Abstract
Purpose of Review
The coronavirus disease 2019 (COVID-19) pandemic has popularized the usage of hydroxychloroquine and chloroquine (HCQ/CQ) as treatments for COVID-19. Previously used as anti-malarial and now commonly used in rheumatologic conditions, preliminary in vitro studies have demonstrated these medications also have anti-viral properties. Retinopathy and neuromyopathy are well recognized complications of using these treatments; however, cardiotoxicity is under-recognized. This review will discuss the implications and cardiotoxicity of HCQ/CQ, their mechanisms of action, and their utility in COVID-19.
Recent Findings
Early clinical trials demonstrated a modest benefit of HCQ in COVID-19, causing a push for the usage of it. However, further large multi-center randomized control centers, demonstrated no benefit, and even a trend towards worse outcomes. The predominant cardiac complication observed with HCQ in COVID-19 was cardiac arrhythmias and prolonging of the QT interval. However, with chronic usage of HCQ/CQ, the development of heart failure (HF) and cardiomyopathy (CM) can occur.
Summary
Although, most adverse cardiac events related to HCQ/CQ usage in COVID-19 were secondary to conduction disorders given the short duration of treatment, HCQ/CQ can cause CM and HF, with chronic usage. Given the insufficient evidence, HCQ/CQ usage in COVID-19 is not routinely recommended, especially with novel therapies now being developed and used. Additionally, usage of HCQ/CQ should prompt initial cardiac evaluation with ECG, and yearly monitoring, with consideration for advanced imaging if clinically warranted. The diagnosis of HCQ/CQ cardiomyopathy is important, as prompt cessation can allow for recovery when these changes are still reversible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronavirus disease 2019 (COVID-19) propagated throughout the world in late 2019 causing a worldwide pandemic, placing a significant burden on healthcare systems. This prompted evaluation for effective medical treatments for COVID-19. Hydroxychloroquine and chloroquine (HCQ/CQ) have known anti-inflammatory effects such as suppressing tumor necrosis factor alpha (TNF-α), interleukin 1 (IL-1) and interleukin 6 (IL-6) which mediate inflammatory complications of several viral diseases [1]. Given these theoretical effects, HCQ/CQ were popularized by the media and politicians as a possible treatment for COVID-19 in early 2020. The FDA approved HCQ/CQ for emergency usage in March 2020, even prior to the first blinded, randomized controlled trial which was published on March-31, 2020 [2]. This caused prescriptions for HCQ/CQ to drastically increase despite any concrete evidence for the use [3]. The FDA later revoked the emergency usage and authorization in June 2020, citing the lack of efficacy [4].
HCQ/CQ are common anti-malarial agents [5] and are also medications used for rheumatologic conditions such as rheumatoid arthritis (RA) [6] and systemic lupus erythematous (SLE) [7]. Although cardiac complications secondary to drugs of abuse [8] and oncologic medications [9] are well documented, cardiac complications secondary to HCQ/CQ are not as well described [10]. This review will discuss the implications and cardiotoxicity of HCQ/CQ and briefly their mechanisms of action and their utility in COVID-19.
Mechanisms of Action
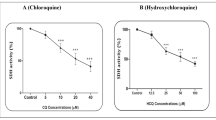
The overall mechanisms of action of HCQ/CQ are quite complex and likely not fully understood [11]. HCQ/CQ belong to a class of medications known as 4-aminoquinolones [5]. HCQ/CQ are well absorbed when given orally and have prolonged half-lives of greater than 40 days [12]. HCQ and CQ are very similar chiral molecules, with similar efficacy for treatment of malaria, but HCQ is much less toxic with fewer adverse effects [13]. An important mechanism of action of HCQ/CQ is through accumulation in lysosomes and autophagosomes of phagocytic cells, changing local cellular pH concentrations [5]. In malaria, this interferes with the asexual reproduction of the parasite, in addition to interfering with parasite growth [14]. HCQ/CQ increase the pH in lysosomes of antigen-presenting cells and inhibit Toll-like receptors function on dendritic cells, which reduce the activation of these cells and in turn inhibit the production of inflammatory cytokines [14].
Since HCQ/CQ can impair the replication of viruses through interacting with the late stages of replication of enveloped viruses and with the endosome-mediated viral entry in addition to the anti-inflammatory properties [1], it seems plausible that there could be utility in the management of viral illnesses such as COVID-19. Indeed, in translational models of severe acute respiratory syndrome, HCQ/CQ inhibits angiotensin-converting enzyme 2 (ACE2) glycosylation attenuating the virus pre- and post-infection [15].
