Abstract
Purpose of Review
To review the current literature on care of hypertension and chronic kidney disease for people who are currently and formerly incarcerated, and to make recommendations for improving outcomes.
Recent Findings
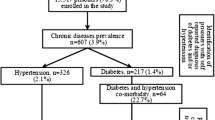
There is a growing body of literature describing care for kidney disease and hypertension for incarcerated and formerly incarcerated individuals that documents the provision of care itself, notably that many jails contract with private companies; the system is not designed to provide sustained, chronic disease care; and the transition from incarceration to community is fraught with gaps in care. However, deficiencies in data collection and regulation still limit our understanding of the quality of care provided in jails and prisons. Furthermore, more data is needed to understand the impact of structural racism in the criminal legal system on overall disparities in care for hypertension and kidney disease. Insurance coverage rates for people who were formerly incarcerated continue to be lower than the general population despite Medicaid expansion in many states. There is little recent data regarding kidney replacement therapy for this population despite known variation in dialysis modalities and transplant programs by state. Transitions clinics, which connect people who were formerly incarcerated with care in the community upon release, are growing and are important avenues by which to deliver care.
Summary
People who are incarcerated are disproportionately affected by hypertension and kidney disease, yet data regarding the extent of these inequities and availability of quality care is lacking. More work is needed to understand the care of individuals with kidney disease and hypertension in prisons and to improve outcomes for these common chronic conditions. Both providing effective treatment of kidney disease and hypertension in prisons and jails and providing coordinated, quality transition to community care upon release represents an important opportunity for reform in care for a marginalized population.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Rich Kluckow D, Zhen Zeng. Correctional populations in the United States, 2020 – statistical tables. Bureau of Justice Statistics. 2022.
Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389(10077):1464–74. https://doi.org/10.1016/s0140-6736(17)30259-3.
Lee H, Wildeman C, Wang EA, Matusko N, Jackson JS. A heavy burden: the cardiovascular health consequences of having a family member incarcerated. Am J Public Health. 2014;104(3):421–7. https://doi.org/10.2105/ajph.2013.301504.
Zeng Z. Jail inmates in 2021 – statistical tables. Bureau of Justice Statistics. 2022.
Services UDoHaH. United States Renal Data System 2022 Annual Data Report (ADR). 2022.
Chronic Kidney Disease in the United States, 2021. United States Department of Health and Human Services. 2021.
Kulkarni SP, Baldwin S, Lightstone AS, Gelberg L, Diamant AL. Is incarceration a contributor to health disparities? Access to care of formerly incarcerated adults. J Community Health. 2010;35(3):268–74. https://doi.org/10.1007/s10900-010-9234-9.
Skarupski KA, Gross A, Schrack JA, Deal JA, Eber GB. The health of America’s aging prison populatioN. Epidemiol Rev. 2018;40(1):157–65. https://doi.org/10.1093/epirev/mxx020.
Prost SG, Archuleta AJ, Golder S. Older adults incarcerated in state prison: health and quality of life disparities between age cohorts. Aging Ment Health. 2021;25(2):260–8. https://doi.org/10.1080/13607863.2019.1693976.
Prisons FBo. Inmate Age. 2023. https://www.bop.gov/about/statistics/statistics_inmate_age.jsp. Accessed 05/25/2023.
Centers for Disease Control and Prevention (CDC): Cigarette smoking among adults–United States, 2004. 2005.
Fazel S, Yoon IA, Hayes AJ. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction. 2017;112(10):1725–39. https://doi.org/10.1111/add.13877.
Bronson J, Stroop J, Zimmer S, Berzofsky M. Drug use, dependence, and abuse among state prisoners and jail inmates. U.S. Department of Justice Bureau of Justice Statistics. 2017;2007–2009.
Boulware LE, Mohottige D. The seen and the unseen: race and social inequities affecting kidney care. Clin J Am Soc Nephrol. 2021;16(5):815–7. https://doi.org/10.2215/cjn.12630820.
