Abstract
Purpose of Review
Sepsis is a leading cause of death worldwide. Groundbreaking international collaborative efforts have culminated in the widely accepted surviving sepsis guidelines, with iterative improvements in management strategies and definitions providing important advances in care for patients. Key to the diagnosis of sepsis is identification of infection, and whilst the diagnostic criteria for sepsis is now clear, the diagnosis of infection remains a challenge and there is often discordance between clinician assessments for infection.
Recent Findings
We review the utility of common biochemical, microbiological and radiological tools employed by clinicians to diagnose infection and explore the difficulty of making a diagnosis of infection in severe inflammatory states through illustrative case reports. Finally, we discuss some of the novel and emerging approaches in diagnosis of infection and sepsis.
Summary
While prompt diagnosis and treatment of sepsis is essential to improve outcomes in sepsis, there remains no single tool to reliably identify or exclude infection. This contributes to unnecessary antimicrobial use that is harmful to individuals and populations. There is therefore a pressing need for novel solutions. Machine learning approaches using multiple diagnostic and clinical inputs may offer a potential solution but as yet these approaches remain experimental.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The third consensus definition of sepsis is ‘life-threatening organ dysfunction caused by a dysregulated host response to infection’ and septic shock a subset of patients with a vasopressor requirement and lactate > 2 mmol/L [1]. At its most severe, sepsis continues to have a high mortality. Agreed criteria to define sepsis are intended to identify patients early, allowing the prompt initiation of treatment, including sepsis care bundles, which may improve outcomes [2]. It also provides a common language for international research and outcome reporting [1]. The need for a third consensus definition points to the challenges underlying the diagnosis of sepsis and the evolution of our understanding of the pathophysiology of this disease and its mimics.
The first consensus definition, made in the 1990’s, utilised one haematological and three clinical variables (temperature, heart rate, respiratory rate and white blood cell count) to identify sepsis in those with infection [3]. These variables, which defined the systemic inflammatory response syndrome (SIRS), provided a useful starting point for standardising the diagnosis of sepsis but had some limitations. Foremost among these is that SIRS is found frequently in patients admitted to intensive care units (ICU) regardless of the reason for admission [4,5,6,7], yet still fails to identify some patients with severe infection causing significant organ dysfunction [8]. The most recent criteria characterise patients with sepsis as those with a change in SOFA (sequential organ failure assessment) score of 2 points or more within a 24-h time period in the presence of suspected infection. The argument in favour of this change is cited as improved predictive validity over SIRS for ICU mortality or prolonged ICU stay. Further advocated is the identification of those patients with infection who are at risk of deterioration using clinical criteria (qSOFA) — two or more of altered mental state, tachypnoea (defined as a respiratory rate > 22 breaths per minute) or hypotension (defined as systolic blood pressure < 100 mmHg) [1]. These criteria make the definition of sepsis clear and its diagnosis in the patient with an infection straightforward, since SOFA scores are readily calculable from routine examination and laboratory tests.
What is not easy is the diagnosis of infection. Indeed, the SEPSIS-3 task force specifically state that examining the definitions of infection was not ‘within the task force brief’. Datasets used to model the performance of the qSOFA and the new definition of sepsis contained patients with ‘suspected infection’. There is no commentary on how the suspicion of infection arises or what objective thresholds exist to make a diagnosis of infection, suspected or otherwise. Similarly, the surviving sepsis guidelines seem to take the diagnosis of infection or suspected infection as read. ‘Diagnosis’ comes in third in the order of consideration after resuscitation and screening for sepsis. Commentary on diagnostic and prognostic biomarkers of infection first appear some 18 pages into these guidelines [2].
In this article, we aim to briefly summarise the utility of tools used to aid clinicians in the diagnosis of infection, and therefore in the diagnosis of sepsis.
Screening for Sepsis
The 2016 iteration of the surviving sepsis campaign guidelines recommends hospitals implement a sepsis screening system for acutely ill, high-risk patients [2]. The utility of sepsis screening tools, and their applicability, continues to be a subject of debate. Identifying the impact of a screening tool alone is challenging, as sepsis care bundles are often implemented alongside screening tools, perhaps explaining why this remains a ‘best practice statement’ in the Surviving Sepsis Campaign Guidelines. For example, in Levy et al.’s study on the impact of the surviving sepsis campaign in 2010, participants were enrolled only if they already had suspected infection and met SIRS criteria for sepsis [9], meaning the impact of the screening tool itself could not be reviewed. Other data cited by the Surviving Sepsis Campaign arise from quality improvement projects. Jones et al. reported a 12% absolute reduction in sepsis associated mortality after the introduction of a 17-point sepsis screening tool [10], but there was promotion of specific interventions following screening in this study too. Damiani et al. undertook a systematic review of such improvement programmes and found consistent reporting of improvement in sepsis outcomes [11].
The SEPSIS-3 task force noted that a patient found to meet qSOFA criteria should ‘prompt consideration of possible infection in patients not previously recognised as infected’ [12]. One potential drawback of qSOFA as a potential screening tool is that it was identified and tested using a dataset of patients already suspected of having infection [13]. The UK national screening committee notes that the purpose of screening is to offer a test to a population who ‘do not necessarily perceive that they are at risk of, or are already affected by, a disease or its complications’ [14]. Since qSOFA was initially validated in a group of patients in hospital with suspected infection and continues to be tested largely in this population, it arguably falls short on this definition. Indeed, members of the task force have subsequently stated that qSOFA is not a screening tool but should be used to identify those at risk of worse outcome from infection. Given the tools used by clinicians to diagnose infection, it may be preferential to use the formal definition of sepsis to predict poor outcome, since many of these tools will also calculate a formal SOFA score. Perhaps the exception is access to a readily available PaO2 for patients outside critical care, although conversion models exist to substitute oxygen saturations (SpO2) [15].
Can Clinicians Agree on Whether an Infection Is Present?
Table 1 provides brief details of presenting symptoms of three imagined case scenarios. They are intended to describe a typical presentation of acute pancreatitis (case 1) and sepsis secondary to a complicated urinary tract infection (case 2). The details provided meet the qSOFA screening criteria that suggest we consider sepsis if we suspect infection. We intend to provoke suspicion of infection in both cases, noting that it appears more likely in case 2. Scenario 3 would satisfy the definition of sepsis; however, it is a case of systemic juvenile arthritis with evolving haemophagocytosis with no infectious trigger. We recognise that there will not be universal suspicion of infection and sepsis amongst physicians reading such case examples. In a survey of intensivists in 104 US hospitals, Stevens et al. found significant discordance in diagnosing pneumonia, with some physicians identifying pneumonia in 100% and others 0% of case vignettes presented to them [16]. Lopansri et al. found only moderate inter-observer agreement on the diagnosis of sepsis or SIRS in a multi-centre cohort of patients with culture positive infection, disagreement was most pronounced in cases of respiratory infections [17], and Rhee et al. found similar disagreement in their survey of US clinicians [18]. Similar results have been found in paediatric studies. Peltola et al. found physician’s sensitivity of 38% for diagnosing influenza in a prospective study of 2288 children with respiratory infections [19] and in a prospective cohort study of nearly 16,000 children with fever presenting to a hospital in Australia, Craig et al. found a low sensitivity of physicians’ diagnosis of bacterial infection (10–50%) [20].
The reader may, or may not, consider infection possible in case 1, but suspicion of infection in cases of acute pancreatitis is high amongst clinicians and antibiotics are often prescribed [21]. The use of routine antibiotics in severe acute pancreatitis is not recommended as there is no evidence of efficacy, either in terms of mortality or reduction in the incidence of infected necrosis [22]. However, as there is some evidence of efficacy in necrotising pancreatitis, international guidelines recommend the use of antibiotics where infection is suspected [23]. In what is a somewhat recurring theme in this subject area, no recommendations are given as to when or how to suspect infection. Given the most common cause of death in acute pancreatitis is infection [24], clinicians are left somewhat in a quandary with regards to antibiotics in this condition. The Surviving Sepsis Campaign guidelines recommend the initiation of antibiotics within one hour of a diagnosis being made or suspected. It seems likely that this time limit will expire prior to any complex cross-sectional imaging can be organised and reported, meaning antibiotics are likely to be given before a diagnosis of necrotising pancreatitis can be confirmed or ruled out.