Adverse Effects
The adverse effects of oral HCQ/CQ are becoming better understood and reported, with retinopathy, neuromyopathy, and skin hyperpigmentation being well documented, and with cardiomyopathy and conduction disorders coming to the forefront in recent literature [10, 16] (Fig. 1). Typically, the risk of cardiotoxicity is dose and time dependent, usually taking years to develop [17]. Some risk factors associated with increased adverse effects are female sex, older age, and renal dysfunction [17].
Cardiomyopathy
HCQ/CQ have inhibitory effects in the lysosomes secondary to changing their local pH concentrations causing pathological accumulation of metabolic products such as glycogen and phospholipids which are a known cause of cardiomyopathy [5, 16, 18]. This results in the appearance of myeloid bodies and curvilinear bodies in cytoplasm when viewed under electron microscopy following endomyocardial biopsy [19]. Similar changes are also seen in other lysosomal storage disorders, such as Fabry disease (FD), and can result in health practitioners incorrectly diagnosing HCQ-induced cardiotoxicity as FD [16, 20•, 21–23]. Importantly, curvilinear bodies are not seen in FD and can serve as a distinguishing characteristic [16, 24]. Accumulation of these curvilinear bodies subsequently can lead to disruption of myofibrillar organization and subsequent cardiac myocyte hypertrophy and myocardial fibrosis. Ultimately, HCQ-induced cardiotoxicity is a phenocopy of FD as both conditions result in a cardiomyopathy secondary to an infiltrative process characterized by concentric hypertrophy with associated conduction abnormalities that can lead to heart failure [16]. The features of cardiomyopathy secondary to HCQ/CQ are not well documented, but thought to be ventricular hypertrophy, hypokinesia, valvular dysfunction, and even pulmonary arterial hypertension [25•] (Table 1).
Cardiac MRI is helpful in the diagnoses of Fabry’s disease, as T1 mapping is highly sensitive and specific for the diagnosis and can also be used for HCQ/CQ induced cardiomyopathy [26]. Endomyocardial biopsy may be needed to identify the curvilinear bodies present in HCQ/CQ induced cardiomyopathy; however, clinical history or genetic testing may be able to make this distinction non-invasively [16, 24]. Diagnosis is important since if HCQ/CQ is withdrawn quickly enough, there does seem to be some reversal and recovery possible [20•].
Electrophysiological Effects of Hydroxychloroquine on the Heart
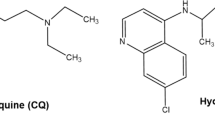
Quinolone anti-malarial medications and other structurally related compounds have been long known to cause cardiovascular side effects including hypotension and electrocardiographic QT interval prolongation [27]. HCQ/CQ can act as Vaughan-William Class-Ia anti-arrhythmic, similar to quinidine, and as such they have been implicated with conduction disorders, bradycardia, tachycardia, T-wave flattening, and QT interval prolongation [28]. The COVID-19 pandemic brought this into further focus as the potential for cardiotoxicity through QT prolongation was a critical consideration during clinical trials [29,30,31]. This potential cardiotoxicity should be interpreted in the context that patients with COVID-19 may have a predisposition to developing arrhythmias ranging from sinus tachycardia, sinus bradycardia, and asystole secondary to the inflammatory process from COVID-19 (Fig. 2A) [29, 30, 32]. Specifically, myocarditis is an important manifestation of COVID-19 disease that is pro-arrhythmogenic and the administration of QT prolonging medications may further exacerbate this underlying arrhythmia burden [30]. Additionally, many of these patients with severe COVID-19 may also have biochemical changes including hypokalemia, hypomagnesemia, and fever which can further enhance QT prolongation [10].