Wilper AP, Woolhandler S, Boyd JW, Lasser KE, McCormick D, Bor DH, et al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health. 2009;99(4):666–72. https://doi.org/10.2105/ajph.2008.144279.
Bondolfi C, Taffe P, Augsburger A, Jaques C, Malebranche M, Clair C, et al. Impact of incarceration on cardiovascular disease risk factors: a systematic review and meta-regression on weight and BMI change. BMJ Open. 2020;10(10): e039278. https://doi.org/10.1136/bmjopen-2020-039278.
Howell BA, Long JB, Edelman EJ, McGinnis KA, Rimland D, Fiellin DA, et al. Incarceration history and uncontrolled blood pressure in a multi-site cohort. J Gen Intern Med. 2016;31(12):1496–502. https://doi.org/10.1007/s11606-016-3857-1.
Wang EA, Pletcher M, Lin F, Vittinghoff E, Kertesz SG, Kiefe CI, et al. Incarceration, incident hypertension, and access to health care: findings from the coronary artery risk development in young adults (CARDIA) study. Arch Intern Med. 2009;169(7):687–93. https://doi.org/10.1001/archinternmed.2009.26.
• Coleman J, Lloyd-Jones DM, Ning H, Allen NB, Kiefe CI, Wang EA, et al. Association between incarceration and incident cardiovascular disease events: results from the CARDIA cohort study. BMC Public Health. 2021;21(1):214. https://doi.org/10.1186/s12889-021-10237-6. Excellent cohort study demonstrating that incidence of cardiovascular disease was higher in patients with history of incarceration, though the association was only significant in a subgroup of white men.
Massoglia M. Incarceration as exposure: the prison, infectious disease, and other stress-related illnesses. J Health Soc Behav. 2008;49(1):56–71. https://doi.org/10.1177/002214650804900105.
Williams BA, Li A, Ahalt C, Coxson P, Kahn JG, Bibbins-Domingo K. The cardiovascular health burdens of solitary confinement. J Gen Intern Med. 2019;34(10):1977–80. https://doi.org/10.1007/s11606-019-05103-6.
D’Atri DA, Fitzgerald EF, Kasl SV, Ostfeld AM. Crowding in prison: the relationship between changes in housing mode and blood pressure. Psychosom Med. 1981;43(2):95–105. https://doi.org/10.1097/00006842-198104000-00001.
Agyapong NAFAR, Apprey C. Prevalence of risk factors of cardiovascular diseases among prisoners: a systematic review. Nutr Food Sci. 2017;47:896–906.
Gebremariam MK, Nianogo RA, Arah OA. Weight gain during incarceration: systematic review and meta-analysis. Obes Rev. 2018;19(1):98–110. https://doi.org/10.1111/obr.12622.
Zatz ND. Get to work or go to jail: state violence and the racialized production of precarious work. Law Soc Inq. 2020;45(2):304–38. https://doi.org/10.1017/lsi.2019.56.
Bryan B. Housing instability following felony conviction and incarceration: disentangling being marked from being locked up. J Quant Criminol. 2022. https://doi.org/10.1007/s10940-022-09550-z.
Dong KR, Tang AM, Stopka TJ, Beckwith CG, Must A. Food acquisition methods and correlates of food insecurity in adults on probation in Rhode Island. PLoS ONE. 2018;13(6): e0198598. https://doi.org/10.1371/journal.pone.0198598.
Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30. https://doi.org/10.1196/annals.1441.030.
Thomas EH, Wang EA, Curry LA, Chen PG. Patients’ experiences managing cardiovascular disease and risk factors in prison. Health Justice. 2016;4:4. https://doi.org/10.1186/s40352-016-0035-9.
Curran J, Saloner B, Winkelman TNA, Alexander GC. Estimated use of prescription medications among individuals incarcerated in jails and state prisons in the US. JAMA Health Forum. 2023;4(4): e230482. https://doi.org/10.1001/jamahealthforum.2023.0482.
