Abstract
Summary
It is important for postmenopausal women to acquire bone health protective behaviors to protect them from fractures. For this reason, it is necessary to evaluate bone health during menopause and to inform women.
Purpose
This study was conducted to examine osteoporotic fracture protection behaviors, quality of life, and self-efficacy in postmenopausal women.
Methods
In the study, the data were evaluated with the socio-demographic data form, Osteoporotic Fracture Protection Scale, Osteoporosis Self-Efficacy-Efficacy Scale, European Osteoporosis Foundation Quality of Life Questionnaire-41, which includes introductory information on socio-demographic characteristics.
Results
It was determined that the postmenopausal women included in our study were between the ages of 45–92; more than half of them had chronic diseases; their average BMI was 29; and their DEXA score was − 3.00 ± 0.41. Among the people included in our study, those with a history of fractures had lower self-efficacy scores. It was determined that the fracture prevention scale scores of the participants were above the average, and the average of the osteoporosis-related quality of life score was high. In addition, it was determined that there was a strong positive correlation between self-efficacy and fracture prevention scale.
Conclusion
It is important to determine behaviors to prevent osteoporotic fractures in postmenopausal women, to raise the necessary awareness and to inform patients about the precautions to be taken. It is thought that it will increase patients’ quality of life by increasing their disease-related self-efficacy. Therefore, there is a need for research on providing education to op patients and examining the results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is defined as a systemic skeletal disease characterized by low bone mass and disruption of the microarchitecture of bone tissue, resulting in increased bone fragility and fracture risk. With accelerated bone loss after menopause, bone mass decreases with age, and the risk of osteoporotic fractures increases [1]. Life expectancy in the world has been increasing in recent years [2, 3]. The population of our country is not a young population with high fertility and mortality rates; it has low fertility and mortality rates and is getting older [4, 5]. According to the 2014 data of the Turkish Statistical Institute (TUIK), the rate of the elderly population in our country is 8%. It is estimated that it will increase to 10.2% in 2023, 20.8% in 2050, and 27.7% in 2075 [5, 6]. The rates of chronic diseases also increased with advancing age. In multicenter studies conducted throughout Turkey, chronic diseases frequently seen in the elderly are, respectively, hypertension 30.7%, osteoarthritis 13.7%, chronic heart failure 13.7%, diabetes mellitus 10.2%, coronary artery disease 9.8%, and osteoporosis 8.2% [7]. Especially in postmenopausal women, osteoporotic fractures occur due to decreased bone density. Major osteoporotic fractures include fractures of the vertebrae, hip, distal forearm, and proximal humerus osteoporotic fractures. It causes a decrease in the quality of life, being bedridden for a long time, an increase in health expenditures, surgical operations or death as a result [8].
In the coming years, it is estimated that osteoporotic fractures will significantly affect postmenopausal women in all countries of the world. The risk of osteoporotic fractures nearly doubles every 5–7 years due to osteoporosis. It is thought that the prevention and treatment of osteoporotic fractures will become a serious public health problem in the coming years. Strategies to protect from fracture are constantly evolving on how to manage osteoporotic fractures when they occur [9, 10].
Osteoporosis increases the risk of fractures associated with increased mortality and lower quality of life. At age 50, the lifetime risk of osteoporotic fractures is close to 50% for women and greater than 20% for men. The clinical significance of osteoporosis is determined by subsequent fractures leading to deterioration in quality of life [8]. It is important to determine the behaviors to prevent osteoporotic fractures in postmenopausal women, to raise the necessary awareness, and to inform the patients about the precautions to be taken. This study was carried out to examine the osteoporotic fracture prevention behaviors and quality of life self-efficacy status in postmenopausal women.
Material and method
This cross-sectional study was conducted between June 2022 and December 2022. A total of 100 postmenopausal women who applied to the Kutahya Health of Science University physical therapy and rehabilitation outpatient clinic in Turkey due to musculoskeletal pain were included in the study. The patients included in the study were diagnosed at least 1 year ago.