QT prolongation in patients with COVID-19 treated with hydroxychloroquine. Predisposing risk factors to QT prolongation in patients with COVID-19 (A). Electrophysiological mechanism of action of QT prolongation with hydroxychloroquine treatment (B). HCQ inhibition of the potassium rectifier current (Ikr) through inhibition of the human ether-a-go-go-related gene (hERG) channel leads to increased action potential duration and subsequent QT prolongation. QT prolongation may ultimately lead to Torsades de Pointes. HCQ indicates hydroxychloroquine; hERG, human ether-a-go-go-related gene; AP, action potential. Figure created in Biorender
QT Interval Prolongation
Perhaps the best understood electrophysiological effect of HCQ/CQ is QT prolongation, which occurs through blockade of the delayed rectifier potassium current (Ikr) involved in phase 3 of the cardiac myocyte action potential (Fig. 2B) [30, 31, 33, 34]. HCQ inhibits the Ikr by human ether-a-go-go-related gene (hERG) channel blockade, which results in increased action potential duration, followed by early after-depolarizations due to calcium depolarizing currents, and triggered premature ventricular complexes. Ultimately, these changes can lead to QT prolongation which may evolve into a polymorphic ventricular tachycardia, specifically Torsades de Pointes (TdP) [35]. When used in rheumatological conditions, the rate of QTc prolongation is relatively low [36,37,38].
When HCQ is used in patients with COVID-19, QT interval prolongation was a commonly noted adverse effect [34, 39, 40]. This risk was further exacerbated by the concurrent use of macrolides, such as azithromycin, which are another commonly used drug class implicated in QT prolongation through hERG blockade [40,41,42]. Use of HCQ/CQ and azithromycin concurrently may have an augmentation effect on QT interval prolongation which can lead to ventricular arrhythmias, discontinuation of therapy, and rarely episodes of TdP [30, 34, 40]. Overall, to mitigate the arrhythmia risk while using HCQ/CQ in COVID-19 patients, or other critical illness; baseline electrocardiograms (ECGs) should be completed as these illnesses can induce systemic inflammatory cascades and electrolyte imbalances that may predispose patients to these fatal cardiac arrythmias [30, 43, 44].
Other Arrhythmic Effects
There are some other less well-defined effects of HCQ on cardiac rhythm, including bradycardia and conduction blocks. There are some case reports that have demonstrated that HCQ may induce sinus bradycardia, including during the COVID-19 pandemic [45, 46]. Early translational work has proposed that HCQ may act as a bradycardic agent by reducing the spontaneous action potential (AP) firing rate in sinoatrial node myocytes [47]. This reduction in AP firing rate may be due to modulation and reduction of through inhibitory modulation of the If, Ikf, and ICaL currents. There is also evidence that HCQ usage may be associated with the development of conductive heart disorders, such as right bundle branch block, left anterior fascicular block, and complete atrioventricular (AV) block [18, 48]. It was noted that these conductive disorders may precede heart failure symptoms and typically progress gradually from right bundle branch block, first- or second-degree AV block to complete AV blocks [18]. Amongst these patients, it is possible that as they get older, they may already be predisposed to increased risk of developing cardiac arrhythmias, and particular attention should be given to this population before initiating therapies [49]. The risk of bradycardia and heart block may be another indication that baseline electrocardiogram and follow-up electrocardiogram be performed as a screening tool for early conductive disease when patients are initiated on HCQ therapy.
It was initially proposed that HCQ may be used in the treatment of atrial fibrillation [50], as similarly quinidine, an anti-malarial agent that is also a Vaughan-William Class-1a anti-arrhythmic was once commonly used as an anti-fibrillatory agent [51]. Interestingly, there is some clinical evidence that supports this notion as there is a reduced incidence of atrial fibrillation in SLE patients being treated with hydroxychloroquine [52]. Additionally, despite the pro-arrhythmic effects discussed previously, there are studies showing that use of HCQ did not significantly increase arrhythmia risk or life-threating arrythmia risk amongst these patients [53]. Further work is likely required to assess the potential utility of HCQ as an anti-arrhythmic agent, and there is one clinical trial (NCT03592823) in progress to assess the potential for HCQ to reduce atrial fibrillation recurrence in patients who have undergone radiofrequency catheter ablations.
Other Adverse Systemic Effects of HCQ Therapy
In addition to these cardiac effects, HCQ is well documented to cause ocular toxicity, skin hyperpigmentation, and neuromuscular weakness (Fig. 1). Ocular toxicity primarily occurs in the form of retinal damage with reports that up to 1 in 20 patients may develop retinopathy after 5 years of HCQ usage [54, 55]. Patients may have lower risk of developing retinopathy if their daily dose is less than 5 mg/kg [56]. Skin hyperpigmentation is a common dermatological adverse effect associated with HCQ use [57], and this hyperpigmentation may be secondary to ecchymosis or bruising and more common in patients with pre-disposing risk factors to bruising easily [58]. There are estimates that 10–25% of patients with systemic lupus erythematosus will develop skin hyperpigmentation while taking HCQ [59]. Finally, HCQ can also lead to myopathy through lysosomal dysfunction leading to formation of curvilinear bodies, which can damage muscle cells [60, 61]. The incidence of HCQ-related myopathy may be approximately 2.5% [62]. From a side effect profile, HCQ use can also commonly lead to gastrointestinal symptoms, primarily nausea, diarrhea, abdominal pain, and vomiting [63, 64].