Hinata M, Ono M, Midorikawa S, Nakanishi K. Metabolic improvement of male prisoners with type 2 diabetes in Fukushima Prison. Japan Diabetes Res Clin Pract. 2007;77(2):327–32. https://doi.org/10.1016/j.diabres.2006.10.008.
Maruschak LM BM, Unangst J. Medical problems of state and federal prisoners and jail inmates. Bur Justice Stats. 2015;2011–12.
Bai JR, Befus M, Mukherjee DV, Lowy FD, Larson EL. Prevalence and predictors of chronic health conditions of inmates newly admitted to maximum security prisons. J Correct Health Care. 2015;21(3):255–64. https://doi.org/10.1177/1078345815587510.
Maruschak L, Chari KA, Simon AE, DeFrances CJ. National survey of prison health care: selected findings. Natl Health Stat Report. 2016;96:1–23.
Khairat S, Bohlmann A, Wallace E, Lakdawala A, Edson BS, Catlett TL, et al. Implementation and evaluation of a telemedicine program for specialty care in North Carolina correctional facilities. JAMA Netw Open. 2021;4(8): e2121102. https://doi.org/10.1001/jamanetworkopen.2021.21102.
• Murphy M, Ding A, Berk J, Rich J, Bayliss G. Kidney disease among people who are incarcerated. Clin J Am Soc Nephrol. 2021;16(11):1766–72. https://doi.org/10.2215/cjn.01910221. Excellent review of kidney disease among incarcerated individuals, highlighting how Black and Latinx patients are disproportionately affected by both. Also recommends steps for improving care including implementing health screening upon entry into jail, expanding lab access, and linking people who are recently released from prison to primary care.
Robinson C. On-site dialysis for prisoners with end-stage kidney disease. Nursing Times [online]. 2018.
Sankaranarayanan N, Agrawal R, Guinipero L, Kaplan AA, Adams ND. Self-performed peritoneal dialysis in prisoners. Adv Perit Dial. 2004;20:98–100.
Gowda M, Gundroo A, Lamphron B, Gupta G, Visger JV, Kataria A. Kidney transplant program for prisoners: rewards, challenges, and perspectives. Transplantation. 2020;104(10):1967–9. https://doi.org/10.1097/tp.0000000000003197.
Ahmad MU, Eves MM. The structural conundrum of parolees and kidney transplantation. Clin Transplant. 2020;34(12): e14104. https://doi.org/10.1111/ctr.14104.
Panesar M, Bhutani H, Blizniak N, Gundroo A, Zachariah M, Pelley W, et al. Evaluation of a renal transplant program for incarcerated ESRD patients. J Correct Health Care. 2014;20(3):220–7. https://doi.org/10.1177/1078345814531726.
Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison–a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–65. https://doi.org/10.1056/NEJMsa064115.
Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. https://doi.org/10.7326/0003-4819-159-9-201311050-00005.
Alex B, Weiss DB, Kaba F, Rosner Z, Lee D, Lim S, et al. Death after jail release. J Correct Health Care. 2017;23(1):83–7. https://doi.org/10.1177/1078345816685311.
Jones M, Kearney GD, Xu X, Norwood T, Proescholdbell SK. Mortality rates and cause of death among former prison inmates in North Carolina. N C Med J. 2017;78(4):223–9. https://doi.org/10.18043/ncm.78.4.223.
Fox AD, Anderson MR, Bartlett G, Valverde J, Starrels JL, Cunningham CO. Health outcomes and retention in care following release from prison for patients of an urban post-incarceration transitions clinic. J Health Care Poor Underserved. 2014;25(3):1139–52. https://doi.org/10.1353/hpu.2014.0139.
Wang EA, Wang Y, Krumholz HM. A high risk of hospitalization following release from correctional facilities in Medicare beneficiaries: a retrospective matched cohort study, 2002 to 2010. JAMA Intern Med. 2013;173(17):1621–8. https://doi.org/10.1001/jamainternmed.2013.9008.
