Abstract
Background
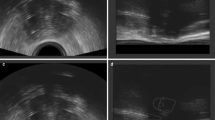
Three-dimensional (3D) imaging has an important role in brachytherapy and the treatment of cervical cancer. The main imaging methods used in the cervical cancer brachytherapy include magnetic resonance imaging (MRI), computer tomography (CT), ultrasound (US), and positron emission tomography (PET). However, single-imaging methods have certain limitations compared to multi-imaging. The application of multi-imaging can make up for the shortcomings and provide a more suitable imaging selection for brachytherapy.
Purpose
This review details the situation and scope of existing multi-imaging combination methods in cervical cancer brachytherapy and provides a reference for medical institutions.
Materials and methods
Searched the literature related to application of three-dimensional multi-imaging combination in brachytherapy of cervical cancer in PubMed/Medline and Web of Science electronic databases. Summarized the existing combined imaging methods and the application of each method in cervical cancer brachytherapy.
Conclusion
The current imaging combination methods mainly include MRI/CT, US/CT, MRI/US, and MRI/PET. The combination of two imaging tools can be used for applicator implantation guidance, applicator reconstruction, target and organs at risk (OAR) contouring, dose optimization, prognosis evaluation, etc., which provides a more suitable imaging choice for brachytherapy.
Similar content being viewed by others
Availability of data and materials
Not applicable.
Code availability
Not applicable.
Abbreviations
- 3D:
-
Three-dimensional
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computer tomography
- US:
-
Ultrasound
- PET:
-
Positron emission tomography
- OAR:
-
Organs at risk
- LC:
-
Local control
- 2D:
-
Two-dimensional
- CTV:
-
Clinical target volume
- GTV:
-
Gross tumor volume
- GEC-ESTRO:
-
Européen de Curiethérapie-European Society for Radiotherapy and Oncology
- 4D:
-
Four-dimensional
- HR-CTV:
-
High-risk clinical target volume
- 3D-US:
-
Three-dimensional ultrasound
- PET-CT:
-
Positron emission tomography-computed tomography
- CR:
-
Complete response
- DIR:
-
Deformable image registration
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- DIR:
-
Deformable image registration
- DVH:
-
Dose volume histograms
- TAUS:
-
Transabdominal ultrasound
- TRUS:
-
Transrectal ultrasound
- TVUS:
-
Transvaginal ultrasound
- TRACE:
-
Trans cervical endosonography
- COV:
-
Coefficient of variation
- CI:
-
Consistency index
- FFS:
-
Failure-free survival
- CSS:
-
Cancer-specific survival
- T2w MRI:
-
T2-weighted MRI
- FDG-PET:
-
Fluorodeoxyglucose PET
- DCE-MRI:
-
Dynamic contrast-enhanced MRI
- DW-MRI:
-
Diffusion-weighted MRI
References
Small W Jr, Bacon MA, Bajaj A et al (2017) Cervical cancer: a global health crisis. Cancer 123:2404–2412. https://doi.org/10.1002/cncr.30667
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Koh WJ, Abu-Rustum NR, Bean S et al (2019) Cervical cancer, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 17:64–84. https://doi.org/10.6004/jnccn.2019.0001
Han K, Milosevic M, Fyles A et al (2013) Trends in the utilization of brachytherapy in cervical cancer in the United States. Int J Radiat Oncol Biol Phys 87:111–119. https://doi.org/10.1016/j.ijrobp.2013.05.033
Viswanathan AN, Creutzberg CL, Craighead P et al (2012) International brachytherapy practice patterns: a survey of the Gynecologic Cancer Intergroup (GCIG). Int J Radiat Oncol Biol Phys 82:250–255. https://doi.org/10.1016/j.ijrobp.2010.10.030