Diagnostic Value of Common Laboratory Biomarkers
Blood culture is the gold standard for diagnosis of blood stream infection but is limited by poor sensitivity and the required processing time. Challenges in clinical diagnosis and requirement for prompt diagnosis and treatment have led to reliance on biomarkers such as white blood cell count, C-reactive protein (CRP), and procalcitonin (PCT). Indeed, the first consensus sepsis definition incorporated an increased (> 12 × 109 /L) or decreased (< 4 × 109 /L) white blood cell count into the SIRS criteria [3]. However, the utility of serum biomarkers to predict or exclude blood stream infection is debated, with many of the commonly used tests lacking sensitivity and specificity. In a recent retrospective cohort study, Marik and Stephenson reported white blood cell count to have a very poor predictive value for bacteraemia in patients presenting with suspected sepsis with an area under the receiver operating characteristic (AUROC) as low as 0.52 [25]. Siegel et al. found that 52% of patients presenting to the Emergency Department with proven blood culture positive bacteraemia had a normal white blood cell count as defined by the SIRS criteria [26]. In a meta-analysis of the value of diagnostic tests in febrile children, Van den Bruel et al. found white cell count to be of little diagnostic benefit in ruling out serious infection, with a negative likelihood ratio as low as 0.61 [27]. In a retrospective analysis of 1169 appendicectomies in a district general hospital, Panagiotopoulou et al. found neither raised CRP or white cell count as useful diagnostic markers for acute appendicitis. Whilst they found a raised white cell count to be relatively sensitive (84%), it was not specific (58%) and did not have a favourable negative predictive value (68%). The results were similar for CRP [28]. Warschkow et al. found similar results in their review of the routine blood tests of patients who had undergone open resection of colorectal cancer [29]. They found day 5 raised white cell count to have a sensitivity of 70% and specificity of 58% for inflammatory complications.
The neutrophil to lymphocyte count ratio has been consistently reported to be a more accurate marker of physiological stress than absolute white blood cell or neutrophil counts [30, 31]. A rise of neutrophil count and fall in lymphocyte count is commonly encountered in systemic illness and is hypothesised to be due to the endogenous actions of cortisol and catecholamines. Furthermore, sepsis causes lymphocyte migration to inflammatory tissues and increased lymphocyte apoptosis resulting in a greater rise in neutrophil to lymphocyte count ratio when compared with other causes of physiological stress. A normal neutrophil to lymphocyte ratio is reported to be 2.15 and a level of 10 considered to be a threshold for the diagnosis of bacteraemia [32, 33]. In a prospective study of 1572 patients presenting to the Emergency Department, Ljungstrӧm et al. found neutrophil to lymphocyte count ratio to be superior to PCT and CRP for the diagnosis of bacterial sepsis (AUROC 0.68 vs 0.64 vs 0.57, p < 0.05) and the diagnosis of bacterial infection, although the difference in AUROC did not reach statistical significant in the latter [34]. Neutrophil to lymphocyte count ratio is seen to be elevated in any form of severe physiological stress and is not specific for the diagnosis of bacteraemia. This is recently evidenced by its application for predicting disease severity in patients with coronavirus disease 2019 (COVID-19) [35]. In addition, neutrophil to lymphocyte count ratio is significantly less accurate in the diagnosis of sepsis in the critical care population in whom there is invariably an elevated neutrophil to lymphocyte count ratio even in non-infected patients. Westerdijk et al. reported neutrophil to lymphocyte count ratio to have an AUROC of 0.66 for predicting sepsis in critical care versus remarkably high AUROCs of 0.89 and 0.88 for CRP and PCT, respectively [36].
C-reactive protein (CRP) is an acute phase protein synthesised in the liver following inflammatory stimuli, with concentrations rising within 12–24 h [37, 38]. Although a commonly used marker in critical illness, CRP lacks specificity for bacterial infection and is seen to rise in most other causes of inflammation. Serum CRP level may take up to 72 h to peak, contributing to diagnostic and surveillance challenges [39]. In a meta-analysis assessing the diagnostic accuracy of CRP in sepsis, Tan et al. found CRP to have a AUROC of 0.75 with a pooled sensitivity of 0.80 but a specificity of only 0.61 [40]. The level of CRP was reported to have little correlation with the severity of illness in sepsis. Conversely, CRP is the most utilised biomarker for predicting disease severity in pancreatitis due to its low cost and widespread availability [41]. A CRP level of > 150 mg/L is regarded as a threshold marker of pancreatitis severity with Khanna et al. reporting this cutoff level to have a 100% sensitivity and 81.4% specificity for necrotising pancreatitis [42]. CRP does not, however, consistently distinguish between sterile and infected pancreatic necrosis and is not recommended to be used as a marker to commence antimicrobial therapy. The CRP trend between two different time points is more efficacious with Póvoa et al. reporting a daily CRP variation of > 41 mg/L in critical care patients predicting bacterial infection with a sensitivity and specificity of 0.92 and 0.71, respectively [43]. Erythrocyte sedimentation rate (ESR) is an alternative non-specific test of systemic inflammation that remains in use in some centres, particularly for the surveillance of rheumatological disorders. It demonstrates a slower rise than CRP and has been suggested to be inferior to PCT, CRP and WBC count in the diagnosis and prognosis of sepsis using the SEPSIS-3 criteria [44].
Procalcitonin (PCT) is a precursor to calcitonin. Its production is upregulated in response to sepsis and has been suggested to reliably distinguish between bacterial infection and other inflammatory states [45]. PCT rises 2–3 h following infection and reaches a peak at 24 h. Although a faster rise than CRP, the delay in reaching peak concentration necessitates caution when using PCT as a sole marker of infection at initial presentation. Highest PCT levels are detected in gram-negative bacteraemia with only a minimal elevation in fungal infection [46]. Given the increasing prevalence of fungaemia, PCT is a potentially useful biomarker to predict those who will not benefit from empirical antifungal therapy [46,47,48]. In a systematic review and meta-analysis, Wacker et al. reported PCT to be a good biomarker to differentiate between sepsis and other non-inflammatory syndromes with an AUROC of 0.85 [49]. Pooled results from the several meta-analyses have reported overall sensitivity and specificity ranges of 0.72 to 0.93 and 0.64 to 0.84, respectively, with positive and negative likelihood ratios of 3.0 to 5.9 and 0.11 to 0.44 [50]. These data suggest a moderate discriminatory ability between bacterial infection and non-infectious inflammatory states but a negative test cannot exclude infection. PCT may be useful in predicting infective versus non-infective pancreatic necrosis with Rau et al. reporting a threshold of > 1.8 ng/mL having a similar sensitivity (0.95) and specificity (0.88) to US guided fine needle aspiration (FNA) [51]. Although subsequent research predicts a slightly lower sensitivity, these data have prompted international guidelines to suggest using PCT to aid in deciding whether to commence antimicrobial therapy [52, 53]. PCT may be less effective in distinguishing between bacterial and viral infection with Kamat et al. reporting poor sensitivity (0.55) and only moderate specificity (0.76) in a systematic review and meta-analysis of 12 papers focused on serum PCT levels in patients with community-acquired pneumonia [54]. Similarly, PCT exhibits a lower diagnostic AUROC and sensitivity for predicting bacterial infection in patients with renal impairment (defined by an estimated glomerular filtration rate < 30 mL/min/1.72 m2) [55], immunocompromised patients [56] and in patients with autoimmune conditions [57].
Numerous studies have assessed the safety and efficacy of discontinuing antimicrobial therapy when PCT concentration reaches < 1 ng/mL or falls by 65–90% from peak values. They have demonstrated a reduction in total duration of antimicrobials (around 2 days) without a negative impact on length of stay and mortality rates [58,59,60]. Many of the antimicrobial courses in the PCT-guided groups remained > 7 days emphasising that more evidence is required to correlate this data with emerging evidence that shorter antibiotic courses may be appropriate for certain disease states [61].
The initial investigations in our theoretical cases emphasise the non-specific nature of commonly used biomarkers. The history consistent with urinary tract infection and raised inflammatory markers is highly predictive of infection in case 2 with indicators of severe disease (e.g. hypotension) that may indicate sepsis. Similarly, the findings and investigations in the other scenarios also support the diagnosis of a significant inflammatory insult that would prompt many clinicians to consider infection and prescribe empirical broad-spectrum antimicrobials for fear of missing the 1-h window. In scenario 1, although the CRP has not exceeded the severity threshold of > 150 mg/L, the white blood cell count level would contribute to severity prediction using both the Glasgow-Imrie and Ranson’s criteria [62, 63]. Readers may or may not consider PCT to be useful in this case, but it is not commonly performed within the first hour of presentation. Similarly, in scenario 3, findings may suggest infection (and sepsis), although all cultures were consequently negative and a significantly elevated ferritin (56,000 µg/L [10-120]) favours a diagnosis of Still’s disease [64].
Microbiological Diagnosis of Infection
In the absence of a suitable alternative test, detection of pathogens from blood culture samples remains the gold standard for diagnosing blood stream infection. Unfortunately, routine blood cultures may take over 72 h to yield a detectable organism with further time required to identify and test for antibiotic susceptibility. This timeframe is unacceptable in sepsis where delays in treatment worsen morbidity and mortality and contributes to the need for empirical, non-targeted antibiotic therapy [65]. A recent meta-analysis of seven studies including 22,655 patients with sepsis or septic shock identified that only 40.1% of patients had positive blood cultures [66]. This is more pronounced in the neonatal population where, even in symptomatic neonates, only 10 to 15% of blood cultures yield a positive causative result after excluding contaminants [67]. A multitude of factors may contribute to this poor diagnostic yield. For example, the lack of reliable diagnostic criteria for infection in sepsis means that many patients actually have non-infectious inflammatory states due to metabolic, neurological or inflammatory disorders [68]. Many patients are administered antibiotics prior to the development of or worsening of sepsis and prior to blood culture sampling. Cheng et al. demonstrated an absolute difference in the proportion of positive blood cultures between pre- and post-antimicrobial testing of 12.0% [69]. This reduces the probability of pathogen detection [70]. Finally, many common pathogens, including some bacteria, viruses and fungi, are not detectable using conventional culture techniques and rely on surrogate markers such as urinary antigens and non-specific fungal markers. Given the growing incidence of sepsis caused by atypical organisms this may become increasingly problematic [71].
