Abstract
Summary
This study provides a national estimate of the incidence of hospitalizations and assesses the clinical features and outcomes during inpatient admission due to osteoporotic fractures diagnosed by ICD-10-CM/PCS among the elderly in the USA, using the US Nationwide Inpatient Sample, 2016–2018.
Purpose
To provide a national estimate of the incidence of hospitalizations and assess the clinical features and outcomes during inpatient admission due to osteoporotic fractures (OFs) among the elderly in the USA.
Methods
The study included all inpatients aged 65 years and older who participated in the US Nationwide Inpatient Sample (NIS). We conducted a retrospective analysis of hospitalizations with OFs diagnosed by the International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Coding System (ICD-10-CM/PCS), using the US NIS, 2016–2018. Trends in epidemiological characteristics and outcomes were calculated by annual percentage change (APC).
Results
From 2016 to 2018, there were an estimated 0.16 million hospitalizations for OFs, and the estimated annual incidence rate changed from 995 cases per 1 million persons in 2016 to 1114 cases per 1 million persons in 2018 (APC, 5.8% [95% CI, 0.0 to 12.0]; P > 0.05). Over two-thirds of the patients (68.2%) were age-related osteoporosis with current pathological fracture, and OFs were more likely to occur in vertebra (51.7%) and femur (34.7%). During the hospitalization, the average length of stay (LOS) was 5.83 days, the average cost reached $60,901.04, and the overall mortality was 2.3%. All outcomes including LOS, average cost and mortality did not change significantly in 2016–2018 (all P values for trend were over 0.05).
Conclusion
Between 2016 and 2018, the incidence rate of OFs remained relatively stable, but the total number of cases was huge. OFs was predominantly age-related, mostly in vertebrae and femurs, with relatively stable cost and mortality during hospitalization.

Similar content being viewed by others
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393:364–376
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16 Suppl 2:S3-7
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Singer A, Exuzides A, Spangler L, O’Malley C, Colby C, Johnston K, Agodoa I, Baker J, Kagan R (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90:53–62
Lippuner K, Grifone S, Schwenkglenks M, Schwab P, Popp AW, Senn C, Perrelet R (2012) Comparative trends in hospitalizations for osteoporotic fractures and other frequent diseases between 2000 and 2008. Osteoporos Int 23:829–839
Ziadé N, Jougla E, Coste J (2010) Population-level impact of osteoporotic fractures on mortality and trends over time: a nationwide analysis of vital statistics for France, 1968–2004. Am J Epidemiol 172:942–951
Siggeirsdottir K, Aspelund T, Jonsson BY, Mogensen B, Gudmundsson EF, Gudnason V, Sigurdsson G (2014) Epidemiology of fractures in Iceland and secular trends in major osteoporotic fractures 1989–2008. Osteoporos Int 25:211–219
Kelly MA, McGowan B, McKenna MJ, Bennett K, Carey JJ, Whelan B, Silke C (2018) Emerging trends in hospitalisation for fragility fractures in Ireland. Ir J Med Sci 187:601–608
World Health Organization (2021) ICD-10 Version:2008. Available at: https://icd.who.int/browse10/2008/en. Accessed on October 14,2021
Lippuner K, Golder M, Greiner R (2005) Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporos Int 16 Suppl 2:S8–S17
Healthcare Cost and Utilization Project (2021) NIS Description of data elements. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/nisdde.jsp. Accessed on October 14,2021
Dhital R, Lynn T, Tachamo N, Poudel DR (2019) The trend of osteoporosis and osteoporotic fragility fractures in inpatients: results from a national database. J Community Hosp Intern Med Perspect 9:211–214
Wang Y, Li J, Zheng X, Jiang Z, Hu S, Wadhera RK, Bai X, Lu J, Wang Q, Li Y, Wu C, Xing C, Normand SL, Krumholz HM, Jiang L (2018) Risk factors associated with major cardiovascular events 1 year after acute myocardial infarction. JAMA Netw Open 1:e181079
US Census Bureau (2021) Annual estimates of the resident population by single year of age and sex for the United States: April 1, 2010 to July 1, 2019. Available at: https://www.census.gov/popest/data/historical/2010s. Accessed on October 14,2021
Harrell Jr FE (2015) Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. Springer
National Cancer Institute (2021) Joinpoint regression program. Available at: https://surveillance.cancer.gov/joinpoint/ Accessed on April 22,2021
Centers for Disease Control and Prevention (2021) International Classification of Diseases,Ninth Revision, Clinical Modification (ICD-9-CM). Available at: https://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed on October 14,2021
Centers for Disease Control and Prevention (2021) International Classification of Diseases,Tenth Revision, Clinical Modification (ICD-10-CM). Available at: https://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed on October 14,2021