Tod MC, Meredith WJ(1938) A dosage system for use in the treatment of cancer of the uterine cervix. Br J Radiol 11:809–824. https://doi.org/10.1259/0007-1285-11-132-809
ICRU Report 38: Dose and volume specification for reporting intracavitary therapy in gynecology. (1985) International Commission on Radiation Units and Measurements,Bethesda, MD, United States
Haie-Meder C, Pötter R, Van Limbergen E et al (2005) Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol 74:235–245. https://doi.org/10.1016/j.radonc.2004.12.015
ICRU Report 89: Prescribing, Recording, and Reporting Brachytherapy for Cancer of the Cervix. (2013) Journal of the ICRU 13:NP. https://doi.org/10.1093/jicru/ndw027
Schmid MP, Nesvacil N, Pötter R et al (2016) Transrectal ultrasound for image-guided adaptive brachytherapy in cervix cancer—an alternative to MRI for target definition? Radiother Oncol 120:467–472. https://doi.org/10.1016/j.radonc.2016.01.021
Hellebust TP (2018) Place of modern imaging in brachytherapy planning. Cancer Radiother 22:326–333. https://doi.org/10.1016/j.canrad.2018.03.005
Polo A (2010) Image fusion techniques in permanent seed implantation. J Contemp Brachytherapy 2:98–106. https://doi.org/10.5114/jcb.2010.16920
Yang X, Rossi PJ, Jani AB et al (2017) Improved prostate delineation in prostate HDR brachytherapy with TRUS-CT deformable registration technology: a pilot study with MRI validation. J Appl Clin Med Phys 18:202–210. https://doi.org/10.1002/acm2.12040
Peach MS, Trifiletti DM, Libby B (2016) Systematic review of focal prostate brachytherapy and the future implementation of image-guided prostate HDR brachytherapy using MR-ultrasound fusion. Prostate Cancer 2016:4754031. https://doi.org/10.1155/2016/4754031
Bowes D, Crook JM, Araujo C et al (2013) Ultrasound-CT fusion compared with MR-CT fusion for postimplant dosimetry in permanent prostate brachytherapy. Brachytherapy 12:38–43. https://doi.org/10.1016/j.brachy.2012.03.007
Tisseverasinghe S, Marbán M, Crook J et al (2021) Comparison between postoperative TRUS-CT fusion with MRI-CT fusion for postimplant quality assurance in prostate LDR permanent seed brachytherapy. Brachytherapy 20:849–856. https://doi.org/10.1016/j.brachy.2021.03.005
Soror T, Siebert FA, Lancellotta V et al. (2021) Quality Assurance in Modern Gynecological HDR-Brachytherapy (Interventional Radiotherapy): Clinical Considerations and Comments. Cancers (Basel) 13 https://doi.org/10.3390/cancers13040912
Dimopoulos JC, Petrow P, Tanderup K et al (2012) Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (IV): basic principles and parameters for MR imaging within the frame of image based adaptive cervix cancer brachytherapy. Radiother Oncol 103:113–122. https://doi.org/10.1016/j.radonc.2011.12.024
Pötter R, Tanderup K, Schmid MP et al (2021) MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): a multicentre prospective cohort study. Lancet Oncol 22:538–547. https://doi.org/10.1016/s1470-2045(20)30753-1
Russo L, Lancellotta V, Miccò M et al (2022) Magnetic resonance imaging in cervical cancer interventional radiotherapy (brachytherapy): a pictorial essay focused on radiologist management. J Contemp Brachytherapy 14:287–298. https://doi.org/10.5114/jcb.2022.117727
Phan T, Mula-Hussain L, Pavamani S et al (2015) The changing landscape of brachytherapy for cervical cancer: a Canadian practice survey. Curr Oncol 22:356–360. https://doi.org/10.3747/co.22.2562
Grover S, Harkenrider MM, Cho LP et al (2016) Image guided cervical brachytherapy: 2014 Survey of the American Brachytherapy Society. Int J Radiat Oncol Biol Phys 94:598–604. https://doi.org/10.1016/j.ijrobp.2015.11.024
