Abstract
Objectives
Brain metastasis (BM) is a common event during the development of many cancers, and is also one of the main causes of death of patients. Stereotactic radiosurgery (SRS) is an effective treatment for BM. The prognostic effects of various clinical factors on local control (LC) and overall survival (OS) after SRS treatment are still unclear. The purpose of this study is to retrospectively analyze the intracranial progression free survival (iPFS) and OS of patients receiving SRS treatment, and explore the relationship between various clinical characteristics and patient prognosis.
Materials and methods
We collected the clinical information of patients who were diagnosed with BM and received SRS treatment in our center between 2018 and 2021. Univariate and multivariate Cox regression analysis and KM analysis for iPFS and OS were conducted in R software to investigate the prognostic effects of clinical characteristics.
Results
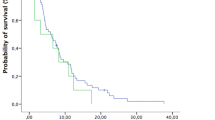
In total, 183 patients that received SRS in our center were enrolled in the cohort. The median iPFS for all patients was 8.87 months (95% CI 6.9–10.6), and the median OS was 16.5 months (95% CI 12.9–20.7). BM number > = 5 (HR 1.965 [95% CI 1.381–2.796], p < 0.001, FDR-corrected p < 0.001) was found to be strong predictor for shorter iPFS and OS. Subgroup analysis showed that patients with cumulative intracranial tumor volume (CITV) > = 2.14 cm3 and number > = 5 had shortest iPFS (P < 0.001) and OS (P = 0.007), compared with other subgroups. For patients with more than 5 BMs, SRS plus whole brain radiotherapy (WBRT) could achieve better local control, compared with SRS alone group (P = 0.0357). Peripheral blood inflammation indicators were associated with the prognosis of BM patients in univariate Cox analysis, but not in multivariate Cox analysis.
Conclusions
BM number is an independent prognostic factor for BM patients. The prognosis of patients in the subgroup with larger CITV and more BM is the worst. For patients with more than 5 BM, the combination of SRS and WBRT can improve the local control, but cannot prolong the OS.





Similar content being viewed by others
Abbreviations
- BM:
-
Brain metastasis
- SRS:
-
Stereotactic radiosurgery
- LC:
-
Local control
- OS:
-
Overall survival
- iPFS:
-
Intracranial progression free survival
- WBRT:
-
Whole brain radiotherapy
- WLR:
-
White cell-to lymphocyte ratio
- NLR:
-
Neutrophil-to-lymphocyte ratio
- MLR:
-
Monocyte-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- KM:
-
Kaplan–Meier survival curve
- ECM:
-
Extracranial metastases
- PD:
-
Progression disease
- SD:
-
Stable disease
- PR:
-
Partial remission
- CITV:
-
Cumulative intracranial tumor volume
- BED10 :
-
Biological equivalent dose with α/β = 10
References
Hardesty DA, Nakaji P (2016) The current and future treatment of brain metastases. Front Surg 3:30
Sprowls SA, Arsiwala TA, Bumgarner JR, Shah N, Lateef SS, Kielkowski BN et al (2019) Improving CNS delivery to brain metastases by blood-tumor barrier disruption. Trends Cancer 5(8):495–505
Achrol AS, Rennert RC, Anders C, Soffietti R, Ahluwalia MS, Nayak L et al (2019) Brain metastases. Nat Rev Dis Primers 5(1):5
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A (2002) Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 94(10):2698–2705
Siegel RL, Miller KD, Fuchs HE, Jemal A (2022) Cancer statistics, 2022. CA Cancer J Clin 72(1):7–33
Tabouret E, Chinot O, Metellus P, Tallet A, Viens P, Goncalves A (2012) Recent trends in epidemiology of brain metastases: an overview. Anticancer Res 32(11):4655–4662
Fortin D (2012) The blood-brain barrier: its influence in the treatment of brain tumors metastases. Curr Cancer Drug Targets 12(3):247–259
Lindquist C (1989) Gamma knife surgery for recurrent solitary metastasis of a cerebral hypernephroma: case report. Neurosurgery 25(5):802–804
Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 316(4):401–409
Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29(2):134–141