The 100 postmenopausal women screened for osteoporosis with DEXA were included in the study. Participants with a DEXA score of lumbar and/or femur T score of − 2.5 and below and diagnosed with osteoporosis were included in the study. DEXA evaluation, which is routinely done in clinical practice, was performed on all those participating in the study.
A diagnosis of osteoporosis in patients whose bone mineral density (BMD) was measured by dual-energy X-ray absorptiometry (DEXA) (GE LUNAR DPX-NT) was made. It will be determined by evaluating the T score based on the World Health Organization criteria. In the study, BMD values with a bone mineral density T score of the lumbar region and femoral neck T score below − 2.5 SD compared to the average of same-sex adults in at least one region were accepted as “osteoporosis.”
Data collection tools
In the study, the data were evaluated with the socio-demographic data form, Osteoporotic Fracture Protection Scale, Osteoporosis Self-Efficacy-Efficacy Scale, European Osteoporosis Foundation Quality of Life Questionnaire-41, which includes introductory information on socio-demographic characteristics.
Socio-demographic data form
Participants included socio-demographic characteristics and features that may affect fracture development (activity in daily work, fall history and time, fall-related fracture status and region, activity status, experience of falling and fracture, orthopedic surgery, use of assistive orthopedic tools, and diagnosis of osteoporosis and osteoporosis). Time was evaluated with a questionnaire about the DEXA score.
OFPS
An Osteoporotic Fracture Prevention Scale (OFPS), developed in 2015 based on the planned behavior model, was used to evaluate the intention and behavior towards prevention of osteoporotic fracture. The scale includes 22 five-point Likert propositions. OFPS consists of 6 sub-headings: belief, attitude and behavior control, diagnosis and treatment behavior, disability perception, fall prevention intention, and diagnosis and treatment intention. It contains recommendations on bone mineral density measurement for diagnosis and follow-up, drug treatment, following calcium-rich diet and sunbathing recommendations, daily physical activity and/or regular physical exercise, and making home arrangements to prevent falls. The internal consistency of the scale is Cronbach’s a coefficient of 0.95. The lowest score that can be obtained from the scale is 22, and the highest score is 110. A high score indicates the high level of protection from osteoporotic fracture. The scale was found to be highly valid and reliable in Turkish population. It can be a part of the public health model aimed at preventing osteoporotic fractures [10].
QUALEFFO-41
European Osteoporosis Foundation Quality of Life Questionnaire-41 (Quality of Life Questionnaire of the European Foundation for Osteoporosis-41, QUALEFFO-41) is a self-assessment scale that is widely used in the evaluation of OP-specific quality of life; it is reproducible and can clearly reveal the differences between the patients and the control group. This scale consists of 41 questions in the subgroups of pain (5 questions), physical function (17 questions), social function (7 questions), general health assessment (3 questions), and mental function (9 questions). While 0 points for total score and subgroup scores indicate the best health status, higher scores mean poor quality of life. Turkish validity and reliability were evaluated by Koçyiğit et al. [11].
The answers to the questions in the QUALEFFO-41 scale are scored from 1 (healthy) to 5 (unhealthy), respectively; between 1 and 3 for questions 23, 24, 25, and 26; for questions 27, 28, and 29, between 1 and 4. The remaining questions were scored between 1 and 5. For questions 24, 26, and 29, no points were given for the options “this question does not apply to me” or “I do not go to the cinema or the theater.” While scoring the 33rd, 34th, 35th, 37th, 39th, and 40th questions, the order of the options is reversed so that the order is from the best health (1 point) to the worst health (5 points), as in the other questions. The section score and the total score are calculated by transferring the scores to a formula made out of 100. With this formula, each subscale and total QUALEFFO-41 scores are calculated. For each subgroup and total result in the scale, 0 points indicate the best health status, while 100 points indicate the worst health status. The formula used is as follows [12, 13].