Fahmy N, Kouyoumdjian FG, Berkowitz J, Fahmy S, Neves CM, Hwang SW, et al. Access to primary care for persons recently released from prison. Ann Fam Med. 2018;16(6):549–51. https://doi.org/10.1370/afm.2314.
Frank JW, Wang EA, Nunez-Smith M, Lee H, Comfort M. Discrimination based on criminal record and healthcare utilization among men recently released from prison: a descriptive study. Health Justice. 2014;2:6. https://doi.org/10.1186/2194-7899-2-6.
Binswanger IA, Nowels C, Corsi KF, Long J, Booth RE, Kutner J, et al. “From the prison door right to the sidewalk, everything went downhill,” a qualitative study of the health experiences of recently released inmates. Int J Law Psychiatry. 2011;34(4):249–55. https://doi.org/10.1016/j.ijlp.2011.07.002.
Patel K, Boutwell A, Brockmann BW, Rich JD. Integrating correctional and community health care for formerly incarcerated people who are eligible for Medicaid. Health Aff (Millwood). 2014;33(3):468–73. https://doi.org/10.1377/hlthaff.2013.1164.
Knapp CD, Howell BA, Wang EA, Shlafer RJ, Hardeman RR, Winkelman TNA. Health insurance gains after implementation of the affordable care act among individuals recently on probation: USA, 2008–2016. J Gen Intern Med. 2019;34(7):1086–8. https://doi.org/10.1007/s11606-019-04900-3.
Winkelman TN, Kieffer EC, Goold SD, Morenoff JD, Cross K, Ayanian JZ. Health insurance trends and access to behavioral healthcare among justice-involved individuals-United States, 2008–2014. J Gen Intern Med. 2016;31(12):1523–9. https://doi.org/10.1007/s11606-016-3845-5.
Commodore-Mensah Y, Foti K, Dennison HC. Equity in hypertension care and outcomes: closing the black-white gap in blood pressure control. Am J Hypertens. 2022;35(6):500–2. https://doi.org/10.1093/ajh/hpac002.
Colvin CL, Kalejaiye A, Ogedegbe G, Commodore-Mensah Y. Advancing equity in blood pressure control: a response to the surgeon general’s call-to-action. Am J Hypertens. 2022;35(3):217–24. https://doi.org/10.1093/ajh/hpab187.
Ogunniyi MO, Commodore-Mensah Y, Ferdinand KC. Race, ethnicity, hypertension, and heart disease: JACC Focus Seminar 1/9. J Am Coll Cardiol. 2021;78(24):2460–70. https://doi.org/10.1016/j.jacc.2021.06.017.
Doyle SK, Chang AM, Levy P, Rising KL. Achieving health equity in hypertension management through addressing the social determinants of health. Curr Hypertens Rep. 2019;21(8):58. https://doi.org/10.1007/s11906-019-0962-7.
• Powell-Wiley TM, Baumer Y, Baah FO, Baez AS, Farmer N, Mahlobo CT, et al. Social determinants of cardiovascular disease. Circ Res. 2022;130(5):782–99. https://doi.org/10.1161/circresaha.121.319811. Recent review that provides a helpful framework for the effects of structural racism on cardiovascular disease, but has very limited discussion of incarceration — noting only one 2014 study that includes judicial treatment at the state level as part of a measure of structural racism. This thorough review exemplifies the dearth of incarceration data impacting CVD outcomes.
Hayes DK, Jackson SL, Li Y, Wozniak G, Tsipas S, Hong Y, et al. Blood pressure control among non-Hispanic black adults is lower than non-Hispanic white adults despite similar treatment with antihypertensive medication: NHANES 2013–2018. Am J Hypertens. 2022;35(6):514–25. https://doi.org/10.1093/ajh/hpac011.
