin Obstet Gynecol. 2018;30(6):432–40. https://doi.org/10.1097/gco.0000000000000502.
Guidelines for retail grocery stores. US Department of Labor Occupational Safety and Health Administration; 2004.
Haramis G, Rosales JC, Palacios JM, Okhunov Z, Mues AC, Lee D, et al. Prospective randomized evaluation of FOOT gel pads for operating room staff COMFORT during laparoscopic renal surgery. Urology. 2010;76(6):1405–8. https://doi.org/10.1016/j.urology.2010.01.018.
Graversen JA, Korets R, Mues AC, Katsumi HK, Badani KK, Landman J, et al. Prospective randomized evaluation of gel mat foot pads in the endoscopic suite. J Endourol. 2011;25(11):1793–6. https://doi.org/10.1089/end.2011.0155.
Nimbarte AD, Sivak-Callcott JA, Zreiqat M, Chapman M. Neck postures and cervical spine loading among microsurgeons operating with loupes and headlamp. IIE Transactions on Occupational Ergonomics and Human Factors. 2013;1(4):215–23. https://doi.org/10.1080/21577323.2013.840342.
• Meltzer AJ, Hallbeck MS, Morrow MM, Lowndes BR, Davila VJ, Stone WM, et al. Measuring ergonomic risk in operating surgeons by using wearable technology. JAMA Surg. 2020;155(5):444–6. https://doi.org/10.1001/jamasurg.2019.6384. Utilized wearable sensors to evaluate ergonomic risks of surgeon postures while they operated using loupes and headlamps.
Lakhiani C, Fisher SM, Janhofer DE, Song DH. Ergonomics in microsurgery. J Surg Oncol. 2018;118(5):840–4. https://doi.org/10.1002/jso.25197.
LumaDent ErgoPrism. https://www.lumadent.com/loupes/ep.html?gclid=CjwKCAjwsfuYBhAZEiwA5a6CDPL4qPjSxiGo-yDL5Osqze0hdlLG2ZiVsKcE3dlsjYvRuXvCRZ0UjhoCxl4QAvD_BwE. Accessed 12 Sept 2022.
• Hemmati P, Nguyen TC, Dearani JA. Ergonomics for surgeons by surgeons-posture, loupes, and exercise. JAMA Surg. 2022. https://doi.org/10.1001/jamasurg.2022.0676. Reviewed the pros and cons of various loupe designs.
Dairywala MI, Gupta S, Salna M, Nguyen TC. Surgeon strength: ergonomics and strength training in cardiothoracic surgery. Semin Thorac Cardiovasc Surg. 2021. https://doi.org/10.1053/j.semtcvs.2021.09.015.
Park AE, Zahiri HR, Hallbeck MS, Augenstein V, Sutton E, Yu D, et al. Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus: a multicenter cohort study. Ann Surg. 2017;265(2):340–6. https://doi.org/10.1097/sla.0000000000001665.
Rosenblatt PL, McKinney J, Adams SR. Ergonomics in the operating room: protecting the surgeon. J Minim Invasive Gynecol. 2013;20(6):744. https://doi.org/10.1016/j.jmig.2013.07.006.
•• Koshy K, Syed H, Luckiewicz A, Alsoof D, Koshy G, Harry L. Interventions to improve ergonomics in the operating theatre: a systematic review of ergonomics training and intra-operative microbreaks. Ann Med Surg (Lond). 2020;55:135–42. https://doi.org/10.1016/j.amsu.2020.02.008. Conducted a systematic review of recently proposed protocols for intraoperative microbreaks and reported on their effectiveness.
Liang B, Qi L, Yang J, Cao Z, Zu X, Liu L, et al. Ergonomic status of laparoscopic urologic surgery: survey results from 241 urologic surgeons in China. PLoS ONE. 2013;8(7): e70423. https://doi.org/10.1371/journal.pone.0070423.
Khan R, Scaffidi MA, Satchwell J, Gimpaya N, Lee W, Genis S, et al. Impact of a simulation-based ergonomics training curriculum on work-related musculoskeletal injury risk in colonoscopy. Gastrointest Endosc. 2020;92(5):1070-80.e3. https://doi.org/10.1016/j.gie.2020.03.3754.
Aaron KA, Vaughan J, Gupta R, Ali NE, Beth AH, Moore JM, et al. The risk of ergonomic injury across surgical specialties. PLoS ONE. 2021;16(2): e0244868. https://doi.org/10.1371/journal.pone.0244868.
Smith C, Galante JM, Pierce JL, Scherer LA. The surgical residency baby boom: changing patterns of childbearing during residency over a 30-year span. J Grad Med Educ. 2013;5(4):625–9. https://doi.org/10.4300/jgme-d-12-00334.1.