Nordin BE, Aaron J, Speed R, Crilly RG (1981) Bone formation and resorption as the determinants of trabecular bone volume in postmenopausal osteoporosis. Lancet 2:277–279
Hamann C, Kirschner S, Günther KP, Hofbauer LC (2012) Bone, sweet bone–osteoporotic fractures in diabetes mellitus. Nat Rev Endocrinol 8:297–305
Smith RW Jr, Eyler WR, Mellinger RC (1960) On the incidence of senile osteoporosis. Ann Intern Med 52:773–781
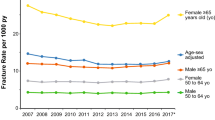
Lewiecki EM, Chastek B, Sundquist K, Williams SA, Weiss RJ, Wang Y, Fitzpatrick LA, Curtis JR (2020) Osteoporotic fracture trends in a population of US managed care enrollees from 2007 to 2017. Osteoporos Int 31:1299–1304
Khosla S, Hofbauer LC (2017) Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol 5:898–907
Eastell R, O’Neill TW, Hofbauer LC, Langdahl B, Reid IR, Gold DT, Cummings SR (2016) Postmenopausal osteoporosis. Nat Rev Dis Primers 2:16069
Rachner TD, Khosla S, Hofbauer LC (2011) Osteoporosis: now and the future. Lancet 377:1276–1287
Ensrud KE, Kats AM, Boyd CM, Diem SJ, Schousboe JT, Taylor BC, Bauer DC, Stone KL, Langsetmo L (2019) Association of disease definition, comorbidity burden, and prognosis with hip fracture probability among late-life women. JAMA Intern Med 179:1095–1103
Huybrechts KF, Ishak KJ, Caro JJ (2006) Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone 38:922–928
Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM, Pressman AR, Ettinger B (2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
Yu EW Screening for osteoporosis. Mulder JE (ed) UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com. Accessed on October 14, 2021
Shanbhogue VV, Mitchell DM, Rosen CJ, Bouxsein ML (2016) Type 2 diabetes and the skeleton: new insights into sweet bones. Lancet Diabetes Endocrinol 4:159–173
Napoli N, Chandran M, Pierroz DD, Abrahamsen B, Schwartz AV, Ferrari SL (2017) Mechanisms of diabetes mellitus-induced bone fragility. Nat Rev Endocrinol 13:208–219
Decramer M, Janssens W (2013) Chronic obstructive pulmonary disease and comorbidities. Lancet Respir Med 1:73–83
Iqbal F, Michaelson J, Thaler L, Rubin J, Roman J, Nanes MS (1999) Declining bone mass in men with chronic pulmonary disease: contribution of glucocorticoid treatment, body mass index, and gonadal function. Chest 116:1616–1624
Xia WF, Jung JU, Shun C, Xiong S, Xiong L, Shi XM, Mei L, Xiong WC (2013) Swedish mutant APP suppresses osteoblast differentiation and causes osteoporotic deficit, which are ameliorated by N-acetyl-L-cysteine. J Bone Miner Res 28:2122–2135
Annweiler C, Rolland Y, Schott AM, Blain H, Vellas B, Herrmann FR, Beauchet O (2012) Higher vitamin D dietary intake is associated with lower risk of Alzheimer’s disease: a 7-year follow-up. J Gerontol A Biol Sci Med Sci 67:1205–1211
Yuan J, Meloni BP, Shi T, Bonser A, Papadimitriou JM, Mastaglia FL, Zhang C, Zheng M, Gao J (2019) The potential influence of bone-derived modulators on the progression of Alzheimer’s disease. J Alzheimers Dis 69:59–70
Stone KL, Seeley DG, Lui LY, Cauley JA, Ensrud K, Browner WS, Nevitt MC, Cummings SR (2003) BMD at multiple sites and risk of fracture of multiple types: long-term results from the Study of Osteoporotic Fractures. J Bone Miner Res 18:1947–1954
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Ahrenfeldt LJ, Pedersen JK, Thinggaard M, Christensen K, Lindahl-Jacobsen R (2020) Sex differences in health and mortality by income and income changes. J Epidemiol Community Health 74:225–231
Montagnani A, Mathieu G, Pomero F, Bertù L, Manfellotto D, Campanini M, Fontanella A, Sposato B, Dentali F (2020) Hospitalization and mortality for acute exacerbation of chronic obstructive pulmonary disease (COPD): an Italian population-based study. Eur Rev Med Pharmacol Sci 24:6899–6907
North BJ, Sinclair DA (2012) The intersection between aging and cardiovascular disease. Circ Res 110:1097–1108
Solfrizzi V, Scafato E, Seripa D, Lozupone M, Imbimbo BP, D’Amato A, Tortelli R, Schilardi A, Galluzzo L, Gandin C, Baldereschi M, Di Carlo A, Inzitari D, Daniele A, Sabbà C, Logroscino G, Panza F (2017) Reversible cognitive frailty, dementia, and all-cause mortality The Italian longitudinal study on aging. J Am Med Dir Assoc 18:89.e1-89.e8
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. Lancet 381:752–762
Funding
This study was funded by the Clinical Research Center of Shandong University (Nos. 2021SDUCRCC002, 2020SDUCRCA008), Taishan Scholars Program of Shandong Province-Young Taishan Scholars (No. tsqn201909197), and the National Natural Science Foundation of China (Nos. 81972073 and 81930070).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Yongfu Lou, Wei Wang, Chaoyu Wang, Runhan Fu, Shenghui Shang, Yi Kang, Chi Zhang, Huan Jian, Yigang Lv, Mengfan Hou, Lingxiao Chen, Hengxing Zhou, and Shiqing Feng declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lou, Y., Wang, W., Wang, C. et al. Clinical features and burden of osteoporotic fractures among the elderly in the USA from 2016 to 2018. Arch Osteoporos 17, 78 (2022). https://doi.org/10.1007/s11657-022-01113-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01113-w