Viswanathan AN, Dimopoulos J, Kirisits C et al (2007) Computed tomography versus magnetic resonance imaging-based contouring in cervical cancer brachytherapy: results of a prospective trial and preliminary guidelines for standardized contours. Int J Radiat Oncol Biol Phys 68:491–498. https://doi.org/10.1016/j.ijrobp.2006.12.021
Hegazy N, Pötter R, Kirisits C et al (2013) High-risk clinical target volume delineation in CT-guided cervical cancer brachytherapy: impact of information from FIGO stage with or without systematic inclusion of 3D documentation of clinical gynecological examination. Acta Oncol 52:1345–1352. https://doi.org/10.3109/0284186x.2013.813068
Mitchell DG, Snyder B, Coakley F et al (2006) Early invasive cervical cancer: tumor delineation by magnetic resonance imaging, computed tomography, and clinical examination, verified by pathologic results, in the ACRIN 6651/GOG 183 Intergroup Study. J Clin Oncol 24:5687–5694. https://doi.org/10.1200/jco.2006.07.4799
Eskander RN, Scanderbeg D, Saenz CC et al (2010) Comparison of computed tomography and magnetic resonance imaging in cervical cancer brachytherapy target and normal tissue contouring. Int J Gynecol Cancer 20:47–53. https://doi.org/10.1111/IGC.0b013e3181c4a627
Iwai Y, Nemoto MW, Horikoshi T et al (2020) Comparison of CT-based and MRI-based high-risk clinical target volumes in image guided-brachytherapy for cervical cancer, referencing recommendations from the Japanese Radiation Oncology Study Group (JROSG) and consensus statement guidelines from the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC ESTRO). Jpn J Radiol 38:899–905. https://doi.org/10.1007/s11604-020-00980-y
Schmid MP, Pötter R, Brader P et al (2013) Feasibility of transrectal ultrasonography for assessment of cervical cancer. Strahlenther Onkol 189:123–128. https://doi.org/10.1007/s00066-012-0258-1
Fischerova D, Cibula D, Stenhova H et al (2008) Transrectal ultrasound and magnetic resonance imaging in staging of early cervical cancer. Int J Gynecol Cancer 18:766–772. https://doi.org/10.1111/j.1525-1438.2007.01072.x
Testa AC, Ludovisi M, Manfredi R et al (2009) Transvaginal ultrasonography and magnetic resonance imaging for assessment of presence, size and extent of invasive cervical cancer. Ultrasound Obstet Gynecol 34:335–344. https://doi.org/10.1002/uog.7325
Gong Y, Wang Q, Dong L et al (2017) Different imaging techniques for the detection of pelvic lymph nodes metastasis from gynecological malignancies: a systematic review and meta-analysis. Oncotarget 8:14107–14125. https://doi.org/10.18632/oncotarget.12959
Van Dyk S, Khaw P, Lin MY et al (2021) Ultrasound-guided brachytherapy for cervix cancer. Clin Oncol (R Coll Radiol) 33:e403–e411. https://doi.org/10.1016/j.clon.2021.02.011
Sapienza LG, Jhingran A, Kollmeier MA et al (2018) Decrease in uterine perforations with ultrasound image-guided applicator insertion in intracavitary brachytherapy for cervical cancer: a systematic review and meta-analysis. Gynecol Oncol 151:573–578. https://doi.org/10.1016/j.ygyno.2018.10.011
Akbas T, Ugurluer G, Acil M et al (2018) Intraoperative sonographic guidance for intracavitary brachytherapy of cervical cancer. J Clin Ultrasound 46:8–13. https://doi.org/10.1002/jcu.22510
Van Dyk S, Schneider M, Kondalsamy-Chennakesavan S et al (2015) Ultrasound use in gynecologic brachytherapy: time to focus the beam. Brachytherapy 14:390–400. https://doi.org/10.1016/j.brachy.2014.12.001