Summary of Research
In 2020, multiple clinical trials were started to assess the efficacy of HCQ/CQ in COVID-19 (Table 2). Initial results seemed promising when the first RCT by Chen et al. demonstrated an improvement in clinical status and resolution of pneumonia [2] and soon after Gautret et al. demonstrated substantial increase in viral clearance [65]. Additionally, the FDA approved HCQ/CQ for emergency usage for COVID-19 in March 2020 [4]. These early results and approval prompted multiple further trials, but with lack of documentation of efficacy and ongoing adverse events, the FDA revoked its emergency status and authorization shortly after in June 2020 [4]. Despite the randomized controlled trials (RCTs) in 2020, there was still very limited documented evidence of benefit (Table 2). Two substantial studies were the RECOVERY trial and the WHO Consortium Solidarity trials published in late 2020, which included adult hospitalized patients with confirmed COVID-19 (The RECOVERY trial also included suspected COVID-19 patients) [66•, 67•]. These were the first RCTs with thousands of patients, and they both demonstrated no significant differences in outcomes and were stopped early [66•, 67•]. In the RECOVERY trial, the average age was 65.4, with 57% having at least one major coexisting illness, and 27% of patients having diabetes [66•]. At randomization, 17% of these patients were receiving invasive mechanical ventilation [66•]. In this trial, patients had a slightly greater risk of death from cardiac causes (0.4%, 0.2–0.6); however, no significant difference between the development of supraventricular tachycardia (SVT), ventricular tachycardia (VT), ventricular fibrillation (VF), or atrioventricular block requiring intervention [66•]. There was one report of a patient developing TdP related to HCQ [66•]. In the WHO Consortium Solidarity trial, 81% of patients were under the age of 70 years, and 25% of patients had diabetes [67•]. At randomization, 8% were receiving invasive mechanical ventilation [67•]. In this trial, cardiac deaths were too few to reliably come to any conclusions [67•].
A systematic review published in April 2021 concluded that the combined odds ratio (OR) of all-cause mortality for the use of HCQ in COVID-19 was 1.11 (95% CI 1.02–1.20) [68]. A systematic review from 2022 additionally found that cardiac adverse events were frequent (0–27.3% and up to 33% if concurrent usage of azithromycin) [69]. Given this overwhelming lack of evidence (despite some of the initial trials) (Table 2), the interest and usage of HCQ/CQ seem to be declining. This is likely in part as the initial trials had very small sample sizes, potential for bias, and did not assess meaningful outcomes.
Usage in COVID-19 and Recommendations
Since the FDA revoked its emergency status and authorization [4], and there are two large RCTs demonstrating lack of utility of HCQ in COVID-19, [66•, 67•], its usage is not recommended for the treatment of COVID-19. Multiple subsequent large systematic reviews support this recommendation [68, 69]. Although, there may be utility for further studies in outpatient COVID-19, or specific sub-groups, at this time, the literature is limited. Notwithstanding the lack of efficacy, if HCQ/CQ is used (off-label) in the management of COVID-19, baseline electrocardiograms (ECGs) should be considered [30, 43, 44]. Although the enormous burden placed upon healthcare systems by the COVID-19 pandemic has led to desperation for efficacious treatment options, we highlight that the use of treatments with limited evidence can result in more harm than benefit.
Conclusions
HCQ/CQ have well documented adverse events, with cardiotoxicity becoming increasingly recognized. Although most adverse cardiac events related to HCQ/CQ usage in COVID-19 were secondary to conduction disorders given the short duration of treatment, it should be noted that HCQ/CQ can cause CM and HF, especially with chronic usage. Given the insufficient evidence to support its usage and lack of FDA approval in COVID-19, HCQ/CQ is not routinely recommended for COVID-19, especially with novel therapies now being developed [4, 68, 70]. Given the concurrent inflammation and critical illness associated with infections such as COVID-19, cardiotoxicity, especially conduction disorders secondary to HCQ/CQ usage can be exacerbated. In chronic usage, such as in rheumatologic conditions, yearly ECGs should be completed with consideration for further advanced imaging if clinical suspicion for HCQ/CQ cardiomyopathy exists. Early recognition and diagnosis of HCQ/CQ cardiomyopathy are important as cessation may lead to reversal and recovery [20•].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Savarino A, Boelaert JR, Cassone A, Majori G, Cauda R. Effects of chloroquine on viral infections: an old drug against today’s diseases? Lancet Infect Dis. 2003;3(11):722–7.