The culture of other fluids and samples, such as urine, sputum, cerebrospinal fluid, faeces, wound and skin swabs, are subject to the same significant time delays as blood culture making them unsuitable for the initial diagnosis of bacterial infection. Essentially any sample may be cultured to identify a causative organism but the results are very variable and often do not yield positive results even in the presence of severe sepsis (a now redundant term) [72, 73]. Simple bedside diagnostic tests tend to lack reliability to exclude infection. Mambatta et al. found the presence of nitrite and leukocyte esterase on urine dipstick analysis to only have a sensitivity of 23.31% and 48.5% respectively [74]. Sputum gram stain has been found to be useful in the aetiologic diagnosis of community acquired pneumonia but is not routinely used and further work is needed to ascertain the impact on clinical outcomes [75].
Novel techniques for pathogen detection may offer an encouraging alternative to conventional methods. Matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF MS) is a rapid diagnostic technology capable of accurately identifying bacteria, yeast, fungi, Nocardia and mycobacteria species as soon as growth on culture is detected [76]. It has been demonstrated to hasten the identification of pathogens by 17 to 34 h, thereby reducing the time taken for effective and optimal antimicrobial strategies in sepsis [77,78,79,80,81,82,83]. These studies also found that MALDI-TOF MS decreased the length of hospital stay by 1.75 to 6 days [78, 82] and improved overall survival by 4 to 9% [78, 83], emphasising the importance of early pathogen recognition. MALDI-TOF MS is currently unable to detect antimicrobial resistance mechanisms and therefore testing antibiotic susceptibility relies upon traditional laboratory techniques [76]. Research to identify spectral peaks that correlate with enzymatic mechanisms of antimicrobial resistance is ongoing and will further increase the value of this technology for tailoring antibiotic therapy [84, 85].
New systems incorporating the polymerase chain reaction (PCR) for microbe amplification, prior to mass spectrometry (MS) detection, have been developed to rapidly accelerate the identification of clinically relevant bacteria and yeast species (turnaround time advertised as 6 to 8 h) with a higher diagnostic yield than blood culture [86]. Furthermore, microorganisms that do not reliably grow in blood cultures may be detectable including Legionella pneumophila, Mycoplasma pneumoniae, Rickettsia typhi, Nocardia spp. and various fungi [87]. Makristathis et al. additionally reported that following prior antimicrobial therapy, positive results were detected in 82.9% of patients with PCR/MS versus only 41.5% with blood cultures [88]. PCR methods enable detection of co-infection with bacteria and viruses which is a frequent phenomenon in community acquired pneumonia [89]. Initial concerns regarding over-sensitivity of these tests due to PCR amplification have been addressed by introducing semi-quantitative methods with an aim to identify and eradicate contaminants. Although commercially available and useful for complementing and expediting microbiological diagnosis of sepsis, these techniques have not yet consistently reached sufficient positive predictive value to replace conventional cultures [90]. They are also unable to identify more than a handful of markers of antibiotic resistance which is an essential factor in providing targeted therapy [91]. Although a promising step forward, these techniques have not yet reached the desired target of accurate detection of organisms with antibiotic susceptibility within a 1 to 3-h window to allow targeted initial management.
PCR has been used in detection of viruses since the late 1980s. For RNA viruses, a reverse transcriptase (RT) process is required to convert the single stranded RNA into complementary DNA. RT-PCR is the frequently used method for detecting viruses due to its low cost, simplicity and high sensitivity [92]. It is limited by a high false positive rate due to contamination and the ability of RT-PCR to detect fragments of non-viable viruses from a previous illness. Real-time quantitative polymerase chain reaction (RT-qPCR) has become the gold standard for virus detection and facilitates quantification of sequences by measuring fluorescence emission during the amplification stage. This provides a high sensitivity and low detection limit [93]. In a sample size of 519 people, Sundell et al. reported the detection of respiratory viruses in asymptomatic individuals was as low as 4.3% from nasopharyngeal swabs suggesting that positive results in symptomatic individuals are likely to be significant [94]. Although bacteria are the predominant causative pathogen for sepsis [95], viruses are often underdiagnosed with several studies detecting viral infection in up to one-third of adults with septic shock [96, 97]. Whilst there is no current recommendation for the use of empirical antiviral therapy in sepsis, it may be prudent to screen for viral infection in patients with severe respiratory illness. This strategy has been widely applied during the COVID-19 pandemic which has mandated the widespread use of real-time PCR testing. Due to the rapid spread of the SARS-CoV-2 virus, rapid antigen lateral flow tests have provided an alternative testing strategy to deliver results in minutes rather than the several days required for PCR in most institutions. The low cost, speed and ease of use of antigen testing is an attractive method for guiding patient management and public health decisions but they lack the sensitivity of PCR, and many have not undergone stringent regulatory review. WHO guidance advises confirmation of positive tests using conventional PCR testing [98].
Future Role of biomarkers, machine learning and gene expression
The absence of an ideal infection or sepsis biomarker has led to the research of hundreds of novel tests [50, 99]. The most extensively investigated include IL6 [100], CD64 [101], presepsin [102], calprotectin [103], sTREM-1 [104] and pentraxin-3 [105]. Unfortunately, many of these tests exhibit the same limitations as conventionally used biomarkers and none have been robustly proven to be superior [99]. Presepsin and CD64 are the most promising biomarkers and are suggested to have a greater sensitivity and shorter time to peak levels than conventional biomarkers although larger studies are required [39, 106]. Studies into novel biomarkers are limited by diverse methodology and small study size with many only having been assessed in populations of < 300 patients. Larger, multi-centre studies are required that account for the heterogeneity of sepsis, before any of these tests change global clinical practice.
Combining several biomarkers has been shown to improve the diagnostic accuracy in sepsis [107, 108]. Han et al. demonstrated the combination of PCT and CRP to have a high ability to discriminate between bacterial sepsis and non-infectious inflammation in the ICU [109]. In a systematic review and meta-analysis including 2661 patients, Ruan et al. reported the same combination to have a higher sensitivity (0.94), AUROC (0.96) and lower negative likelihood ratio (0.89) than CRP or PCT alone in the diagnosis of neonatal sepsis [110]. Similarly, the combination of CD64 and CRP was found to be more sensitive for neonatal sepsis than either measure alone [111]. Combination biomarker panels may also perform better than single biomarkers in predicting prognosis in septic patients [112, 113]. The integration of clinical information into these biomarker panel algorithms may further improve the ability to differentiate between sepsis and non-infectious inflammatory states. In a multi-centre prospective study, Mearelli et al. developed a predictive algorithm incorporating age, SOFA score, recent antimicrobial therapy, hyperthermia and a biomarker panel (white blood cell, CRP, PCT, presepsin, soluble phospholipase A2 group IIA & soluble interleukin-2 receptor α) which demonstrated an high negative predictive value for ruling out sepsis in the Emergency Department [108]. The same authors subsequently demonstrated this algorithm to be superior to qSOFA alone in the prognostication of patients with sepsis [114].
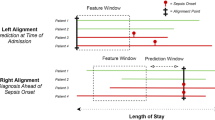
The widespread application of electronic medical records (EMR) in modern clinical practice provides a unique opportunity to analyse large amounts of data within machine learning models. The combination of novel biomarkers with EMR data is suggested to be capable of the early diagnosis and differentiation of sepsis from its mimics [115]. A recent meta-analysis by Islam et al. reported machine learning approaches to perform better than conventional scoring systems for predicting sepsis [116]. Machine learning models are described as being either left-aligned or right-aligned. Left-aligned models are used to predict the onset of sepsis from a fixed point in time — for example from the arrival of the patient into the Emergency Department [117]. The predominant aim of this approach is to expedite the diagnosis and initiation of sepsis treatment to avoid delay. Right-aligned models use large amounts of data to continually predict the development of sepsis following a distinct period of time — effectively the ability to diagnose sepsis before it is clinically evident [118]. The potential value of machine learning algorithms is clear. Fleuren et al. have recently demonstrated in a systematic review and meta-analysis that machine learning models may accurately predict sepsis ahead of time when analysing retrospective data [118]. Unfortunately, significant heterogeneity exists in study methodology, reducing the clinical utility of these models. Additionally, most models have been tested using the MIMIC database which is a freely available clinical database of patients from the Beth Israel Deaconess Medical Center in Boston, USA [119]. This potentially means the models have limited applicability in low- and middle-income countries. Nevertheless, this is an area that is likely to expand dramatically in the coming years. Prospective trials are required to confirm the clinical utility of these models.