Kalash R, Glaser SM, Rangaswamy B et al (2018) Use of functional magnetic resonance imaging in cervical cancer patients with incomplete response on positron emission tomography/computed tomography after image-based high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys 102:1008–1013. https://doi.org/10.1016/j.ijrobp.2018.01.092
Kim N, Park W, Cho WK et al (2022) Clinical outcomes after positron emission tomography/computed tomography-based image-guided brachytherapy for cervical cancer. Asia Pac J Clin Oncol. https://doi.org/10.1111/ajco.13758
Han S, Kim H, Kim YJ et al (2018) Prognostic value of volume-based metabolic parameters of (18)F-FDG PET/CT in uterine cervical cancer: a systematic review and meta-analysis. AJR Am J Roentgenol 211:1112–1121. https://doi.org/10.2214/ajr.18.19734
Chopra S, Engineer R, Shah S et al (2020) MRI- and PET-guided interstitial brachytherapy for postsurgical vaginal recurrences of cervical cancer: results of phase II study. Int J Radiat Oncol Biol Phys 106:310–319. https://doi.org/10.1016/j.ijrobp.2019.10.037
Min LA, Ackermans LL, Nowee ME et al (2020) Pre-treatment prediction of early response to chemoradiotherapy by quantitative analysis of baseline staging FDG-PET/CT and MRI in locally advanced cervical cancer. Acta Radiol:284185120943046. https://doi.org/10.1177/0284185120943046
Kim N, Park W, Cho WK et al (2020) Early metabolic response assessed using 18F-FDG-PET/CT for image-guided intracavitary brachytherapy can better predict treatment outcomes in patients with cervical cancer. Cancer Res Treat. https://doi.org/10.4143/crt.2020.1251
Lin LL, Mutic S, Low DA et al (2007) Adaptive brachytherapy treatment planning for cervical cancer using FDG-PET. Int J Radiat Oncol Biol Phys 67:91–96. https://doi.org/10.1016/j.ijrobp.2006.08.017
Dutta S, Nguyen NP, Vock J et al (2015) Image-guided radiotherapy and -brachytherapy for cervical cancer. Front Oncol 5:64. https://doi.org/10.3389/fonc.2015.00064
Kidd E, Grigsby P (2011) The use of positron emission tomographic imaging for image-guided therapy. In: Gynecologic radiation therapy. Springer, Cham, pp 41–48
Oh D, Huh SJ, Park W et al (2016) Clinical outcomes in cervical cancer patients treated by FDG-PET/CT-based 3-dimensional planning for the first brachytherapy session. Medicine (Baltimore) 95:e3895. https://doi.org/10.1097/md.0000000000003895
Nam H, Huh SJ, Ju SG et al (2012) 18F-fluorodeoxyglucose positron emisson tomography/computed tomography guided conformal brachytherapy for cervical cancer. Int J Radiat Oncol Biol Phys 84:e29-34. https://doi.org/10.1016/j.ijrobp.2012.02.055
Wang X, Fan L, Yan W et al (2020) Comparison of accuracy and long-term prognosis between computed tomography-based and magnetic resonance imaging-based brachytherapy for cervical cancer: a meta-analysis. J Med Imaging Radiat Oncol 64:151–162. https://doi.org/10.1111/1754-9485.12984
Tuntipumiamorn L, Lohasammakul S, Dankulchai P et al (2018) Comparison of impact of target delineation of computed tomography- and magnetic resonance imaging-guided brachytherapy on dose distribution in cervical cancer. J Contemp Brachytherapy 10:418–424. https://doi.org/10.5114/jcb.2018.78993
Koulis TA, Doll CM, Brown D et al (2016) Implementation and validation of a combined MRI-CT-based cervical cancer brachytherapy program using existing infrastructure. Brachytherapy 15:319–326. https://doi.org/10.1016/j.brachy.2016.01.005
Wakatsuki M, Ohno T, Yoshida D et al (2011) Intracavitary combined with CT-guided interstitial brachytherapy for locally advanced uterine cervical cancer: introduction of the technique and a case presentation. J Radiat Res 52:54–58. https://doi.org/10.1269/jrr.10091