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295(21):2483–2491
Lin X, DeAngelis LM (2015) Treatment of brain metastases. J Clin Oncol 33(30):3475–3484
Bhatnagar AK, Flickinger JC, Kondziolka D, Lunsford LD (2006) Stereotactic radiosurgery for four or more intracranial metastases. Int J Radiat Oncol Biol Phys 64(3):898–903
Limon D, McSherry F, Herndon J, Sampson J, Fecci P, Adamson J et al (2017) Single fraction stereotactic radiosurgery for multiple brain metastases. Adv Radiat Oncol 2(4):555–563
Routman DM, Bian SX, Diao K, Liu JL, Yu C, Ye J et al (2018) The growing importance of lesion volume as a prognostic factor in patients with multiple brain metastases treated with stereotactic radiosurgery. Cancer Med 7(3):757–764
Yamamoto M, Kawabe T, Sato Y, Higuchi Y, Nariai T, Barfod BE et al (2013) A case-matched study of stereotactic radiosurgery for patients with multiple brain metastases: comparing treatment results for 1–4 vs >/= 5 tumors: clinical article. J Neurosurg 118(6):1258–1268
Sperduto PW, Shanley R, Luo X, Andrews D, Werner-Wasik M, Valicenti R et al (2014) Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1–3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys 90(3):526–531
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37(4):745–751
Sperduto PW, Chao ST, Sneed PK, Luo X, Suh J, Roberge D et al (2010) Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys 77(3):655–661
Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70(2):510–514
Sperduto PW, Yang TJ, Beal K, Pan H, Brown PD, Bangdiwala A et al (2017) Estimating survival in patients with lung cancer and brain metastases: an update of the graded prognostic assessment for lung cancer using molecular markers (Lung-molGPA). JAMA Oncol 3(6):827–831
Baschnagel AM, Meyer KD, Chen PY, Krauss DJ, Olson RE, Pieper DR et al (2013) Tumor volume as a predictor of survival and local control in patients with brain metastases treated with Gamma Knife surgery. J Neurosurg 119(5):1139–1144
Bagshaw HP, Ly D, Suneja G, Jensen RL, Shrieve DC (2016) Local control of melanoma brain metastases treated with stereotactic radiosurgery. J Radiosurg SBRT 4(3):181–190
Garsa AA, Badiyan SN, DeWees T, Simpson JR, Huang J, Drzymala RE et al (2014) Predictors of individual tumor local control after stereotactic radiosurgery for non-small cell lung cancer brain metastases. Int J Radiat Oncol Biol Phys 90(2):407–413
Ko PH, Kim HJ, Lee JS, Kim WC (2020) Tumor volume and sphericity as predictors of local control after stereotactic radiosurgery for limited number (1–4) brain metastases from nonsmall cell lung cancer. Asia Pac J Clin Oncol 16(3):165–171
Lai M, Li S, Zhou J, Zhen J, Li J, Hu Q et al (2021) Stereotactic radiosurgery for treatment of large cerebellum metastases from lung cancer. Ann Palliat Med 10(1):220–228
Matsunaga S, Shuto T, Serizawa T, Aoyagi K, Hasegawa T, Kawagishi J et al (2022) Gamma Knife radiosurgery for metastatic brain tumors from ovarian cancer: histopathological analysis of survival and local control. A Japanese multi-institutional cooperative and retrospective cohort study. J Neurosurg 137:1006
Xu G, Yang X, Zhang L, Xu M (2022) Prognostic and predictive markers of limited (1–4) brain metastases in patients with lung adenocarcinoma after stereotactic radiosurgery: a retrospective analysis. World Neurosurg 164:e671–e680
Lopes M, Carvalho B, Vaz R, Linhares P (2018) Influence of neutrophil-lymphocyte ratio in prognosis of glioblastoma multiforme. J Neurooncol 136(1):173–180
Koh CH, Bhoo-Pathy N, Ng KL, Jabir RS, Tan GH, See MH et al (2015) Utility of pre-treatment neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as prognostic factors in breast cancer. Br J Cancer 113(1):150–158
Kim JH, Lee JY, Kim HK, Lee JW, Jung SG, Jung K et al (2017) Prognostic significance of the neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with stage III and IV colorectal cancer. World J Gastroenterol 23(3):505–515