The role of host gene response to sepsis is another avenue of research to identify a sepsis signature. These techniques aim to identify specific RNA biomarkers that arise in response to sepsis but not other causes of inflammation. Two such assays are commercially available, the SeptiCyte Lab [120] and the Sepsis MetaScore [121], which have recently been prospectively validated in the ICU population. The AUROC results for diagnosis of sepsis versus non-infectious inflammation was 0.8 for the Sepsis MetaScore and 0.68 for the SeptiCyte Lab [122]. Although this method is not routinely deployed, these findings are encouraging for the role of precision, gene-based medicine in the future of sepsis treatment.
Role of Diagnostic Imaging in Sepsis
Identifying the source of sepsis using diagnostic imaging is essential for providing targeted antimicrobial therapy, disease surveillance and interventional source control. The source of sepsis can guide the clinician to the likely causative pathogen and guide antibiotic class and subtype depending upon regional resistance patterns. In the critically unwell patients, conventional history providing clues as to the origin of infection is often unavailable leading to the reliance on septic screens including microbiological cultures and diagnostic imaging. Imaging will also enable diagnosis of sepsis mimics, such as acute pulmonary embolus and acute pancreatitis, which require alternative management and can avoid the unnecessary administration of antimicrobials. The optimal imaging modality is dependent upon the suspected source and balanced against the risks of cumulative radiation exposure and moving critically unwell patients.
The chest radiograph (CXR) is the most commonly performed radiological investigation in sepsis [123] which is unsurprising considering respiratory infections are by far the most common source [95]. In many centres, CXR is regularly performed to confirm the position of medical devices, such as nasogastric tubes and central venous catheters, allowing for the incidental identification and surveillance of pathology. Unfortunately, many features of pulmonary consolidation are non-specific for infection and the quality of portable imaging in unwell patients further worsens its performance [124]. Airspace opacities on CXR in ICU may reflect infection, atelectasis, oedema, haemorrhage, inflammation, drug or transfusion reaction or acute respiratory distress syndrome [125]. Winkler et al. in a meta-analysis including 543 patients found CXR to only have a sensitivity of 49% for identifying causative pathology in the ICU [126]. Additionally, the risk of cumulative radiation exposure continues to be a concern in patients with long term critical illness. Machine learning has been reported to increase the diagnostic capability of CXR although is not widely applied. In a systematic review and meta-analysis, Li et al. reported deep learning algorithms to perform with high accuracy for the detection of pneumonia with an AUROC of 0.99 and the ability to differentiate viral from bacterial pneumonia with an AUROC of 0.95 [127]. Recent studies have applied machine learning to CXR interpretation in the COVID-19 pandemic with encouraging results [128].
Recent technological advances in the quality and portability of ultrasound devices have led to the widespread use of point of care ultrasound to assess the lung parenchyma. Several systematic reviews and meta-analyses have found lung US to be superior to CXR for the diagnosis of pneumonia [126, 129,130,131,132,133]. Serial assessments may be performed without repeated exposure to ionising radiation. However, ultrasound is limited to the identification of pathology extending to the lung peripheries due to the high acoustic impedance of air upon ultrasound waves. Similarly, ultrasound is highly user dependent, requires dedicated training and is time consuming for busy clinicians leading to continued reliance on CXR and computerised tomography (CT) imaging [134].
Ultrasound is recommended as the first line imaging modality in suspected biliary tree pathology [135]. It is reported to have a sensitivity of 81% for the diagnosis of acute cholecystitis and 85–95% for the detection of biliary dilatation [136, 137]. Only if the ultrasound is equivocal should further imaging such as magnetic resonance cholangiopancreatography (MRCP) or cholescintigraphy be performed.
Ultrasound, in the form of echocardiography, is the imaging modality of choice in suspected infective endocarditis. 2D transthoracic echocardiography (TTE) is invariably the initial investigation due to being non-invasive, low cost and portable with a sensitivity of 70% and specificity of 90% for native valve infective endocarditis [138, 139]. Transoesophageal echocardiography (TOE) is superior to TTE with a sensitivity of 96% but at the expense of being an invasive procedure with significant potential complications [138, 140]. The sensitivity of both modalities falls in the setting of prosthetic valve endocarditis (TTE 50% versus TOE 92%) but it remains an important investigation to assess ventricular size, performance and valvular dysfunction [141]. Whilst a normal TOE is highly suggestive of a negative diagnosis of endocarditis, it cannot unequivocally be excluded and current guidance recommends that a repeat TOE should be performed after 7–10 days in cases with a high index of suspicion [142]. Diagnosis may be particularly challenging with prosthetic valves (infective endocarditis versus thrombus versus pannus), intracardiac devices, small vegetations, abscesses and in patients with pre-existing valvular lesions such as mitral valve prolapse or degenerative calcific disease. In challenging cases, modern alternative imaging techniques may be deployed such as multi-slice computed tomography (MSCT), magnetic resonance imaging (MRI), 18F-fluorodeoxyglucose (FDG) positron emission tomography (PET)/CT or other functional imaging techniques [139].
CT has emerged as the gold standard investigation for many potential sources of infection. It is highly sensitive and specific for the diagnosis of pneumonia and enables differentiation of infective patterns including focal, lobar, bronchopneumonia, interstitial, ground glass, nodular, tree-in-bud and halo sign opacities. These pattern subtypes may provide clues as to the likely causative organisms and guide further investigation [143]. CT is suggested to reduce the overdiagnosis of pneumonia when compared with CXR, therefore lowering the inappropriate administration of antimicrobial agents [144]. Incidental radiological findings, such as pulmonary nodules, may be seen in up to one third of elderly patients undergoing imaging for pneumonia providing an opportunity to diagnose and treat unexpected pathology [145]. In a case series of patients with CXR diagnosed community acquired pneumonia admitted to the ICU, Karhu et al. found CT to yield new findings in 58.5% of patients. Of these patients, 76.5% subsequently underwent further diagnostic or therapeutic interventions based upon the CT findings [146].
CT is the diagnostic modality of choice for peritonitis. In a retrospective analysis of 251 patients with post-operative sepsis, Bader et al. found CT to have a diagnostic sensitivity of 97.2% when compared with conventional radiography (66.2%) and US (44.3%) [147]. It can readily identify intra-abdominal infection in ICU patients who have sustained major trauma; a cohort who invariably have signs of systemic inflammatory response with or without infection [148]. Furthermore, CT can accurately identify intra and retroperitoneal collections and guide drainage to avoid the requirement for invasive surgery. Although the safety and success rate of percutaneous drainage of intra-abdominal collections was conventionally considered to be safer with CT compared with ultrasound [149], many modern techniques will use both modalities to enhance outcomes [150]. CT-guided fine needle aspiration (FNA) is the gold standard for diagnosing infected pancreatic necrosis but is not frequently deployed due to the high rate of false negative findings [52]. In the context of severe acute pancreatitis, retroperitoneal gas is considered to be indicative of infection but has a low negative predictive value [151]. This further adds to the dilemma of diagnosing pancreatic infection and promotes the excessive use of empirical antimicrobials.
The high diagnostic utility of CT must be balanced against the risk of transporting acutely unwell patients and the cumulative risk of cancer due to radiation exposure. Radiation dosage depends upon the type of CT but is estimated to range from 1–15 millisieverts (mSv) [152]. The use of CT imaging in children has been found to triple the risk of developing leukaemia and brain tumours [153, 154]. In adults, much of the large population data suggesting the increased cancer risk due to low-level radiation exposure is derived from atomic bomb survivors [155] and workers in the nuclear industry [156]. For context, these sub-groups received radiation doses ranging from 5 to 20 mSv which is the equivalent of 1 to 2 CT scans. Radiation is thought to contribute to 2% of all deaths in this group. Based upon these findings, Shao et al. conducted a retrospective cohort study assessing 56,050 cases of thyroid cancer, leukaemia and non-Hodgkin lymphoma (NHL) in Taiwan and identified a small but significant increase in risk in patients under 45 exposed to medical radiation [152]. The odds ratios for thyroid cancer, leukaemia and NHL for all populations were 2.55, 1.55 and 1.05, respectively. There was a threefold increase in NHL in individuals aged under 45. Whilst the individual risk is low, the increased prevalence of CT imaging is likely to have an impact at a public health level.
FDG-PET/CT has emerged as a useful second line investigation in patients with sepsis of unknown origin and Staphylococcus aureus bacteraemia. Areas of active infection are identified as abnormal areas of glucose metabolism due to increased glycolysis by activated white blood cells [157]. FDG-PET/CT exposes the patient to less radiation than a CT scan of the abdomen and pelvis with contrast and can identify many potential foci of infection within one investigation. Whilst potentially appealing, its use is limited by cost and required reporting time. The cost of PET/CT in the UK is £909 compared with around £140 for a CT scan [158]. The diagnostic advantage and cost-effectiveness will need to be justified prior to PET/CT being offered on a routine basis. Recent statistics suggest that the median timeframe from imaging request to being performed is 7 days with a further 2 days required for reporting [159]. This delay is likely to be considered unacceptable for critically unwell patients and promotes continued reliance on conventional imaging techniques.