Kang HC, Shin KH, Park SY et al (2010) 3D CT-based high-dose-rate brachytherapy for cervical cancer: clinical impact on late rectal bleeding and local control. Radiother Oncol 97:507–513. https://doi.org/10.1016/j.radonc.2010.10.002
Beriwal S, Kim H, Coon D et al (2009) Single magnetic resonance imaging vs magnetic resonance imaging/computed tomography planning in cervical cancer brachytherapy. Clin Oncol (R Coll Radiol) 21:483–487. https://doi.org/10.1016/j.clon.2009.03.007
Beriwal S, Kannan N, Kim H et al (2011) Three-dimensional high dose rate intracavitary image-guided brachytherapy for the treatment of cervical cancer using a hybrid magnetic resonance imaging/computed tomography approach: feasibility and early results. Clin Oncol (R Coll Radiol) 23:685–690. https://doi.org/10.1016/j.clon.2011.08.007
Dolezel M, Odrazka K, Vanasek J et al (2011) MRI-based pre-planning in patients with cervical cancer treated with three-dimensional brachytherapy. Br J Radiol 84:850–856. https://doi.org/10.1259/bjr/75446993
Dolezel M, Odrazka K, Zizka J et al (2012) MRI-based preplanning using CT and MRI data fusion in patients with cervical cancer treated with 3D-based brachytherapy: feasibility and accuracy study. Int J Radiat Oncol Biol Phys 84:146–152. https://doi.org/10.1016/j.ijrobp.2011.11.003
Takagawa Y, Izumi S, Kita M (2022) Laminaria tent insertion in preplanning MRI for CT-based cervical cancer brachytherapy. Brachytherapy 21:170–176. https://doi.org/10.1016/j.brachy.2021.10.001
Nesvacil N, Pötter R, Sturdza A et al (2013) Adaptive image guided brachytherapy for cervical cancer: a combined MRI-/CT-planning technique with MRI only at first fraction. Radiother Oncol 107:75–81. https://doi.org/10.1016/j.radonc.2012.09.005
Choong ES, Bownes P, Musunuru HB et al (2016) Hybrid (CT/MRI based) vs. MRI only based image-guided brachytherapy in cervical cancer: Dosimetry comparisons and clinical outcome. Brachytherapy 15:40–48. https://doi.org/10.1016/j.brachy.2015.09.002
Pötter R, Georg P, Dimopoulos JC et al (2011) Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol 100:116–123. https://doi.org/10.1016/j.radonc.2011.07.012
Berger D, Pötter R, Dimopoulos JCA et al (2010) New Vienna applicator design for distal parametrial disease in cervical cancer. Brachytherapy 9:S51–S52. https://doi.org/10.1016/j.brachy.2010.02.071
Corriher TJ, Dutta SW, Alonso CE et al (2020) Comparison of initial computed tomography-based target delineation and subsequent magnetic resonance imaging-based target delineation for cervical cancer brachytherapy. J Contemp Brachytherapy 12:279–282. https://doi.org/10.5114/jcb.2020.96871
Trifiletti DM, Libby B, Feuerlein S et al (2015) Implementing MRI-based target delineation for cervical cancer treatment within a rapid workflow environment for image-guided brachytherapy: a practical approach for centers without in-room MRI. Brachytherapy 14:905–909. https://doi.org/10.1016/j.brachy.2015.07.005
Dutta SW, Trifiletti DM, Pugh KJ et al (2018) Integration of MRI target delineation into rapid workflow cervical cancer brachytherapy: Impact on clinical outcomes. J Med Imaging Radiat Oncol 62:716–725. https://doi.org/10.1111/1754-9485.12763
Tait LM, Hoffman D, Benedict S et al (2016) The use of MRI deformable image registration for CT-based brachytherapy in locally advanced cervical cancer. Brachytherapy 15:333–340. https://doi.org/10.1016/j.brachy.2016.01.002
Dyer BA, Yuan Z, Qiu J et al (2019) Factors associated with deformation accuracy and modes of failure for MRI-optimized cervical brachytherapy using deformable image registration. Brachytherapy 18:378–386. https://doi.org/10.1016/j.brachy.2019.01.001