Chen Z, Hu J, Zhang Z, Jiang S, Han S, Yan D, et al. Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial. medRxiv. 2020;2020.03.22.20040758.
Vaduganathan M, van Meijgaard J, Mehra MR, Joseph J, O’Donnell CJ, Warraich HJ. Prescription fill patterns for commonly used drugs during the COVID-19 pandemic in the United States. JAMA. 2020;323(24):2524–6.
Lovelace Jr. B. FDA revokes emergency use authorization for chloroquine and hydroxychloroquine. 2020. https://www.cnbc.com/2020/06/15/fda-revokes-emergency-use-of-hydroxychloroquine.html. Accessed 15 June 2020
Schrezenmeier E, Dörner T. Mechanisms of action of hydroxychloroquine and chloroquine: implications for rheumatology. Nat Rev Rheumatol. 2020;16(3):155–66.
Fraenkel L, Bathon JM, England BR, St Clair EW, Arayssi T, Carandang K, et al. American College of Rheumatology Guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2021;73(7):924–39.
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN, et al. 2019 Update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis. 2019;78(6):736–45.
Gagnon LR, Sadasivan C, Perera K, Oudit GY. Cardiac complications of common drugs of abuse: pharmacology, toxicology, and management. Can J Cardiol. 2022;38:1331–41
Sadasivan C, Zhabyeyev P, Labib D, White JA, Paterson DI, Oudit GY. Cardiovascular toxicity of PI3Kα inhibitors. Clin Sci (Lond). 2020;134(19):2595–622.
Oren O, Yang EH, Gluckman TJ, Michos ED, Blumenthal RS, Gersh BJ. Use of chloroquine and hydroxychloroquine in COVID-19 and cardiovascular implications: understanding safety discrepancies to improve interpretation and design of clinical trials. Circ Arrhythm Electrophysiol. 2020;13(6):e008688.
Fox RI. Mechanism of action of hydroxychloroquine as an antirheumatic drug. Semin Arthritis Rheum. 1993;23(2 Suppl 1):82–91.
Furst DE. Pharmacokinetics of hydroxychloroquine and chloroquine during treatment of rheumatic diseases. Lupus. 1996;5(Suppl 1):S11–5.
Warhurst DC, Steele JC, Adagu IS, Craig JC, Cullander C. Hydroxychloroquine is much less active than chloroquine against chloroquine-resistant Plasmodium falciparum, in agreement with its physicochemical properties. J Antimicrob Chemother. 2003;52(2):188–93.
Stokkermans TJ, Goyal A, Trichonas G. Chloroquine and hydroxychloroquine toxicity. Treasure Island: StatPearls; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537086/
Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, Ksiazek TG, et al. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. 2005;2:69.
Yogasundaram H, Putko BN, Tien J, Paterson DI, Cujec B, Ringrose J, et al. Hydroxychloroquine-induced cardiomyopathy: case report, pathophysiology, diagnosis, and treatment. Can J Cardiol. 2014;30(12):1706–15.
Nadeem U, Raafey M, Kim G, Treger J, Pytel P, N Husain A, et al. Chloroquine and hydroxychloroquine–induced cardiomyopathy: a case report and brief literature review. Am J Clin Pathol. 2021;155(6):793–801.
Tönnesmann E, Kandolf R, Lewalter T. Chloroquine cardiomyopathy – a review of the literature. Immunopharmacol Immunotoxicol. 2013;35(3):434–42.
Joyce E, Fabre A, Mahon N. Hydroxychloroquine cardiotoxicity presenting as a rapidly evolving biventricular cardiomyopathy: key diagnostic features and literature review. Eur Heart J Acute Cardiovasc Care. 2012;2(1):77–83.
Yogasundaram H, Hung W, Paterson ID, Sergi C, Oudit GY. Chloroquine-induced cardiomyopathy: a reversible cause of heart failure. ESC Heart Failure. 2018;5(3):372–5. These authors report that chloroquine-induced cardiomyopathy is reversible. It is suggested that early cessation of chloroquine prevents further damage.