Alves da Costa F, Verschuuren M, Andersen Y, Stürup-Toft S, Lopez-Acuña D, Ferreira-Borges C. The WHO Prison Health Framework: a framework for assessment of prison health system performance. Eur J Public Health. 2022;32(4):565–70. doi:https://doi.org/10.1093/eurpub/ckac020.
• Wennerstrom A, Sugarman M, Martin D, Lobre CB, Haywood CG, Niyogi A. 'You have to be almost dead before they ever really work on you in prison': a qualitative study of formerly incarcerated women's health care experiences during incarceration in Louisiana, U.S. Health Soc Care Community. 2022;30(5):1763–74. https://doi.org/10.1111/hsc.13556. Qualitative study of 22 formerly incarcerated women in a Louisiana prison who describe severe health care deficiencies including lack of timely care, high cost, punishment for seeking care and more.
• Howell BA, Puglisi LB, Aminawung J, Domingo KB, Elumn J, Gallagher C, et al. A prospective cohort study examining exposure to incarceration and cardiovascular disease (Justice-Involved Individuals Cardiovascular Disease Epidemiology - JUSTICE study): a protocol paper. BMC Public Health. 2022;22(1):331. https://doi.org/10.1186/s12889-022-12688-x. Little prospective data currently exist that examine the impact of incarceration, and this is an exciting ongoing study that will examine risk factors for cardiovascular disease among formerly incarcerated individuals.
Estelle v. Gamble, 429 U.S. 97 (1976). https://supreme.justia.com/cases/federal/us/429/97/. Accessed 05/25/2023.
Assembly UNG. United Nations Standard Minimum Rules for the Treatment of Prisoners, G.A. Res. 70/175. 2016.
• Carda-Auten J, Dirosa EA, Grodensky C, Nowotny KM, Brinkley-Rubinstein L, Travers D, et al. Jail health care in the southeastern United States from entry to release. Milbank Q. 2022;100(3):722–60. https://doi.org/10.1111/1468-0009.12569. This qualitative study of 34 jails in five southeastern states demonstrated that 90% of jails contracted with private health companies, and it was common for detention officers to participate in medical care and uncommon for jails to participate in transitional services for health care.
Isaacs C. Treatment industrial complex: Prison Policy Initiative2014.
Klein DE, Lima JM. The prison industrial complex as a commercial determinant of health. Am J Public Health. 2021;111(10):1750–2. https://doi.org/10.2105/ajph.2021.306467.
Scott D. A worrisome trend in American hospitals is hurting poor patients. Vox. 2023. https://www.vox.com/policy-and-politics/2023/1/13/23550067/us-hospitals-medicaid-patients-health-care-access. Accessed 05/28/2023 2023.
Singh Y, Song Z, Polsky D, Bruch JD, Zhu JM. Association of private equity acquisition of physician practices with changes in health care spending and utilization. JAMA Health Forum. 2022;3(9):e222886-e. https://doi.org/10.1001/jamahealthforum.2022.2886.
Deitch M. But who oversees the overseers?: the status of prison and jail oversight in the United States. Am J Criminal Law. 2020;47.
Saloner B, Eber GB, Sufrin CB, Beyrer C, Rubenstein LS. A human rights framework for advancing the standard of medical care for incarcerated people in the United States in the time of COVID-19. Health Hum Rights. 2022;24(1):59–75.
Karandinos G, Bourgois P. The structural violence of hyperincarceration - a 44-year-old man with back pain. N Engl J Med. 2019;380(3):205–9. https://doi.org/10.1056/NEJMp1811542.
Transitions Clinic Network. 2014. https://transitionsclinic.org/transitions-clinic-network/. Accessed 05/25/2023.
Shavit S, Aminawung JA, Birnbaum N, Greenberg S, Berthold T, Fishman A, et al. Transitions clinic network: challenges and lessons in primary care for people released from prison. Health Aff (Millwood). 2017;36(6):1006–15. https://doi.org/10.1377/hlthaff.2017.0089.