Cannon NA, Meyer J, Iyengar P, Ahn C, Westover KD, Choy H et al (2015) Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non-small-cell lung cancer. J Thorac Oncol 10(2):280–285
Conteduca V, Crabb SJ, Jones RJ, Caffo O, Elliott T, Scarpi E et al (2016) Persistent neutrophil to lymphocyte ratio >3 during treatment with enzalutamide and clinical outcome in patients with castration-resistant prostate cancer. PLoS ONE 11(7):e0158952
Kim TW, Lee JH, Shim KH, Choo SH, Choi JB, Ahn HS et al (2019) Prognostic significance of preoperative and follow-up neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with non-metastatic clear cell renal cell carcinoma. Investig Clin Urol 60(1):14–20
Diem S, Schmid S, Krapf M, Flatz L, Born D, Jochum W et al (2017) Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer 111:176–181
Mitsuya K, Nakasu Y, Kurakane T, Hayashi N, Harada H, Nozaki K (2017) Elevated preoperative neutrophil-to-lymphocyte ratio as a predictor of worse survival after resection in patients with brain metastasis. J Neurosurg 127(2):433–437
Murovic J, Ding V, Han SS, Adler JR, Chang SD (2017) Impact of CyberKnife radiosurgery on overall survival and various parameters of patients with 1–3 versus ≥ 4 brain metastases. Cureus 9(10):e1798
Graziano V, Grassadonia A, Iezzi L, Vici P, Pizzuti L, Barba M et al (2019) Combination of peripheral neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio is predictive of pathological complete response after neoadjuvant chemotherapy in breast cancer patients. Breast 44:33–38
Wang J, Zhou X, He Y, Chen X, Liu N, Ding Z et al (2018) Prognostic role of platelet to lymphocyte ratio in prostate cancer: a meta-analysis. Medicine (Baltimore) 97(40):e12504
Tian C, Song W, Tian X, Sun Y (2018) Prognostic significance of platelet-to-lymphocyte ratio in patients with ovarian cancer: a meta-analysis. Eur J Clin Invest 48(5):e12917
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–47
Lin NU, Lee EQ, Aoyama H, Barani IJ, Barboriak DP, Baumert BG et al (2015) Response assessment criteria for brain metastases: proposal from the RANO group. Lancet Oncol 16(6):e270–e278
Viani GA, Gouveia AG, Louie AV, Moraes FY (2021) Stereotactic radiosurgery for brain metastases from small cell lung cancer without prior whole-brain radiotherapy: a meta-analysis. Radiother Oncol 162:45–51
Tamari K, Suzuki O, Hashimoto N, Kagawa N, Fujiwara M, Sumida I et al (2015) Treatment outcomes using CyberKnife for brain metastases from lung cancer. J Radiat Res 56(1):151–158
Yamamoto M, Serizawa T, Sato Y, Higuchi Y, Kasuya H, Barfod BE (2020) Stereotactic radiosurgery for brain metastases: a retrospective cohort study comparing treatment results between two lung cancer patient age groups, 75 years or older vs 65–74 years. Lung Cancer 149:103–112
Wilson TG, Robinson T, MacFarlane C, Spencer T, Herbert C, Wade L et al (2020) Treating brain metastases from breast cancer: outcomes after stereotactic radiosurgery. Clin Oncol (R Coll Radiol) 32(6):390–396
Hall MD, McGee JL, McGee MC, Hall KA, Neils DM, Klopfenstein JD et al (2014) Cost-effectiveness of stereotactic radiosurgery with and without whole-brain radiotherapy for the treatment of newly diagnosed brain metastases. J Neurosurg 121(Suppl):84–90
Pope WB, Sayre J, Perlina A, Villablanca JP, Mischel PS, Cloughesy TF (2005) MR imaging correlates of survival in patients with high-grade gliomas. AJNR Am J Neuroradiol 26(10):2466–2474
Schoenegger K, Oberndorfer S, Wuschitz B, Struhal W, Hainfellner J, Prayer D et al (2009) Peritumoral edema on MRI at initial diagnosis: an independent prognostic factor for glioblastoma? Eur J Neurol 16(7):874–878
Spanberger T, Berghoff AS, Dinhof C, Ilhan-Mutlu A, Magerle M, Hutterer M et al (2013) Extent of peritumoral brain edema correlates with prognosis, tumoral growth pattern, HIF1a expression and angiogenic activity in patients with single brain metastases. Clin Exp Metastasis 30(4):357–368