• Rangel EL, Castillo-Angeles M, Easter SR, Atkinson RB, Gosain A, Hu YY, et al. Incidence of infertility and pregnancy complications in US female surgeons. JAMA Surg. 2021;156(10):905–15. https://doi.org/10.1001/jamasurg.2021.3301. Surveyed nearly 700 US female surgeons and reported on rates of childbearing, as well as rates of pregancy complications and risk factors associated with pregancy complications.
Lerner LB, Stolzmann KL, Gulla VD. Birth trends and pregnancy complications among women urologists. J Am Coll Surg. 2009;208(2):293–7.
•• Francis F, Johnsunderraj SE, Divya KY, Raghavan D, Al-Furgani A, Bera LP, et al. Ergonomic stressors among pregnant healthcare workers: impact on pregnancy outcomes and recommended safety practices. Sultan Qaboos Univ Med J. 2021;21(2):e172–e181. https://doi.org/10.18295/squmj.2021.21.02.004. Conducted a narrative review of the ergonomic stressors that affect pregnant healthcare workers and provided a number of recommendations to protect maternal and fetal health.
Cohen-Rosenblum AR, Varady NH, Leonovicz O, Chen AF. Repetitive musculoskeletal injuries: a survey of female adult reconstruction surgeons. J Arthroplasty. 2022;37(8):1474-7.e6. https://doi.org/10.1016/j.arth.2022.01.001.
•• Harnsberger CR, Davids JS. The pregnant surgeon. Clin Colon Rectal Surg. 2019;32(6):450–6 https://doi.org/10.1055/s-0039-1693012. Conducted a narrative review of the occupational hazards to the pregnant surgeon, organized by trimester, and provided guidance on reducing caseload.
Pennick V, Liddle SD. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev. 2013(8):Cd001139. https://doi.org/10.1002/14651858.CD001139.pub3.
MacDonald LA, Waters TR, Napolitano PG, Goddard DE, Ryan MA, Nielsen P, et al. Clinical guidelines for occupational lifting in pregnancy: evidence summary and provisional recommendations. Am J Obstet Gynecol. 2013;209(2):80–8. https://doi.org/10.1016/j.ajog.2013.02.047.
•• Kakaraparthi VN, Vishwanathan K, Gadhavi B, Reddy RS, Tedla JS, Samuel PS, et al. Application of the rapid upper limb assessment tool to assess the level of ergonomic risk among health care professionals: a systematic review. Work. 2022;71(3):551–64. https://doi.org/10.3233/wor210239. Conducted a systematic review of the use of the Rapid Upper Limb Assessment (RULA) to evaluate ergonomic risk in healthcare workers.
Dwyer A, Huckleby J, Kabbani M, Delano A, De Sutter M, Crawford D. Ergonomic assessment of robotic general surgeons: a pilot study. J Robot Surg. 2020;14(3):387–92. https://doi.org/10.1007/s11701-019-00996-1.
Meems M, Truijens S, Spek V, Visser LH, Pop VJ. Prevalence, course and determinants of carpal tunnel syndrome symptoms during pregnancy: a prospective study. BJOG. 2015;122(8):1112–8. https://doi.org/10.1111/1471-0528.13360.
Salazar L. Addressing the medical device safety crisis. 2021. https://www.theregreview.org/2021/10/27/salazar-addressing-medical-device-safety-crisis/. Accessed 11 Sept 2022.
•• Chrouser K, Foley F, Goldenberg M, Hyder J, Kim FJ, Maranchie J, et al. Optimizing outcomes in urologic surgery: intraoperative considerations. Am Urol Assoc. 2018. Official publication of the American Urological Association that recognized the importance of operating room ergonomics in optimizing patient outcomes.
Hung AJ, Chen J, Gill IS. Automated performance metrics and machine learning algorithms to measure surgeon performance and anticipate clinical outcomes in robotic surgery. JAMA Surg. 2018;153(8):770–1. https://doi.org/10.1001/jamasurg.2018.1512.
Kono E, Taniguchi K, Lee SW, Ohdaira T, Uchiyama K. Laparoscopic instrument for female surgeons: an innovative model for endoscopic purse-string suture. Minim Invasive Ther Allied Technol. 2022;31(4):642–5. https://doi.org/10.1080/13645706.2020.1851724.
Brearley S, Watson H. Towards an efficient retractor handle: an ergonomic study. Ann R Coll Surg Engl. 1983;65(6):382–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Education
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gillespie, A.M., Wang, C. & Movassaghi, M. Ergonomic Considerations in Urologic Surgery. Curr Urol Rep 24, 143–155 (2023). https://doi.org/10.1007/s11934-022-01142-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-022-01142-5