In the absence of conclusive radiological diagnosis or if a patient is too unstable for imaging, bedside diagnostic laparoscopy may yield important information and negate the requirement for non-therapeutic laparotomy. Alemanno et al. recently reviewed 129 patients that underwent bedside diagnostic laparoscopy within their ICU, including 25 patients with unexplained sepsis. Findings were compared against 154 ICU patients who underwent exploratory laparotomy in the operating suite. They conclude bedside diagnostic laparoscopy in the ICU setting can be considered an option for cases with suggestive, but non-conclusive, laparotomy or radiological results, or in the rare case in which it is unsafe to transfer a critically ill patient to the radiology department [160]. Although large scale studies will be difficult to justify, diagnostic laparoscopy either at the bedside or in the operating department remains a consideration in individual cases.
Conclusions
The prompt recognition and targeted treatment of sepsis is essential to improve clinical outcomes. We have considered the role of screening tools, clinical assessment, biomarkers, microbiology and imaging in the diagnosis of infection and highlighted the strengths and limitations associated with each. To date, there is no diagnostic tool able to rapidly identify or exclude infection. The lack of a reliable diagnostic tool contributes to the high quantities of broad-spectrum antimicrobial therapy used globally and is likely to lead to under-recognition (and over-treatment) of non-infectious inflammatory states. Given the increasing prevalence of antibiotic resistance, there is an ever-pressing need for novel solutions. Combining machine learning models with biomarkers, gene markers and EMR data may improve the utility of screening tools but requires further work. The identification and management of sepsis continues to rely on thorough patient assessment and sound clinical judgement. Novel techniques should complement, not replace, these fundamental elements of patient care.
References
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). J Am Med Assoc. 2016;315:801–10.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Crit Care Med. 2017;45:486–552.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992;101:1644–1655.
Sprung CL, Sakr Y, Vincent JL, Le Gall JR, Reinhart K, Ranieri VM, Gerlach H, Fielden J, Groba CB, Payen D. An evaluation of systemic inflammatory response syndrome signs in the Sepsis Occurrence In Acutely Ill Patients (SOAP) study. Intensive Care Med. 2006;32:421–7.
Lai NA, Kruger P. The predictive ability of a weighted systemic inflammatory response syndrome score for microbiologically confirmed infection in hospitalised patients with suspected sepsis. Crit Care Resusc. 2011;13:146–50.
Shibata K. Funada H [The epidemiology of SIRS.sepsis in Japan]. Nihon Rinsho. 2004;62:2184–8.
Brun-Buisson C. The epidemiology of the systemic inflammatory response. Intensive Care Med. 2000;26:S064–74.
Kaukonen KM, Bailey M, Pilcher D, Cooper DJ, Bellomo R. Systemic inflammatory response syndrome criteria in defining severe sepsis. N Engl J Med. 2015;372:1629–38.
Levy MM, Dellinger RP, Townsend SR, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Intensive Care Med. 2010;36:222–31.
Jones SL, Ashton CM, Kiehne L, Gigliotti E, Bell-Gordon C, Disbot M, Masud F, Shirkey BA, Wray NP. Reductions in sepsis mortality and costs after design and implementation of a nurse-based early recognition and response program. Jt Comm J Qual Patient Saf. 2015;41:483–91.
Damiani E, Donati A, Serafini G, Rinaldi L, Adrario E, Pelaia P, Busani S, Girardis M. Effect of performance improvement programs on compliance with sepsis bundles and mortality: a systematic review and meta-analysis of observational studies. PLoS ONE. 2015;10:e0125827–e0125827.
Singer M, Shankar-Hari M. qSOFA. Cue Confusion Ann Intern Med. 2018;168:293.
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, Rubenfeld G, Kahn JM, Shankar-Hari M, Singer M. Assessment of clinical criteria for sepsis: for the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:762–74.
UK NSC: evidence review process. https://www.gov.uk/government/publications/uk-nsc-evidence-review-process/uk-nsc-evidence-review-process.
Pandharipande PP, Shintani AK, Hagerman HE, St Jacques PJ, Rice TW, Sanders NW, Ware LB, Bernard GR, Ely EW. Derivation and validation of Spo2/Fio2 ratio to impute for Pao2/Fio2 ratio in the respiratory component of the Sequential Organ Failure Assessment score. Crit Care Med. 2009;37:1317–21.
Stevens JP, Kachniarz B, Wright SB, Gillis J, Talmor D, Clardy P, Howell MD. When Policy Gets It Right: Variability in U.S. Hospitals’ diagnosis of ventilator-Associated pneumonia. Crit Care Med 2014;42:497–503.
Lopansri BK, Miller Iii RR, Burke JP, et al. Physician agreement on the diagnosis of sepsis in the intensive care unit: estimation of concordance and analysis of underlying factors in a multicenter cohort. J Intensive Care. 2019;7:13.
Rhee C, Kadri SS, Danner RL, Suffredini AF, Massaro AF, Kitch BT, Lee G, Klompas M. Diagnosing sepsis is subjective and highly variable: a survey of intensivists using case vignettes. Crit Care. 2016;20:89.
Peltola V, Reunanen T, Ziegler T, Silvennoinen H, Heikkinen T. Accuracy of Clinical Diagnosis of Influenza in Outpatient Children. Clin Infect Dis. 2005;41:1198–200.
Craig JC, Williams GJ, Jones M, Codarini M, Macaskill P, Hayen A, Irwig L, Fitzgerald DA, Isaacs D, McCaskill M. The accuracy of clinical symptoms and signs for the diagnosis of serious bacterial infection in young febrile children: prospective cohort study of 15 781 febrile illnesses. BMJ 2010;340:c1594.
Barrie J, Jamdar S, Smith N, McPherson SJ, Siriwardena AK, O’Reilly DA. Mis-use of antibiotics in acute pancreatitis: Insights from the United Kingdom’s National Confidential Enquiry into patient outcome and death (NCEPOD) survey of acute pancreatitis. Pancreatology. 2018;18:721–6.
Abdul-Aziz MH, Lipman J, Akova M, et al. Is prolonged infusion of piperacillin/tazobactam and meropenem in critically ill patients associated with improved pharmacokinetic/pharmacodynamic and patient outcomes? An observation from the Defining Antibiotic Levels in Intensive care unit patients (DA. J Antimicrob Chemother. 2016;71:196–207.
Goodchild G, Chouhan M, Johnson GJ. Practical guide to the management of acute pancreatitis. Frontline Gastroenterol. 2019;10:292–9.
Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011;46:261–70.
Marik PE, Stephenson E. The ability of Procalcitonin, lactate, white blood cell count and neutrophil-lymphocyte count ratio to predict blood stream infection. Analysis of a large database. J Crit Care 2020;60:135–139.
Seigel TA, Cocchi MN, Salciccioli J, Shapiro NI, Howell M, Tang A, Donnino MW. Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J Emerg Med. 2012;42:254–9.
Van den Bruel A, Thompson MJ, Haj-Hassan T, Stevens R, Moll H, Lakhanpaul M, Mant D. Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ 2011;342:d3082.
Panagiotopoulou IG, Parashar D, Lin R, Antonowicz S, Wells AD, Bajwa FM, Krijgsman B. The diagnostic value of white cell count, C-reactive protein and bilirubin in acute appendicitis and its complications. Ann R Coll Surg Engl. 2013;95:215–21.
Warschkow R, Tarantino I, Torzewski M, Näf F, Lange J, Steffen T. Diagnostic accuracy of C-reactive protein and white blood cell counts in the early detection of inflammatory complications after open resection of colorectal cancer: a retrospective study of 1,187 patients. Int J Colorectal Dis. 2011;26:1405–13.
Orfanu AE, Popescu C, Leuștean A, Negru AR, Tilişcan C, Aramă V, Aramă ȘS. The Importance of Haemogram Parameters in the Diagnosis and Prognosis of Septic Patients. J Crit Care Med. 2017;3:105–10.
Farkas JD. The complete blood count to diagnose septic shock. J Thorac Dis. 2020;12:S16–21.
Azab B, Camacho-Rivera M, Taioli E. Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLoS One 2014;9:e112361.
de Jager CPC, van Wijk PTL, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, Wever PC. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care. 2010;14:R192.
Ljungström L, Pernestig A-K, Jacobsson G, Andersson R, Usener B, Tilevik D. Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS One 2017;12:e0181704.
Liu J, Liu Y, Xiang P, et al. Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med. 2020;18:206.
Westerdijk K, Simons KS, Zegers M, Wever PC, Pickkers P, de Jager CPC. The value of the neutrophil-lymphocyte count ratio in the diagnosis of sepsis in patients admitted to the Intensive Care Unit: A retrospective cohort study. PLoS One 2019;14:e0212861.
Kolb-Bachofen V. A Review on the Biological Properties of C-Reactive Protein. Immunobiology. 1991;183:133–45.
Markanday A. Acute Phase Reactants in Infections: Evidence-Based Review and a Guide for Clinicians. Open Forum Infect Dis. https://doi.org/10.1093/ofid/ofv098.
