Abstract
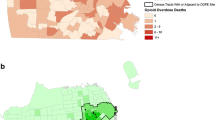
The third wave of the opioid overdose crisis—defined by the proliferation of illicit fentanyl and its analogs—has not only led to record numbers of overdose deaths but also to unprecedented racial inequities in overdose deaths impacting Black Americans. Despite this racialized shift in opioid availability, little research has examined how the spatial epidemiology of opioid overdose death has also shifted. The current study examines the differential geography of OOD by race and time (i.e., pre-fentanyl versus fentanyl era) in St. Louis, Missouri. Data included decedent records from the local medical examiners suspected to involve opioid overdose (N = 4420). Analyses included calculating spatial descriptive analyses and conducting hotspot analyses (i.e., Gettis-Ord Gi*) stratified by race (Black versus White) and time (2011–2015 versus 2016–2021). Results indicated that fentanyl era overdose deaths were more densely clustered than pre-fentanyl era deaths, particularly those among Black decedents. Although hotspots of overdose death were racially distinct pre-fentanyl, they substantially overlapped in the fentanyl era, with both Black and White deaths clustering in predominantly Black neighborhoods. Racial differences were observed in substances involved in cause of death and other overdose characteristics. The third wave of the opioid crisis appears to involve a geographic shift from areas where White individuals live to those where Black individuals live. Findings demonstrate racial differences in the epidemiology of overdose deaths that point to built environment determinants for future examination. Policy interventions targeting high-deprivation communities are needed to reduce the burden of opioid overdose on Black communities.



Similar content being viewed by others
References
Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019;71:183–8. https://doi.org/10.1016/j.drugpo.2019.01.010.
Ahmad FB, Cisewski JA, Rossen LM, Sutton P. Provisional drug overdose death counts. Published online 2022. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed 30 Jan 2023
Furr-Holden D, Milam AJ, Wang L, Sadler R. African Americans now outpace whites in opioid-involved overdose deaths: a comparison of temporal trends from 1999 to 2018. Addiction. 2021;116(3):677–83. https://doi.org/10.1111/add.15233.
Friedman JR, Hansen H. Evaluation of increases in drug overdose mortality rates in the US by race and ethnicity before and during the COVID-19 pandemic. JAMA Psychiatry. 2022;79(4):379–81. https://doi.org/10.1001/jamapsychiatry.2022.0004.
Rossen LM, Khan D, Warner M. Hot spots in mortality from drug poisoning in the United States, 2007–2009. Health Place. 2014;26:14–20. https://doi.org/10.1016/j.healthplace.2013.11.005.
Hernandez A, Branscum AJ, Li J, MacKinnon NJ, Hincapie AL, Cuadros DF. Epidemiological and geospatial profile of the prescription opioid crisis in Ohio, United States. Sci Rep. 2020;10(1):4341. https://doi.org/10.1038/s41598-020-61281-y.
Marotta PL, Hunt T, Gilbert L, Wu E, Goddard-Eckrich D, El-Bassel N. Assessing spatial relationships between prescription drugs, race, and overdose in New York State from 2013 to 2015. J Psychoactive Drugs. 2019;51(4):360–70. https://doi.org/10.1080/02791072.2019.1599472.
Sadler RC, Hippensteel CL, Nelson V, Greene-Moton E, Furr-Holden D. Community-engaged development of a GIS-based healthfulness index to shape health equity solutions. Soc Sci Med. 2019;1982(227):63–75. https://doi.org/10.1016/j.socscimed.2018.07.030.
Visconti AJ, Santos GM, Lemos NP, Burke C, Coffin PO. Opioid overdose deaths in the City and County of San Francisco: prevalence, distribution, and disparities. J Urban Health. 2015;92(4):758–72. https://doi.org/10.1007/s11524-015-9967-y.
Cerdá M, Ransome Y, Keyes KM, et al. Prescription opioid mortality trends in New York City, 1990–2006: examining the emergence of an epidemic. Drug Alcohol Depend. 2013;132(1-2):53–62. https://doi.org/10.1016/j.drugalcdep.2012.12.027.