Fox AD, Anderson MR, Bartlett G, Valverde J, MacDonald RF, Shapiro LI, et al. A description of an urban transitions clinic serving formerly incarcerated people. J Health Care Poor Underserved. 2014;25(1):376–82. https://doi.org/10.1353/hpu.2014.0039.
Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102(9):e22–9. https://doi.org/10.2105/ajph.2012.300894.
Dong KR, Beckwith CG, Grossman A, Weiner DE, Lichtenstein AH. Utilizing the probation office as an opportunity to screen for cardiometabolic outcomes: a feasibility study. J Correct Health Care. 2022;28(4):274–82. https://doi.org/10.1089/jchc.20.11.0102.
• Barnert ES, Scannell C, Ashtari N, Albertson E. Policy solutions to end gaps in Medicaid coverage during reentry after incarceration in the United States: experts’ recommendations. Z Gesundh Wiss. 2022;30(9):2201–9. https://doi.org/10.1007/s10389-021-01483-4. This 2022 paper highlights the effects of Medicaid coverage gaps for formerly incarcerated individuals and describes practical policy changes to fill these gaps.
Foundation KF. Status of state medicaid expansion decisions: interactive map. 2023. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/.
• Howell BA, Hawks L, Wang EA, Winkelman TNA. Evaluation of changes in US health insurance coverage for individuals with criminal legal involvement in Medicaid expansion and nonexpansion states, 2010 to 2017. JAMA Health Forum. 2022;3(4): e220493. https://doi.org/10.1001/jamahealthforum.2022.0493. 2022 study demonstrating that Medicaid expansion in states that have not adopted ACA policies would disproportionately affect formerly incarcerated persons and improve coverage for chronic conditions.
Albertson EM, Scannell C, Ashtari N, Barnert E. Eliminating gaps in medicaid coverage during reentry after incarceration. Am J Public Health. 2020;110(3):317–21. https://doi.org/10.2105/ajph.2019.305400.
Winkelman TN, Choi H, Davis MM. The Affordable Care Act, insurance coverage, and health care utilization of previously incarcerated young men: 2008–2015. Am J Public Health. 2017;107(5):807–11. https://doi.org/10.2105/ajph.2017.303703.
• Burns ME, Cook ST, Brown L, Tyska S, Westergaard RP. Increasing Medicaid enrollment among formerly incarcerated adults. Health Serv Res. 2021;56(4):643–54. https://doi.org/10.1111/1475-6773.13634. Recent study demonstrating that Medicaid eligibility expansion and assistance with Medicaid enrollment during the month prior to release increased Medicaid coverage from 8 to 36% in this study in Wisconsin state prisons.
• Burns ME, Cook S, Brown LM, Dague L, Tyska S, Hernandez Romero K, et al. Association between assistance with Medicaid enrollment and use of health care after incarceration among adults with a history of substance use. JAMA Netw Open. 2022;5(1): e2142688. https://doi.org/10.1001/jamanetworkopen.2021.42688. A retrospective cohort study of 16,307 adults with substance use disorders released from state prison that showed assistance with Medicaid enrollment prior to release from prison is associated with increased utilization of outpatient health services among formerly incarcerated individuals with substance use disorders.
Patel K, Herdman B, Brown K. Preventing interruptions in health care after release from jail. J Correct Health Care. 2022;28(4):215–9. https://doi.org/10.1089/jchc.20.12.0119.
Funding
Dr. Rizzolo was funded by National Institutes of Health grant 5T32DK007135-46 during the drafting of this manuscript. The remaining authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rockey, N., Cervantes, L., LeMasters, K. et al. Challenging Health Inequities in Incarceration: a Call for Equitable Care for Kidney Disease and Hypertension. Curr Hypertens Rep 25, 437–445 (2023). https://doi.org/10.1007/s11906-023-01267-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11906-023-01267-z