Wu CC, Lan HM, Han ST, Chaou CH, Yeh CF, Liu SH, Li CH, Blaney GN, Liu ZY, Chen KF. Comparison of diagnostic accuracy in sepsis between presepsin, procalcitonin, and C-reactive protein: a systematic review and meta-analysis. Ann Intensive Care. 2017;7:91.
Tan M, Lu Y, Jiang H, Zhang L. The diagnostic accuracy of procalcitonin and C-reactive protein for sepsis: A systematic review and meta-analysis. J Cell Biochem. 2019;120:5852–9.
Stirling AD, Moran NR, Kelly ME, Ridgway PF, Conlon KC. The predictive value of C-reactive protein (CRP) in acute pancreatitis – is interval change in CRP an additional indicator of severity? HPB. 2017;19:874–80.
Khanna AK, Meher S, Prakash S, Tiwary SK, Singh U, Srivastava A, Dixit VK. Comparison of Ranson, Glasgow, MOSS, SIRS, BISAP, APACHE-II, CTSI Scores, IL-6, CRP, and Procalcitonin in Predicting Severity, Organ Failure, Pancreatic Necrosis, and Mortality in Acute Pancreatitis. HPB Surg. 2013;2013:1–10.
Póvoa P, Coelho L, Almeida E, Fernandes A, Mealha R, Moreira P, Sabino H. Early identification of intensive care unit-acquired infections with daily monitoring of C-reactive protein: a prospective observational study. Crit Care. 2006;10:R63.
Jekarl DW, Lee S, Kim M, Kim Y, Woo SH, Lee WJ. Procalcitonin as a prognostic marker for sepsis based on SEPSIS-3. J Clin Lab Anal. 2019;33:22996.
Assicot M, Bohuon C, Gendrel D, Raymond J, Carsin H, Guilbaud J. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993;341:515–8.
Oussalah A, Ferrand J, Filhine-Tresarrieu P, Aissa N, Aimone-Gastin I, Namour F, Garcia M, Lozniewski A, Gueánt JL. Diagnostic accuracy of procalcitonin for predicting blood culture results in patients with suspected bloodstream infection. Med (United States) 2015;94:e1774.
Klastersky J. Empirical antifungal therapy. Int J Antimicrob Agents. 2004;23:105–12.
Thomas-Rüddel DO, Poidinger B, Kott M, Weiss M, Reinhart K, Bloos F, MEDUSA study group. Influence of pathogen and focus of infection on procalcitonin values in sepsis patients with bacteremia or candidemia. Crit Care 2018;22:128.
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:426–35.
Heffernan AJ, Denny KJ. Host diagnostic biomarkers of infection in the ICU: where are we and where are we going? Curr Infect Dis Rep. 2021;23:4.
Rau B, Steinbach G, Baumgart K, Gansauge F, Grünert A, Beger HG. The clinical value of procalcitonin in the prediction of infected necrois in acute pancreatitis. Intensive Care Med. 2000;26:S159–64.
Leppäniemi A, Tolonen M, Tarasconi A, et al. 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg. 2019;14:1–20.
Mofidi R, Suttie SA, Patil PV, Ogston S, Parks RW. The value of procalcitonin at predicting the severity of acute pancreatitis and development of infected pancreatic necrosis: systematic review. Surgery. 2009;146:72–81.
Kamat IS, Ramachandran V, Eswaran H, Guffey D, Musher DM. Procalcitonin to distinguish viral from bacterial pneumonia: a systematic review and meta-analysis. Clin Infect Dis. 2020;70:538–42.
El-Sayed D, Grotts J, Golgert WA, Sugar AM. Sensitivity and specificity of procalcitonin in predicting bacterial infections in patients with renal impairment. Open Forum Infect Dis. 2014;1:1–7.
Hoeboer SH, van der Geest PJ, Nieboer D, Groeneveld ABJ. The diagnostic accuracy of procalcitonin for bacteraemia: A systematic review and meta-analysis. Clin Microbiol Infect. 2015;21:474–81.
Joo K, Park W, Lim MJ, Kwon SR, Yoon J. Serum procalcitonin for differentiating bacterial infection from disease flares in patients with autoimmune diseases. J Korean Med Sci. 2011;26:1147–51.
Iankova I, Thompson-Leduc P, Kirson NY, Rice B, Hey J, Krause A, Schonfeld SA, Debrase CR, Bozzette S, Schuetz P. Efficacy and safety of procalcitonin guidance in patients with suspected or confirmed sepsis: A systematic review and meta-analysis. Crit Care Med. 2018;46:691–8.
Wirz Y, Meier MA, Bouadma L, et al. Effect of procalcitonin-guided antibiotic treatment on clinical outcomes in intensive care unit patients with infection and sepsis patients: a patient-level meta-analysis of randomized trials. Crit Care. 2018;22:191.
Meier MA, Branche A, Neeser OL, et al. Procalcitonin-guided antibiotic treatment in patients with positive blood cultures: a patient-level meta-analysis of randomized trials. Clin Infect Dis. 2019;69:388–96.
Cole K, Phlamon M, Petite SE. Comparison of short-course and prolonged antimicrobial therapy in the management of intra-abdominal infections. Surg Infect (Larchmt). 2019;20:519–23.
Blamey SL, Imrie CW, O’Neill J, Gilmour WH, Carter DC. Prognostic factors in acute pancreatitis Gut. 1984;25:1340–6.
Ranson JH, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer FC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet. 1974;139:69–81.
Mehta B, Efthimiou P. Ferritin in adult-onset still’s disease: just a useful innocent bystander? Int J Inflam. 2012;2012:1–7.
Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96.
Li Y, Guo J, Yang H, Li H, Shen Y, Zhang D. Comparison of culture-negative and culture-positive sepsis or septic shock: a systematic review and meta-analysis. Crit Care. 2021;25:167.
Blackburn RM, Muller-Pebody B, Planche T, Johnson A, Hopkins S, Sharland M, Kennea N, Heath PT. Neonatal sepsis–many blood samples, few positive cultures: implications for improving antibiotic prescribing. Arch Dis Child Fetal Neonatal Ed. 2012;97:F487–8.
Cohen J, Brun-Buisson C, Torres A, Jorgensen J. Diagnosis of infection in sepsis: an evidence-based review. Crit Care Med. 2004;32:S466–94.
Cheng MP, Stenstrom R, Paquette K, et al. Blood culture results before and after antimicrobial administration in patients with severe manifestations of sepsis: a diagnostic study. Ann Intern Med. 2019;171:547–54.
Scheer CS, Fuchs C, Gründling M, Vollmer M, Bast J, Bohnert JA, Zimmermann K, Hahnenkamp K, Rehberg S, Kuhn SO. Impact of antibiotic administration on blood culture positivity at the beginning of sepsis: a prospective clinical cohort study. Clin Microbiol Infect. 2019;25:326–31.
Lin GL, McGinley JP, Drysdale SB, Pollard AJ. Epidemiology and Immune Pathogenesis of Viral Sepsis. Front Immunol. 2018;9:2147.
Lee JY, Cho SY, Hwang HSH, Ryu JY, Lee J, Song I Do, Kim BJ, Kim JW, Chang SK, Choi CH. Diagnostic yield of stool culture and predictive factors for positive culture in patients with diarrheal illness. Medicine (Baltimore) 2017;96:e7641.
Brouwer MC, Tunkel AR, van de Beek D. Epidemiology, diagnosis, and antimicrobial treatment of acute bacterial meningitis. Clin Microbiol Rev. 2010;23:467–92.
Mambatta A, Rashme V, Menon S, Jayarajan J, Harini S, Kuppusamy J. Reliability of dipstick assay in predicting urinary tract infection. J Fam Med Prim Care. 2015;4:265.
Del Rio-Pertuz G, Gutiérrez JF, Triana AJ, et al. Usefulness of sputum gram stain for etiologic diagnosis in community-acquired pneumonia: a systematic review and meta-analysis. BMC Infect Dis. 2019;19:1–12.
Luethy PM, Johnson JK. The Use of Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS) for the Identification of Pathogens Causing Sepsis. J Appl Lab Med. 2019;3:675–85.
Delport JA, Strikwerda A, Armstrong A, Schaus D, John M. Quality of care is improved by rapid short incubation MALDI-ToF identification from blood cultures as measured by reduced length of stay and patient outcomes as part of a multi-disciplinary approach to bacteremia in pediatric patients. PLoS One 2016;11:e0160618.
Delport JA, Strikwerda A, Armstrong A, Schaus D, John M. MALDI-ToF short incubation identification from blood cultures is associated with reduced length of hospitalization and a decrease in bacteremia associated mortality. Eur J Clin Microbiol Infect Dis. 2017;36:1181–6.
Curtoni A, Cipriani R, Marra ES, Barbui AM, Cavallo R, Costa C. Rapid identification of microorganisms from positive blood culture by MALDI-TOF MS after short-term incubation on solid medium. Curr Microbiol. 2017;74:97–102.