Sadasivan C, Chow JTY, Sheng B, Chan DKH, Fan Y, Choi PCL, et al. Screening for Fabry disease in patients with unexplained left ventricular hypertrophy. PLoS ONE. 2020;15(9):e0239675.
Wu S-Z, Liang X, Geng J, Zhang M-B, Xie N, Su X-Y. Hydroxychloroquine-induced renal phospholipidosis resembling Fabry disease in undifferentiated connective tissue disease: a case report. World J Clin Cases. 2019;7(24):4377–83.
Serre J, Buob D, Boffa J-J. Hydroxychloroquine-induced podocytopathy mimicking Fabry disease. BMJ Case Reports. 2019;12(5):e228876.
Roos JM, Aubry M-C, Edwards WD. Chloroquine cardiotoxicity: clinicopathologic features in three patients and comparison with three patients with Fabry disease. Cardiovasc Pathol. 2002;11(5):277–83.
Chatre C, Roubille F, Vernhet H, Jorgensen C, Pers YM. Cardiac complications attributed to chloroquine and hydroxychloroquine: a systematic review of the literature. Drug Saf. 2018;41(10):919–31. These authors conducted a large systematic review documenting the cardiac complications of HCQ/CQ.
Thompson RB, Chow K, Khan A, Chan A, Shanks M, Paterson I, et al. T1 mapping with cardiovascular MRI is highly sensitive for Fabry disease independent of hypertrophy and sex. Circ Cardiovasc Imaging. 2013;6(5):637–45.
Haeusler IL, Chan XHS, Guérin PJ, White NJ. The arrhythmogenic cardiotoxicity of the quinoline and structurally related antimalarial drugs: a systematic review. BMC Med. 2018;16(1):200.
Mubagwa K. Cardiac effects and toxicity of chloroquine: a short update. Int J Antimicrob Agents. 2020;56(2):106057.
Padiyar S, Danda D. Revisiting cardiac safety of hydroxychloroquine in rheumatological diseases during COVID-19 era: facts and myths. Eur J Rheumatol. 2020;8(2):100–4.
Stevenson A, Kirresh A, Conway S, White L, Ahmad M, Little C. Hydroxychloroquine use in COVID-19: is the risk of cardiovascular toxicity justified? Open Heart. 2020;7(2):e001362.
Agstam S, Yadav A, Kumar-M P, Gupta A. Hydroxychloroquine and QTc prolongation in patients with COVID-19: a systematic review and meta-analysis. Indian Pacing Electrophysiol J. 2021;21(1):36–43.
Koh HM, Chong PF, Tan JN, Chidambaram SK, Chua HJ. QT prolongation associated with hydroxychloroquine and protease inhibitors in COVID-19. J Clin Pharm Ther. 2021;46(3):800–6.
Eftekhar SP, Kazemi S, Barary M, Javanian M, Ebrahimpour S, Ziaei N. Effect of hydroxychloroquine and azithromycin on QT interval prolongation and other cardiac arrhythmias in COVID-19 confirmed patients. Cardiovasc Ther. 2021;2021:6683098.
Saleh M, Gabriels J, Chang D, Kim BS, Mansoor A, Mahmood E, et al. Effect of chloroquine, hydroxychloroquine, and azithromycin on the corrected QT interval in patients with SARS-CoV-2 infection. Circ Arrhythm Electrophysiol. 2020;13(6):e008662.
Recanatini M, Poluzzi E, Masetti M, Cavalli A, De Ponti F. QT prolongation through hERG K(+) channel blockade: current knowledge and strategies for the early prediction during drug development. Med Res Rev. 2005;25(2):133–66.
Park E, Giles JT, Perez-Recio T, Pina P, Depender C, Gartshteyn Y, et al. Hydroxychloroquine use is not associated with QTc length in a large cohort of SLE and RA patients. Arthritis Res Ther. 2021;23(1):271.
Hooks M, Bart B, Vardeny O, Westanmo A, Adabag S. Effects of hydroxychloroquine treatment on QT interval. Heart Rhythm. 2020;17(11):1930–5.
Pareek A, Sharma TS, Mehta RT. Hydroxychloroquine and QT prolongation: reassuring data in approved indications. Rheumatol Adv Practice. 2020;4:rkaa044.
Bessière F, Roccia H, Delinière A, Charrière R, Chevalier P, Argaud L, et al. Assessment of QT intervals in a case series of patients with Coronavirus Disease 2019 (COVID-19) infection treated with hydroxychloroquine alone or in combination with azithromycin in an intensive care unit. JAMA Cardiol. 2020;5(9):1067–9.