Nardone V, Nanni S, Pastina P, Vinciguerra C, Cerase A, Correale P et al (2019) Role of perilesional edema and tumor volume in the prognosis of non-small cell lung cancer (NSCLC) undergoing radiosurgery (SRS) for brain metastases. Strahlenther Onkol 195(8):734–744
Tini P, Nardone V, Pastina P, Battaglia G, Vinciguerra C, Carfagno T et al (2017) Perilesional edema in brain metastasis from non-small cell lung cancer (NSCLC) as predictor of response to radiosurgery (SRS). Neurol Sci 38(6):975–982
Kerschbaumer J, Bauer M, Popovscaia M, Grams AE, Thome C, Freyschlag CF (2017) Correlation of tumor and peritumoral edema volumes with survival in patients with cerebral metastases. Anticancer Res 37(2):871–875
Calluaud G, Terrier LM, Mathon B, Destrieux C, Velut S, Francois P et al (2019) Peritumoral edema/tumor volume ratio: a strong survival predictor for posterior fossa metastases. Neurosurgery 85(1):117–125
Vogelbaum MA, Brown PD, Messersmith H, Brastianos PK, Burri S, Cahill D et al (2022) Treatment for brain metastases: ASCO-SNO-ASTRO guideline. J Clin Oncol 40(5):492–516
Tian BW, Yang YF, Yang CC, Yan LJ, Ding ZN, Liu H et al (2022) Systemic immune-inflammation index predicts prognosis of cancer immunotherapy: systemic review and meta-analysis. Immunotherapy 14(18):1481–1496
Dougan M, Luoma AM, Dougan SK, Wucherpfennig KW (2021) Understanding and treating the inflammatory adverse events of cancer immunotherapy. Cell 184(6):1575–1588
Chen L, Douglass J, Kleinberg L, Ye X, Marciscano AE, Forde PM et al (2018) Concurrent immune checkpoint inhibitors and stereotactic radiosurgery for brain metastases in non-small cell lung cancer, melanoma, and renal cell carcinoma. Int J Radiat Oncol Biol Phys 100(4):916–925
Deng H, Xiong B, Gao Y, Yang W, Wang Wei (2023) Stereotactic radiosurgery combined with immune checkpoint inhibitors for brain metastasis: a systematic review and meta-analysis. Asian J Surg 46(5):1917–1923. https://doi.org/10.1016/j.asjsur.2022.09.080
Li B, Zhou P, Liu Y, Wei H, Yang X, Chen T et al (2018) Platelet-to-lymphocyte ratio in advanced cancer: review and meta-analysis. Clin Chim Acta 483:48–56
Wang G, Lu X, Dey P, Deng P, Wu CC, Jiang S et al (2016) Targeting YAP-dependent MDSC infiltration impairs tumor progression. Cancer Discov 6(1):80–95
Swierczak A, Mouchemore KA, Hamilton JA, Anderson RL (2015) Neutrophils: important contributors to tumor progression and metastasis. Cancer Metastasis Rev 34(4):735–751
Coffelt SB, Wellenstein MD, de Visser KE (2016) Neutrophils in cancer: neutral no more. Nat Rev Cancer 16(7):431–446
Ou Q, Cheng J, Zhang L, Wang H, Wang W, Ma Y (2017) The prognostic value of pretreatment neutrophil-to-lymphocyte ratio in breast cancer: deleterious or advantageous? Tumour Biol 39(6):1010428317706214
Bald T, Quast T, Landsberg J, Rogava M, Glodde N, Lopez-Ramos D et al (2014) Ultraviolet-radiation-induced inflammation promotes angiotropism and metastasis in melanoma. Nature 507(7490):109–113
Bodogai M, Moritoh K, Lee-Chang C, Hollander CM, Sherman-Baust CA, Wersto RP et al (2015) Immunosuppressive and prometastatic functions of myeloid-derived suppressive cells rely upon education from tumor-associated B cells. Cancer Res 75(17):3456–3465
Yamamoto T, Kawada K, Obama K (2021) Inflammation-related biomarkers for the prediction of prognosis in colorectal cancer patients. Int J Mol Sci 22(15):8002
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
YH: design of study, drafting; TT and JR: collecting data and design of study; GL: providing substantial conception and suggestions. All authors gave final approval for submission of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Ethical approval
This retrospective analysis of patient data was approved by the local ethics committee ([2022]438).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hao, Y., Tang, T., Ren, J. et al. Prognostic analysis of stereotactic radiosurgery for brain metastases: a single-center retrospective study. Radiol med 128, 1271–1283 (2023). https://doi.org/10.1007/s11547-023-01698-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01698-3