Huang AM, Newton D, Kunapuli A, Gandhi TN, Washer LL, Isip J, Collins CD, Nagel JL. Impact of rapid organism identification via matrix-assisted laser desorption/ionization time-of-flight combined with antimicrobial stewardship team intervention in adult patients with bacteremia and candidemia. Clin Infect Dis. 2013;57:1237–45.
Malcolmson C, Ng K, Hughes S, Kissoon N, Schina J, Tilley PA, Roberts A. Impact of matrix-assisted laser desorption and ionization time-of-flight and antimicrobial stewardship intervention on treatment of bloodstream infections in hospitalized children. J Pediatric Infect Dis Soc 2016;6:piw033.
Beganovic M, Costello M, Wieczorkiewicz SM. Effect of matrix-assisted laser desorption ionization–time of flight mass spectrometry (MALDI-TOF MS) alone versus MALDI-TOF MS combined with real-time antimicrobial stewardship interventions on time to optimal antimicrobial therapy in patients with posit. J Clin Microbiol. 2017;55:1437–45.
Patel TS, Kaakeh R, Nagel JL, Newton DW, Stevenson JG. Cost Analysis of implementing matrix-assisted laser desorption ionization–time of flight mass spectrometry plus real-time antimicrobial stewardship intervention for bloodstream infections. J Clin Microbiol. 2017;55:60–7.
Burckhardt I, Zimmermann S. Using matrix-assisted laser desorption ionization-time of flight mass spectrometry to detect carbapenem resistance within 1 to 2.5 hours. J Clin Microbiol 2011;49:3321–3324.
Jung JS, Popp C, Sparbier K, Lange C, Kostrzewa M, Schubert S. Evaluation of matrix-assisted laser desorption ionization-time of flight mass spectrometry for rapid detection of -lactam resistance in enterobacteriaceae derived from blood cultures. J Clin Microbiol. 2014;52:924–30.
Westh H, Lisby G, Breysse F, et al. Multiplex real-time PCR and blood culture for identification of bloodstream pathogens in patients with suspected sepsis. Clin Microbiol Infect. 2009;15:544–51.
Mustafa MIA, Al-Marzooq F, How SH, Kuan YC, Ng TH. The use of multiplex real-time PCR improves the detection of the bacterial etiology of community acquired pneumonia. Trop Biomed. 2011;28:531–44.
Makristathis A, Harrison N, Ratzinger F, Kussmann M, Selitsch B, Forstner C, Hirschl AM, Burgmann H. Substantial diagnostic impact of blood culture independent molecular methods in bloodstream infections: Superior performance of PCR/ESI-MS. Sci Rep. 2018;8:16024.
Johansson N, Kalin M, Annika TL, Giske CG, Hedlund J. Etiology of community-acquired pneumonia: Increased microbiological yield with new diagnostic methods. Clin Infect Dis. 2010;50:202–9.
van de Groep K, Bos MP, Varkila MRJ, Savelkoul PHM, Ong DSY, Derde LPG, Juffermans NP, van der Poll T, Bonten MJM, Cremer OL. Moderate positive predictive value of a multiplex real-time PCR on whole blood for pathogen detection in critically ill patients with sepsis. Eur J Clin Microbiol Infect Dis. 2019;38:1829–36.
Sinha M, Jupe J, Mack H, Coleman TP, Lawrence SM, Fraley SI. Emerging technologies for molecular diagnosis of sepsis. Clin Microbiol Rev. 2018;31:1–26.
Choudhary ML, Anand SP, Tikhe SA, Walimbe AM, Potdar VA, Chadha MS, Mishra AC. Comparison of the conventional multiplex RT-PCR, real time RT-PCR and Luminex xTAG® RVP fast assay for the detection of respiratory viruses. J Med Virol. 2016;88:51–7.
Navarro E, Serrano-Heras G, Castaño MJ, Solera J. Real-time PCR detection chemistry. Clin Chim Acta. 2015;439:231–50.
Sundell N, Andersson L-M, Brittain-Long R, Sundvall P-D, Alsiö Å, Lindh M, Gustavsson L, Westin J. PCR detection of respiratory pathogens in asymptomatic and symptomatic adults. J Clin Microbiol. https://doi.org/10.1128/JCM.00716-18.
Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54.
Sudarmono P, Aman AT, Arif M, et al. Causes and outcomes of sepsis in southeast Asia: a multinational multicentre cross-sectional study. Lancet Glob Heal. 2017;5:e157–67.
Ljungström LR, Jacobsson G, Claesson BEB, Andersson R, Enroth H. Respiratory viral infections are underdiagnosed in patients with suspected sepsis. Eur J Clin Microbiol Infect Dis. 2017;36:1767–76.
World Health Organization. Antigen-detection in the diagnosis of SARS-CoV-2 infection using rapid immunoassays Interim guidance.
Pierrakos C, Velissaris D, Bisdorff M, Marshall JC, Vincent JL. Biomarkers of sepsis: Time for a reappraisal. Crit Care. 2020;24:1–15.
Ma L, Zhang H, Yin Y ling, Guo W zhi, Ma Y qun, Wang Y bo, Shu C, Dong L qiang. Role of interleukin-6 to differentiate sepsis from non-infectious systemic inflammatory response syndrome. Cytokine 2016;88:126–135.
Yin W, Li J, Zheng X, An L, Shao H, Li C. Effect of neutrophil CD64 for diagnosing sepsis in emergency department. World J Emerg Med. 2020;11:79.
Kweon OJ, Choi JH, Park SK, Park AJ. Usefulness of presepsin (sCD14 subtype) measurements as a new marker for the diagnosis and prediction of disease severity of sepsis in the Korean population. J Crit Care. 2014;29:965–70.
Larsson A, Tydén J, Johansson J, Lipcsey M, Bergquist M, Kultima K, Mandic-Havelka A. Calprotectin is superior to procalcitonin as a sepsis marker and predictor of 30-day mortality in intensive care patients. Scand J Clin Lab Invest. 2020;80:156–61.
Brenner T, Uhle F, Fleming T, et al. Soluble TREM-1 as a diagnostic and prognostic biomarker in patients with septic shock: an observational clinical study. Biomarkers. 2017;22:63–9.
Hamed S, Behnes M, Pauly D, et al. Diagnostic value of Pentraxin-3 in patients with sepsis and septic shock in accordance with latest sepsis-3 definitions. BMC Infect Dis. https://doi.org/10.1186/s12879-017-2606-3.
Jämsä J, Ala-Kokko T, Huotari V, Ohtonen P, Savolainen ER, Syrjälä H. Neutrophil CD64, C-reactive protein, and procalcitonin in the identification of sepsis in the ICU — Post-test probabilities. J Crit Care. 2018;43:139–42.
Grover V, Pantelidis P, Soni N, Takata M, Shah PL, Wells AU, Henderson DC, Kelleher P, Singh S. A biomarker panel (Bioscore) incorporating monocytic surface and soluble TREM-1 has high discriminative value for ventilator-associated pneumonia: A prospective observational study. PLoS One 2014;9:e109686.
Mearelli F, Fiotti N, Giansante C, et al. Derivation and validation of a biomarker-based clinical algorithm to rule out sepsis from noninfectious systemic inflammatory response syndrome at emergency department admission: a multicenter prospective study. Crit Care Med. 2018;46:1421–9.
Han JH, Nachamkin I, Coffin SE, et al. Use of a combination biomarker algorithm to identify medical intensive care unit patients with suspected sepsis at very low likelihood of bacterial infection. Antimicrob Agents Chemother. 2015;59:6494–500.
Ruan L, Chen GY, Liu Z, Zhao Y, Xu GY, Li SF, Li CN, Chen LS, Tao Z. The combination of procalcitonin and C-reactive protein or presepsin alone improves the accuracy of diagnosis of neonatal sepsis: A meta-analysis and systematic review. Crit Care. 2018;22:1–9.
Shi J, Tang J, Chen D. Meta-analysis of diagnostic accuracy of neutrophil CD64 for neonatal sepsis. Ital J Pediatr. https://doi.org/10.1186/s13052-016-0268-1.
Kim H, Hur M, Moon HW, Yun YM, Di Somma S. Multi-marker approach using procalcitonin, presepsin, galectin-3, and soluble suppression of tumorigenicity 2 for the prediction of mortality in sepsis. Ann Intensive Care. 2017;7:27.
Mikacenic C, Price BL, Harju-Baker S, et al. A two-biomarker model predicts mortality in the critically Ill with sepsis. Am J Respir Crit Care Med. 2017;196:1004–11.
Mearelli F, Barbati G, Casarsa C, et al. The Integration of qSOFA with Clinical Variables and Serum Biomarkers Improves the Prognostic Value of qSOFA Alone in Patients with Suspected or Confirmed Sepsis at ED Admission. J Clin Med 2020;9:1205.
Taneja I, Reddy B, Damhorst G, et al. Combining Biomarkers with EMR Data to Identify Patients in Different Phases of Sepsis. Sci Rep. 2017;7:10800.