Mercuro NJ, Yen CF, Shim DJ, Maher TR, McCoy CM, Zimetbaum PJ, et al. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(9):1036–41.
Volberg WA, Koci BJ, Su W, Lin J, Zhou J. Blockade of human cardiac potassium channel human <em>ether-a-go-go-</em>related gene (<em>HERG</em>) by macrolide antibiotics. J Pharmacol Exp Ther. 2002;302(1):320–7.
Mason JW. Antimicrobials and QT prolongation. J Antimicrob Chemother. 2017;72(5):1272–4.
Sapp JL, Alqarawi W, MacIntyre CJ, Tadros R, Steinberg C, Roberts JD, et al. Guidance on minimizing risk of drug-induced ventricular arrhythmia during treatment of COVID-19: a statement from the Canadian Heart Rhythm Society. Can J Cardiol. 2020;36(6):948–51.
Jankelson L, Karam G, Becker ML, Chinitz LA, Tsai M-C. QT prolongation, torsades de pointes, and sudden death with short courses of chloroquine or hydroxychloroquine as used in COVID-19: a systematic review. Heart Rhythm. 2020;17(9):1472–9.
Keating RJ, Bhatia S, Amin S, Williams A, Sinak LJ, Edwards WD. Hydroxychloroquine-induced dardiotoxicity in a 39-year-old woman with systemic lupus erythematosus and systolic dysfunction. J Am Soc Echocardiogr. 2005;18(9):981.e1-e5.
Kang Y, Wang H, Chen H, Wang B, Yang Y, Zhao X, et al. Suspected hydroxychloroquine-induced sinus bradycardia and QTc prolongation in a patient with COVID-19. Int Heart J. 2020;61(5):1056–8.
Capel RA, Herring N, Kalla M, Yavari A, Mirams GR, Douglas G, et al. Hydroxychloroquine reduces heart rate by modulating the hyperpolarization-activated current If: novel electrophysiological insights and therapeutic potential. Heart Rhythm. 2015;12(10):2186–94.
Costedoat-Chalumeau N, Hulot JS, Amoura Z, Leroux G, Lechat P, Funck-Brentano C, et al. Heart conduction disorders related to antimalarials toxicity: an analysis of electrocardiograms in 85 patients treated with hydroxychloroquine for connective tissue diseases. Rheumatology. 2007;46(5):808–10.
Yu Y, Xu J, Xie A, Liu S, Wang X, Zhu R, et al. Hydroxychloroquine inhibits cardiac conduction in aged patients with nonmalaria diseases. Kidney Dis. 2021;7(5):401–10.
Burrell ZL, Martinez AC. Chloroquine and hydroxychloroquine in the treatment of cardiac arrhythmias. N Engl J Med. 1958;258(16):798–800.
Schwaab B, Katalinic A, Böge UM, Loh J, Blank P, Kölzow T, et al. Quinidine for pharmacological cardioversion of atrial fibrillation: a retrospective analysis in 501 consecutive patients. Ann Noninvasive Electrocardiol. 2009;14(2):128–36.
Gupta A, Shields KJ, Manzi S, Wasko MC, Sharma TS. Association of hydroxychloroquine use with decreased incident atrial fibrillation in systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2021;73(6):828–32.
Lo CH, Wang YH, Tsai CF, Chan KC, Li LC, Lo TH, et al. Association of hydroxychloroquine and cardiac arrhythmia in patients with systemic lupus erythematosus: a population-based case control study. PLoS ONE. 2021;16(5):e0251918.
Misra DP, Gasparyan AY, Zimba O. Benefits and adverse effects of hydroxychloroquine, methotrexate and colchicine: searching for repurposable drug candidates. Rheumatol Int. 2020;40(11):1741–51.
Yusuf IH, Sharma S, Luqmani R, Downes SM. Hydroxychloroquine retinopathy. Eye (Lond). 2017;31(6):828–45.
Melles RB, Marmor MF. The risk of toxic retinopathy in patients on long-term hydroxychloroquine therapy. JAMA Ophthalmol. 2014;132(12):1453–60.
Sharma AN, Mesinkovska NA, Paravar T. Characterizing the adverse dermatologic effects of hydroxychloroquine: a systematic review. J Am Acad Dermatol. 2020;83(2):563–78.