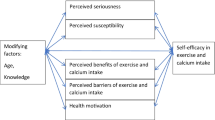
Osteoporosis Self-Efficacy Scale
It was developed by Gendler, Horan and Kim, and its Turkish validity and reliability were made by Kılıç. Marking on a 12-item visual-like scale is done on a scale that includes numbers from 0 to “I have no confidence at all” to 10 “I have a lot of confidence.” A score between 0 and 100 is taken as basis for each item. The total score of the scale is 0 at the lowest and 1200 at the highest. Cronbach alpha reliability coefficient ranges between 0.96 and 0.98.
Osteoporosis Exercise Self-Efficacy Scale
It determines the degree of perceived confidence in performing exercises and activities for the Prevention of Osteoporosis Scale. It includes items 1, 2, 3, 4, 5, and 6.
Osteoporosis Calcium Self-Efficacy Scale
The scale determines the degree of perceived confidence in carrying out activities related to calcium intake for the Prevention of Osteoporosis Scale. It contains items 7, 8, 9, 10, 11, and 12 [12, 14].
Inclusion criteria
-
Postmenopausal women
-
Able to communicate in Turkish
-
It was planned to include individuals who were literate and who agreed to participate in the study among patients without a psychiatric illness.
Exclusion criteria
-
Those with severe hearing loss or visual impairment, who have undergone major surgery in the last 2 months, with extremity amputation, who are scheduled for surgery soon, and with acute trauma
-
Patients who have surgically entered menopause
-
Those who are treated for malignancy
-
Terminal stage cancer patients
-
Those who have literacy and comprehension problems
-
Those with communication problems and those who did not agree to participate in the research were not included in the research.
Statistical analysis
Frequency tables and descriptive statistics were used to interpret the findings for statistical analysis (Table 1). The “Student’s t test” t-table value was used to compare the scale score averages of the independent variables with normal distribution. Pearson correlation “r” coefficient was used for normally distributed averages in the comparison of the relationship between the scale point averages according to the research question.
Results
It was determined that the participants were 65.3 ± 9.79 years old on average; their average BMI was 29.10 ± 5.03; and their DEXA score was − 3.00 ± 0.41. It was determined that the majority of the participants were married; more than half of them were secondary school graduates; and 77% of them were engaged in activities in their daily work.
It was determined that the mean disease duration of the participants was 9.01 ± 5.41 years; 62% had a history of falling; nearly half had a history of fracture; and 88% had a chronic disease. It was determined that the majority of the patients did not smoke or use alcohol (Table 2).
It was determined that the Osteoporosis Self-Efficacy Scale score of the participants was close to the average (min 0–max 120) (Table 3). It was determined that the participants’ Osteoporotic Fracture Prevention Behavior Scale scores were above the average (min 22–max 110). It was determined that the European Osteoporosis Quality of Life Scale score average of the participants was quite high (min 0–max 100).
When the relationship between the participants’ Fracture Prevention Behaviors, Quality of Life and Self-Efficacy Scales was examined, it was determined that there was a strong positive relationship between OSES and OFPS and a strong negative relationship between OSES and QUALEFFO (Table 4). It was determined that there was a positive relationship between the participants’ DEXA scores and OSES and a negative relationship between QUALEFFO.
It was determined that the participants who were active in their daily work had higher OSES scores and lower QUALEFFO scores (Table 5). Participants with a history of falling had lower OSES and OFPS scores but higher QUALEFFO. Participants with a history of fractures had lower OSES scores. In addition, participants with a history of fracture were found to have higher QUALEFFO. Participants using assistive devices had lower OSES and OFPS scores but higher QUALEFFO scores.
Discussion
It was determined that the postmenopausal women included in our study were between the ages of 45–92; more than half of them had chronic diseases; their average BMI was 29; and their DEXA score was − 3.00 ± 0.41. Low bone density is known to be associated with a higher fracture rate, and many studies show an association between early menopause, oophorectomy, and an increase in osteoporotic fractures [15].