Islam MM, Nasrin T, Walther BA, Wu CC, Yang HC, Li YC. Prediction of sepsis patients using machine learning approach: A meta-analysis. Comput Methods Programs Biomed. 2019;170:1–9.
Nachimuthu SK, Haug PJ. Early detection of sepsis in the emergency department using Dynamic Bayesian Networks. AMIA Annu Symp proceedings AMIA Symp. 2012;2012:653–62.
Fleuren LM, Klausch TLT, Zwager CL, et al. Machine learning for the prediction of sepsis: a systematic review and meta-analysis of diagnostic test accuracy. Intensive Care Med. 2020;46:383–400.
Johnson AEW, Pollard TJ, Shen L, Lehman L-WH, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci data 2016;3:160035.
McHugh L, Seldon TA, Brandon RA, et al. A Molecular Host Response Assay to Discriminate Between Sepsis and Infection-Negative Systemic Inflammation in Critically Ill Patients: Discovery and Validation in Independent Cohorts. PLoS Med 2015;12:e1001916.
Sweeney TE, Shidham A, Wong HR, Khatri P. A comprehensive time-course-based multicohort analysis of sepsis and sterile inflammation reveals a robust diagnostic gene set. Sci Transl Med 2015;7:287ra71.
Maslove DM, Shapira T, Tyryshkin K, Veldhoen RA, Marshall JC, Muscedere J. Validation of diagnostic gene sets to identify critically ill patients with sepsis. J Crit Care. 2019;49:92–8.
Lohan R. Imaging of ICU Patients. Thorac Imaging 2019;173–194.
Yu CJ, Yang PC, Chang DB, Luh KT. Diagnostic and therapeutic use of chest sonography: Value in critically ill patients. Am J Roentgenol. 1992;159:695–701.
Rubinowitz AN, Siegel MD, Tocino I. Thoracic Imaging in the ICU. Crit Care Clin. 2007;23:539–73.
Winkler MH, Touw HR, van de Ven PM, Twisk J, Tuinman PR. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung ultrasound, in critically ill patients with respiratory symptoms: a systematic review and meta-analysis. Crit Care Med. 2018;46:e707–14.
Li Y, Zhang Z, Dai C, Dong Q, Badrigilan S. Accuracy of deep learning for automated detection of pneumonia using chest X-Ray images: a systematic review and meta-analysis. Comput Biol Med 2020;123:103898.
Castiglioni I, Ippolito D, Interlenghi M, Monti CB, Salvatore C, Schiaffino S, Polidori A, Gandola D, Messa C, Sardanelli F. Machine learning applied on chest x-ray can aid in the diagnosis of COVID-19: a first experience from Lombardy. Italy Eur Radiol Exp. 2021;5:1–10.
Alzahrani SA, Al-Salamah MA, Al-Madani WH, Elbarbary MA. Systematic review and meta-analysis for the use of ultrasound versus radiology in diagnosing of pneumonia. Crit Ultrasound J. 2017;9:6.
Maw AM, Hassanin A, Ho PM, et al. Diagnostic accuracy of point-of-care lung ultrasonography and chest radiography in adults with symptoms suggestive of acute decompensated heart failure: a systematic review and meta-analysis. JAMA Netw Open 2019;2:e190703.
Chavez MA, Shams N, Ellington LE, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res. 2014;15:1–9.
Xin H, Li J, Hu HY. Is lung ultrasound useful for diagnosing pneumonia in children?: A meta-analysis and systematic review. Ultrasound Q. 2018;34:3–10.
Orso D, Guglielmo N, Copetti R. Lung ultrasound in diagnosing pneumonia in the emergency department: A systematic review and meta-analysis. Eur J Emerg Med. 2018;25:312–21.
Wong J, Montague S, Wallace P, Negishi K, Liteplo A, Ringrose J, Dversdal R, Buchanan B, Desy J, Ma IWY. Barriers to learning and using point-of-care ultrasound: a survey of practicing internists in six North American institutions. Ultrasound J. 2020;12:19.
Internal Clinical Guidelines Team U. Gallstone disease: diagnosis and management of cholelithiasis, cholecystitis and choledocholithiasis. Natl Inst Heal Care Excell 2014;1–102.
Kiewiet JJS, Leeuwenburgh MMN, Bipat S, Bossuyt PMM, Stoker J, Boermeester MA. A systematic review and meta-analysis of diagnostic performance of imaging in acute cholecystitis. Radiology. 2012;264:708–20.
Yarmenitis SD. Ultrasound of the gallbladder and the biliary tree. Eur Radiol. 2002;12:270–82.
Afonso L, Kottam A, Reddy V, Penumetcha A. Echocardiography in infective endocarditis: state of the art. Curr Cardiol Rep. 2017;19:127.
Bruun NE, Habib G, Thuny F, Sogaard P. Cardiac imaging in infectious endocarditis. Eur Heart J. 2014;35:624–32.
Hilberath JN, Oakes DA, Shernan SK, Bulwer BE, D’Ambra MN, Eltzschig HK. Safety of transesophageal echocardiography. J Am Soc Echocardiogr. 2010;23:1115–27.
Habets J, Tanis W, Reitsma JB, van den Brink RBA, Mali WPTM, Chamuleau SAJ, Budde RPJ. Are novel non-invasive imaging techniques needed in patients with suspected prosthetic heart valve endocarditis? A systematic review and meta-analysis. Eur Radiol. 2015;25:2125–33.
Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Heart J. 2015;36:3075–123.
Carrillo-Bayona JA, Arias-Alvarez L. Diagnostic imaging in sepsis of pulmonary origin. Sepsis, Third Ed 2017;51–65.
Prendki V, Scheffler M, Huttner B, et al. Low-dose computed tomography for the diagnosis of pneumonia in elderly patients: A prospective, interventional cohort study. Eur Respir J. 2018;51:1702375.
Garin N, Marti C, Scheffler M, Stirnemann J, Prendki V. Computed tomography scan contribution to the diagnosis of community-acquired pneumonia. Curr Opin Pulm Med. 2019;25:242–8.
Karhu JM, Ala-Kokko TI, Ahvenjärvi LK, Rauvala E, Ohtonen P, Syrjälä HPT. Early chest computed tomography in adult acute severe community-acquired pneumonia patients treated in the intensive care unit. Acta Anaesthesiol Scand. 2016;60:1102–10.
Bader FG, Schröder M, Kujath P, Muhl E, Bruchi HP, Eckmann C. Diffuse postoperative peritonitis - Value of diagnostic parameters and impact of early indication for relaparotomy. Eur J Med Res. 2009;14:491–6.
Velmahos GC, Kamel E, Berne TV, Yassa N, Ramicone E, Song Z, Demetriades D. Abdominal computed tomography for the diagnosis of intra-abdominal sepsis in critically injured patients: fishing in Murky waters. Arch Surg. 1999;134:831–8.
Connell TR, Stephens DH, Carlson HC, Brown ML. Upper abdominal abscess: a continuing and deadly problem. Am J Roentgenol. 1980;134:759–65.
Anbumani S, Soundarapandian A. A study of ultrasound and CT guided therapeutic drainage of intra-abdominal collections and abscesses. Int J Contemp Med Surg Radiol. 2018;3:3.
De Waele JJ. Rational use of antimicrobials in patients with severe acute pancreatitis. Semin Respir Crit Care Med. 2011;32:174–80.
Shao Y-H, Tsai K, Kim S, Wu Y-J, Demissie K, Shao Y-HJ. Exposure to tomographic scans and cancer risks. JNCI Cancer Spectr 2020;4:pkz072.
De Gonzalez AB, Salotti JA, McHugh K, et al. Relationship between paediatric CT scans and subsequent risk of leukaemia and brain tumours: assessment of the impact of underlying conditions. Br J Cancer. 2016;114:388–94.
Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505.
Preston DL, Pierce DA, Shimizu Y, Cullings HM, Fujita S, Funamoto S, Kodama K. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat Res. 2004;162:377–89.
Cardis E, Vrijheid M, Blettner M, et al. Risk of cancer after low doses of ionising radiation - Retrospective cohort study in 15 countries. Br Med J. 2005;331:77–80.
Goodman AL, Cook GJ, Goh V. Imaging in the investigation and management of Staphylococcus aureus bacteraemia: a role for advanced imaging techniques. J Hosp Infect. 2020;105:234–41.
NHS reference costs - GOV.UK. https://www.gov.uk/government/collections/nhs-reference-costs.
Operational Information for Commissioning NHS England. Diagnostic Imaging Dataset Annual Statistical Release 2017/18.
Alemanno G, Prosperi P, Di Bella A, et al. Bedside diagnostic laparoscopy for critically ill patients in the intensive care unit: retrospective study and review of literature. J Minim Access Surg. 2019;15:56–62.
Author information
Authors and Affiliations
Contributions
All authors contributed to the drafting and review of this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest or competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sepsis in the ICU
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duncan, C.F., Youngstein, T., Kirrane, M.D. et al. Diagnostic Challenges in Sepsis. Curr Infect Dis Rep 23, 22 (2021). https://doi.org/10.1007/s11908-021-00765-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s11908-021-00765-y