Dyer BA, Yuan Z, Qiu J et al (2020) Clinical feasibility of MR-assisted CT-based cervical brachytherapy using MR-to-CT deformable image registration. Brachytherapy 19:447–456. https://doi.org/10.1016/j.brachy.2020.03.001
Nemoto MW, Iwai Y, Togasaki G et al (2017) Preliminary results of a new workflow for MRI/CT-based image-guided brachytherapy in cervical carcinoma. Jpn J Radiol 35:760–765. https://doi.org/10.1007/s11604-017-0690-3
Cooper R, Brearley E, Hurmuz P et al (2014) Assessment of uterus position as a surrogate for high-risk clinical target volume with respect to the applicator position for multiple fractions of brachytherapy in cervical cancer. Arch Gynecol Obstet 290:1201–1205. https://doi.org/10.1007/s00404-014-3350-1
Rogowski P, Rottler M, Walter F et al (2022) Clinical outcome of combined intracavitary/interstitial brachytherapy using a hybrid applicator in locally advanced cervical cancer. Gynecol Oncol 166:576–581. https://doi.org/10.1016/j.ygyno.2022.06.019
Wu PY, Wong TPW, Yip YYC et al (2019) MRI-guided adaptive brachytherapy for locally advanced cervix cancer: treatment outcomes from a single institution in Hong Kong. Brachytherapy 18:171–179. https://doi.org/10.1016/j.brachy.2018.11.007
Lang S, Nesvacil N, Kirisits C et al (2013) Uncertainty analysis for 3D image-based cervix cancer brachytherapy by repetitive MR imaging: assessment of DVH-variations between two HDR fractions within one applicator insertion and their clinical relevance. Radiother Oncol 107:26–31. https://doi.org/10.1016/j.radonc.2013.02.015
Pötter R, Haie-Meder C, Van Limbergen E et al (2006) Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol 78:67–77. https://doi.org/10.1016/j.radonc.2005.11.014
Haack S, Nielsen SK, Lindegaard JC et al (2009) Applicator reconstruction in MRI 3D image-based dose planning of brachytherapy for cervical cancer. Radiother Oncol 91:187–193. https://doi.org/10.1016/j.radonc.2008.09.002
Hellebust TP, Kirisits C, Berger D et al (2010) Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group: considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother Oncol 96:153–160. https://doi.org/10.1016/j.radonc.2010.06.004
Krempien RC, Daeuber S, Hensley FW et al (2003) Image fusion of CT and MRI data enables improved target volume definition in 3D-brachytherapy treatment planning. Brachytherapy 2:164–171. https://doi.org/10.1016/s1538-4721(03)00133-8
Datta NR, Kumar S, Das KJ et al (2001) Variations of intracavitary applicator geometry during multiple HDR brachytherapy insertions in carcinoma cervix and its influence on reporting as per ICRU report 38. Radiother Oncol 60:15–24. https://doi.org/10.1016/s0167-8140(01)00352-8
Tanderup K, Hellebust TP, Lang S et al (2008) Consequences of random and systematic reconstruction uncertainties in 3D image based brachytherapy in cervical cancer. Radiother Oncol 89:156–163. https://doi.org/10.1016/j.radonc.2008.06.010
Harkenrider MM, Patel R, Surucu M et al (2018) Can MRI-only replace MRI-CT planning with a titanium tandem and ovoid applicator? Brachytherapy 17:747–752. https://doi.org/10.1016/j.brachy.2018.05.010
Van Dyk S, Kondalsamy-Chennakesavan S, Schneider M et al (2014) Comparison of measurements of the uterus and cervix obtained by magnetic resonance and transabdominal ultrasound imaging to identify the brachytherapy target in patients with cervix cancer. Int J Radiat Oncol Biol Phys 88:860–865. https://doi.org/10.1016/j.ijrobp.2013.12.004