Among the participants included in our study, those with a history of fracture had lower OSES scores. In Akpınar’s study, 46% of women experienced a fall. Fractures developed in approximately one third of those who fell [16]. Çıtıl et al. reported that 50% of women fell within the last month; 23% fell more than once; and 9% suffered fractures as a result of falling [17]. It is thought that the level of self-efficacy is affected, and the quality of life is affected due to the high rates of fractures and negative health outcomes.
In a study conducted with 419 women between the ages of 19 and 60 with different education levels, it was reported that the osteoporosis self-efficacy level was low [18]. Arslan et al. found that the OSES scores of the participants were low in their study, which included 236 individuals over the age of 35, 53.4% female and 34.7% literate, who applied to the bone densitometry unit of a hospital [19].
It was determined that the OFPS scores of the participants were above the average. The Centers for Disease Control determined people who needed screening. Screening is recommended for Caucasian women aged 65 years or above without any additional risk factors, while it is recommended for younger women who are at risk for OP and fractures [20]. The OSES scores of the participants included in our study were found to be close to the average. It was determined that the average QUALEFFO score of the participants was high. While 0 points for total score and subgroup scores indicate the best health status, higher scores mean poor quality of life. It was determined that there was a strong positive relationship between OSES and OFPS of the participants and a strong negative relationship between OSES and QUALEFFO. In the study of Ahn and Oh, which included elderly women, it was determined that there was a positive relationship between osteoporosis exercise self-efficacy and diet self-efficacy and protective behaviors from osteoporosis [21]. Wu and Sheng conducted a study with elderly individuals and determined that there is a positive relationship between “self-efficacy” and “healthy lifestyle behaviors” for health practices [22]. Guntzviller et al. reported that exercise self-efficacy is associated with exercise behavior in low-income adults [23]. It is known that physically inactive individuals have a higher incidence of osteoporosis and related complications [24]. In the study of Arslan et al., it is shown that the higher the education level, the higher the osteoporosis self-efficacy-efficacy level [19]. When the results are examined, it is thought that people with high osteoporosis self-efficacy can develop fracture prevention behaviors, and their quality of life is affected by this situation. In addition, it is known that the level of self-efficacy is affected by education level and socioeconomic status.
Conclusion
It is important to determine behaviors to prevent osteoporotic fractures in postmenopausal women, to raise the necessary awareness and to inform patients about the precautions to be taken. It is thought that it will increase patients’ quality of life by increasing their disease-related self-efficacy. Therefore, there is a need for research on providing education to op patients and examining the results.
References
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24:23–57
Anderson GF, Hussey PS (2000) Population aging: a comparison among industrialized countries: populations around the world are growing older, but the trends are not cause for despair. Health Aff 19(3):191–203
World Health Statistic 2014. www.who.int. Accessed 20 Nov 2023
Altındiş M (2013) Yaşlılarda güncel sağlık sorunları ve bakımı. İstanbul Tıp Kitabevleri, İstanbul, Türkiye, ss 2–8
Türkiye İstatistik Kurumu Basın Odası Haberleri.Yaşlanıyoruz. Sayı:2014/4 http://www.tuik.gov.tr/basinOdasi/haberler/2014_4_20140203.pdf
Beğer T, Yavuzer H (2012) Yaşlılık ve yaşlılık epidemiyolojisi. Klinik Gelişim 25(3):1–3