Jallouli M, Francès C, Piette J-C, Huong DLT, Moguelet P, Factor C, et al. Hydroxychloroquine-induced pigmentation in patients with systemic lupus erythematosus: a case-control study. JAMA Dermatol. 2013;149(8):935–40.
Bajoghli A, Hernandez G, Cardis MA. Hydroxychloroquine-induced hyperpigmentation. J Rheumatol. 2020;47(11):1721–2.
Biguetti CC, Junior JFS, Fiedler MW, Marrelli MT, Brotto M. The toxic effects of chloroquine and hydroxychloroquine on skeletal muscle: a systematic review and meta-analysis. Sci Rep. 2021;11(1):6589.
Naddaf E, Paul P, AbouEzzeddine OF. Chloroquine and hydroxychloroquine myopathy: clinical spectrum and treatment outcomes. Front Neurol. 2021;11:616075.
Tselios K, Gladman DD, Su J, Urowitz MB. Antimalarials as a risk factor for elevated muscle enzymes in systemic lupus erythematosus. Lupus. 2016;25(5):532–5.
Schiemann U, Kellner H. Gastrointestinal side effects in the therapy of rheumatologic diseases. Z Gastroenterol. 2002;40(11):937–43.
Srinivasa A, Tosounidou S, Gordon C. Increased incidence of gastrointestinal side effects in patients taking hydroxychloroquine: a brand-related issue? J Rheumatol. 2017;44(3):398.
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56(1):105949.
Horby P, Mafham M, Linsell L, Bell JL, Staplin N, Emberson JR, et al. Effect of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020;383(21):2030–40. This is a large RCT that reports patients had a slightly greater risk of death from cardiac causes with HCQ. This is one of the two largest RCT's using HCQ in COVID-19.
Pan H, Peto R, Henao-Restrepo AM, Preziosi MP, Sathiyamoorthy V, Abdool Karim Q, et al. Repurposed antiviral drugs for Covid-19 - interim WHO solidarity trial results. N Engl J Med. 2021;384(6):497–511. This is a large RCT that reports no benefit of HCQ in COVID-19. This is one of the two largest RCT's using HCQ in COVID-19.
Axfors C, Schmitt AM, Janiaud P, van’t Hooft J, Abd-Elsalam S, Abdo EF, et al. Mortality outcomes with hydroxychloroquine and chloroquine in COVID-19 from an international collaborative meta-analysis of randomized trials. Nat Commun. 2021;12(1):2349.
Marin S, Val AM, Peligero MB, Rodríguez-Bernuz C, Pérez-Ricart A, Vilaró Jaques L, et al. Safety of short-term treatments with oral chloroquine and hydroxychloroquine in patients with and without COVID-19: a systematic review. Pharmaceuticals (Basel). 2022;15(5).
Niknam Z, Jafari A, Golchin A, Danesh Pouya F, Nemati M, Rezaei-Tavirani M, et al. Potential therapeutic options for COVID-19: an update on current evidence. Eur J Med Res. 2022;27(1):6.
Mahévas M, Tran V-T, Roumier M, Chabrol A, Paule R, Guillaud C, et al. Clinical efficacy of hydroxychloroquine in patients with covid-19 pneumonia who require oxygen: Observational comparative study using routine care data. Bmj. 2020;369:m1844.
Chen J, Liu D, Liu L, Liu P, Xu Q, Xia L, et al. A pilot study of hydroxychloroquine in treatment of patients with moderate COVID-19. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2020;49(2):215–9.
Tang W, Cao Z, Han M, Wang Z, Chen J, Sun W, et al. Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ. 2020;369:m1849.
Mitjà O, Corbacho-Monné M, Ubals M, Tebé C, Peñafiel J, Tobias A, et al. Hydroxychloroquine for early treatment of adults with mild coronavirus disease 2019: a randomized, controlled trial. Clin Infect Dis. 2021;73(11):e4073–81.
Cavalcanti AB, Zampieri FG, Rosa RG, Azevedo LCP, Veiga VC, Avezum A, et al. Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid-19. N Engl J Med. 2020;383(21):2041–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Luke Gagnon, Chandu Sadasivan, Dr. Haran Yogasundaram, and Dr. Gavin Oudit declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Clinical Heart Failure
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gagnon, L.R., Sadasivan, C., Yogasundaram, H. et al. Review of Hydroxychloroquine Cardiotoxicity: Lessons From the COVID-19 Pandemic. Curr Heart Fail Rep 19, 458–466 (2022). https://doi.org/10.1007/s11897-022-00581-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11897-022-00581-y