Van Dyk S, Kondalsamy-Chennakesavan S, Schneider M et al (2015) Assessing changes to the brachytherapy target for cervical cancer using a single MRI and serial ultrasound. Brachytherapy 14:889–897. https://doi.org/10.1016/j.brachy.2015.04.011
Petric P, Kirisits C (2016) Potential role of TRAns Cervical Endosonography (TRACE) in brachytherapy of cervical cancer: proof of concept. J Contemp Brachytherapy 8:215–220. https://doi.org/10.5114/jcb.2016.60502
Mendez LC, Morton GC (2018) High dose-rate brachytherapy in the treatment of prostate cancer. Transl Androl Urol 7:357–370. https://doi.org/10.21037/tau.2017.12.08
Lin Y, Cheng G, Shi D et al (2020) Clinical application of ultrasound guidance for parametrial treatment of advanced cervical cancer. J Ultrasound Med 39:1087–1095. https://doi.org/10.1002/jum.15189
Yan XJ, Yang Y, Chen X et al. (2022) A new technique for performing interstitial implants for gynecologic malignancies using transvaginal ultrasound guidance. Front Oncol 12:858620. https://doi.org/10.3389/fonc.2022.858620
Nesvacil N, Schmid MP, Pötter R et al (2016) Combining transrectal ultrasound and CT for image-guided adaptive brachytherapy of cervical cancer: proof of concept. Brachytherapy 15:839–844. https://doi.org/10.1016/j.brachy.2016.08.009
Smet S, Nesvacil N, Knoth J et al (2020) Hybrid TRUS/CT with optical tracking for target delineation in image-guided adaptive brachytherapy for cervical cancer. Strahlenther Onkol 196:983–992. https://doi.org/10.1007/s00066-020-01656-2
Mahantshetty U, Naga ChP, Khadanga CR et al (2018) A Prospective comparison of computed tomography with transrectal ultrasonography assistance and magnetic resonance imaging-based target-volume definition during image guided adaptive brachytherapy for cervical cancers. Int J Radiat Oncol Biol Phys 102:1448–1456. https://doi.org/10.1016/j.ijrobp.2018.05.080
Swamidas J, Jain J, Nesvacil N et al (2022) Dosimetric impact of target definition in brachytherapy for cervical cancer—computed tomography and trans rectal ultrasound versus magnetic resonance imaging. Phys Imaging Radiat Oncol 21:126–133. https://doi.org/10.1016/j.phro.2022.02.002
St-Amant P, Foster W, Froment MA et al (2017) Use of 3D transabdominal ultrasound imaging for treatment planning in cervical cancer brachytherapy: comparison to magnetic resonance and computed tomography. Brachytherapy 16:847–854. https://doi.org/10.1016/j.brachy.2017.03.006
Shimizu Y, Murakami N, Chiba T et al. (2021) High-dose-rate interstitial brachytherapy for deeply situated gynecologic tumors guided by combination of transrectal and transabdominal ultrasonography: a technical note. Front Oncol 11:808721. https://doi.org/10.3389/fonc.2021.808721
Rodgers JR, Mendez LC, Hoover DA et al (2021) Feasibility of fusing three-dimensional transabdominal and transrectal ultrasound images for comprehensive intraoperative visualization of gynecologic brachytherapy applicators. Med Phys 48:5611–5623. https://doi.org/10.1002/mp.15175
Zeng J, Liu Z, Jiang S et al (2021) Verification of guiding needle placement by registered ultrasound image during combined intracavitary/interstitial gynecologic brachytherapy. Cancer Manag Res 13:1917–1928. https://doi.org/10.2147/cmar.S294498
Federico M, Hernandez-Socorro CR, Ribeiro I et al (2019) Prospective intra/inter-observer evaluation of pre-brachytherapy cervical cancer tumor width measured in TRUS and MR imaging. Radiat Oncol 14:173. https://doi.org/10.1186/s13014-019-1352-7