Altındağ Ö, Soran N (2014) Osteoporosis significantly reduces quality of life. Gaziantep Med J 20(3):217–220
Rizzoli R (2018) Postmenopausal osteoporosis: assessment and management. Best Pract Res Clin Endocrinol Metab 32(5):739–757
Koval KJ, Riehl JT, Baldwin PC and Kates SL (2015) Osteoporotic fragility fractures, chapter 21. Browner BD, Jupiter JB, Krettek C, Anderson PA (ed) Skeletal Trauma: Basic Science, Management, and Reconstruction, Fifth Edn. p 561–569.e2
Aydın S, Kurçer MA, & Erdoğan Z (2021) Development of the Protection Against Osteoporotic Fractures Scale. Turkish Journal of Osteoporosis/Turk Osteoporoz Dergisi 27(1)
Kocyigit H, Gülseren S, Erol A, Hizli N, Memis A (2003) The reliability and validity of the Turkish version of Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Clin Rheumatol 22:18–23
Pamuk, G, Kutlu, R, Çivi, S (2014) Osteoporozu Olan ve Olmayan Postmenopozal Kadınlarda QUALEFFO-41 Ölçeği ile Yaşam Kalitesinin Değerlendirilmesi. Turkish J Phys Med Rehabilitation/Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi 60(2)
Lips PTM, Cooper C, Agnusdei DF, Caulin F, Egger P, Johnell O, ... & Wiklund I (1999) Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). Osteoporosis Int 10(2): 150–160
Kılıç D, Behice E, Ölçeği Osteoporoz Sağlık İnanç (2004) Osteoporoz Öz-Etkililik/Yeterlik Ölçeği ve Osteoporoz Bilgi Testi’nin Geçerlilik ve Güvenirliği. Anadolu Hemşirelik ve Sağlık Bilimleri Dergisi 7(2):89–102
Gallagher JC (2007) Effect of early menopause on bone mineral density and fractures. J North Am Menopause Soc 14(3):567–571
Akpınar CV (2019) Bir Fizik Tedavi Dal Merkezine Başvuran Postmenapozal Kadınlarda Osteoporotik Kırıklardan Korunma Davranışının Belirlenmesi. Sürekli Tıp Eğitimi Dergisi 28(3):201–195
Çıtıl R, Özdemir M, Poyrazoğlu S, Balcı E, Aykut M, Öztürk Y (2007) Kayseri Melikgazi Sağlık Grup Başkanlığı Bölgesindeki Kadınların Osteoporoza Yönelik Bilgi ve Davranışları. Osteoporoz Dünyasından 13:60–66
Gezer C, Ocak E (2019) The level of osteoporosis knowledge and the related factors among women who attended Iskenderun Public Education Center Courses. Türk Osteoporoz Dergisi 25(2):58–64
Arslan SA, Daşkapan A, Atalay DK, Tüzün EH, Korkem D (2015) Kırıkkale ilinde yaşayan kadınların osteoporoz bilgi düzeyi. Türk Fizyoterapi ve Rehabilitasyon Dergisi 26(3):120–127
Czerwiński E, Badurski JE, Marcinowska-Suchowierska E, Osieleniec J (2007) Current understanding of osteoporosis according to the position of the World Health Organization (WHO) and International Osteoporosis Foundation. Ortop Traumatol Rehabil 9:337–356
Ahn S, Oh J (2018) Relationships among knowledge, self-efficacy, and health behavior of osteoporosis and fall prevention in old aged women. Korean J Women Health Nurs 24(2):209–218
Wu F, Sheng Y (2019) Social support network, social support, self-efficacy, health-promoting behavior and healthy aging among older adults: a pathway analysis. Arch Gerontol Geriatr 85:103934
Guntzviller LM, King AJ, Jensen JD, Davis LA (2017) Self-efficacy, health literacy, and nutrition and exercise behaviors in a low-income, Hispanic population. J Immigr Minor Health 19(2):489–493
Özgürbüz C (2008) Osteoporoz ve fiziksel aktivite. Spor Hekimliği Dergisi 43:99–109
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
Concept: GÜ, AÖ, AE, MFÖ. Design: AÖ, AE. Data Collection or Processing: AE, MFÖ, Analysis or Interpretation: GÜ, AÖ, AE, MFÖ, Literature Search: GÜ, AÖ,SÜ Writing: GÜ, AÖ,SÜ.
Corresponding author
Ethics declarations
Ethics approval
Approval for the study was granted by the Clinical Research Ethics Committee at Kutahya Health of Science University.
Informed consent
Consent form was obtained from all the patients participating in the study.
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ünver, G., Özlü, A., Erdoğan, A. et al. Osteoporotic quality of life, self-efficacy, and fracture protection behaviors in postmenopausal women. Arch Osteoporos 19, 22 (2024). https://doi.org/10.1007/s11657-024-01377-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-024-01377-4