Van Dyk S, Narayan K, Bernshaw D et al (2016) Clinical outcomes from an innovative protocol using serial ultrasound imaging and a single MR image to guide brachytherapy for locally advanced cervix cancer. Brachytherapy 15:817–824. https://doi.org/10.1016/j.brachy.2016.07.008
Tharavichitkul E, Tippanya D, Jayavasti R et al (2015) Two-year results of transabdominal ultrasound-guided brachytherapy for cervical cancer. Brachytherapy 14:238–244. https://doi.org/10.1016/j.brachy.2014.11.001
Pu G, Jiang S, Yang Z et al (2022) A novel ultrasound probe calibration method for multimodal image guidance of needle placement in cervical cancer brachytherapy. Phys Med 100:81–89. https://doi.org/10.1016/j.ejmp.2022.06.009
Yang Z, Liu Z, Jiang S et al (2020) Verification of needle guidance accuracy in pelvic phantom using registered ultrasound and MRI images for intracavitary/interstitial gynecologic brachytherapy. J Contemp Brachytherapy 12:147–159. https://doi.org/10.5114/jcb.2020.94583
Petrič P, Hudej R, Rogelj P et al (2013) Uncertainties of target volume delineation in MRI guided adaptive brachytherapy of cervix cancer: a multi-institutional study. Radiother Oncol 107:6–12. https://doi.org/10.1016/j.radonc.2013.01.014
Dyk P, Jiang N, Sun B et al (2014) Cervical gross tumor volume dose predicts local control using magnetic resonance imaging/diffusion-weighted imaging-guided high-dose-rate and positron emission tomography/computed tomography-guided intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys 90:794–801. https://doi.org/10.1016/j.ijrobp.2014.07.039
Tanderup K, Fokdal LU, Sturdza A et al (2016) Effect of tumor dose, volume and overall treatment time on local control after radiochemotherapy including MRI guided brachytherapy of locally advanced cervical cancer. Radiother Oncol 120:441–446. https://doi.org/10.1016/j.radonc.2016.05.014
Ke T, Wang J, Zhang N et al (2022) Dose-effect relationship between dose-volume parameters of residual gross tumor volume and clinical prognosis in MRI-guided adaptive brachytherapy for locally advanced cervical cancer: a single-center retrospective study. Strahlenther Onkol. https://doi.org/10.1007/s00066-022-02000-6
Pötter R, Tanderup K, Kirisits C et al (2018) The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC-ESTRO GYN working group and the EMBRACE studies. Clin Transl Radiat Oncol 9:48–60. https://doi.org/10.1016/j.ctro.2018.01.001
Han K, Croke J, Foltz W et al (2016) A prospective study of DWI, DCE-MRI and FDG PET imaging for target delineation in brachytherapy for cervical cancer. Radiother Oncol 120:519–525. https://doi.org/10.1016/j.radonc.2016.08.002
Funding
This work was partially supported by grants from the National Natural Science Foundation of China [Grant Numbers 82073331, 81703034, 82003208]; Project of Science and Technology Department of Jilin Province (Grant Number 20190303151SF, 20210401138YY, 20230203082SF); Horizontal Project of Jilin University [Grant Numbers 2019YX435, 2019155, 2023YX0056] and the Natural Science Foundation of Jilin Province, China (Grant No.212558JC010284904).
Author information
Authors and Affiliations
Contributions
ZZ wrote original draft, made the tables; NZ carefully read and provided helpful discussions and edited manuscript; GC had the idea for the article, supervised the review and revised the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
Not applicable.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Zhang, N. & Cheng, G. Application of three-dimensional multi-imaging combination in brachytherapy of cervical cancer. Radiol med 128, 588–600 (2023). https://doi.org/10.1007/s11547-023-01632-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01632-7