Modarai F, Mack K, Hicks P, et al. Relationship of opioid prescription sales and overdoses, North Carolina. Drug Alcohol Depend. 2013;132(1-2):81–6. https://doi.org/10.1016/j.drugalcdep.2013.01.006.
Stopka TJ, Amaravadi H, Kaplan AR, et al. Opioid overdose deaths and potentially inappropriate opioid prescribing practices (PIP): a spatial epidemiological study. Int J Drug Policy. 2019;68:37–45. https://doi.org/10.1016/j.drugpo.2019.03.024.
Hembree C, Galea S, Ahern J, et al. The urban built environment and overdose mortality in New York City neighborhoods. Health Place. 2005;11(2):147–56. https://doi.org/10.1016/j.healthplace.2004.02.005.
Nesoff ED, Branas CC, Martins SS. The geographic distribution of fentanyl-involved overdose deaths in Cook County, Illinois. Am J Public Health. 2020;110(1):98–105. https://doi.org/10.2105/AJPH.2019.305368.
Ghose R, Forati AM, Mantsch JR. Impact of the COVID-19 pandemic on opioid overdose deaths: a spatiotemporal analysis. J Urban Health. 2022;99(2):316–27. https://doi.org/10.1007/s11524-022-00610-0.
Forati AM, Ghose R, Mantsch JR. Examining opioid overdose deaths across communities defined by racial composition: a multiscale geographically weighted regression approach. J Urban Health. 2021;98(4):551–62. https://doi.org/10.1007/s11524-021-00554-x.
Rowe C, Santos GM, Vittinghoff E, Wheeler E, Davidson P, Coffin PO. Neighborhood-level and spatial characteristics associated with lay naloxone reversal events and opioid overdose deaths. J Urban Health. 2016;93(1):117–30. https://doi.org/10.1007/s11524-015-0023-8.
Bohnert ASB, Nandi A, Tracy M, et al. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Depend. 2011;113(1):62–8. https://doi.org/10.1016/j.drugalcdep.2010.07.008.
Johnson LT, Shreve T. The ecology of overdose mortality in Philadelphia. Health Place. 2020;66:102430. https://doi.org/10.1016/j.healthplace.2020.102430.
Berke EM, Tanski SE, Demidenko E, Alford-Teaster J, Shi X, Sargent JD. Alcohol retail density and demographic predictors of health disparities: a geographic analysis. Am J Public Health. 2010;100(10):1967–71. https://doi.org/10.2105/AJPH.2009.170464.
Hippensteel CL, Sadler RC, Milam AJ, Nelson V, Debra F-HC. Using zoning as a public health tool to reduce oversaturation of alcohol outlets: an examination of the effects of the new “300 foot rule” on packaged goods stores in a mid-Atlantic city. Prev Sci. 2019;20(6):833–43. https://doi.org/10.1007/s11121-018-0947-9.
Gomes T, Juurlink DN, Mamdani MM, Paterson JM, van den Brink W. Prevalence and characteristics of opioid-related deaths involving alcohol in Ontario, Canada. Drug Alcohol Depend. 2017;179:416–23. https://doi.org/10.1016/j.drugalcdep.2017.07.008.
University of Missouri, St. Louis-Missouri Institute of Mental Health Addiction Science Team, St. Louis City and St. Louis County Medical Examiners. St. Louis City and County drug-involved deaths report 2021. Published online 2020. https://www.mimhaddisci.org/missouri-overdose-data
Benton M. “Just the way things are around here”: racial segregation, critical junctures, and path dependence in Saint Louis. J Urban Hist. 2018;44(6):1113–30. https://doi.org/10.1177/0096144217696988.
Harris KM. Mapping inequality: childhood asthma and environmental injustice, a case study of St. Louis, Missouri. Soc Sci Med. 2019;230:91–110. https://doi.org/10.1016/j.socscimed.2019.03.040.
Goodman, M. S., & Gilbert, K. L. Segregation: divided cities lead to differences in health. Published online 2013. https://forthesakeofall.files.wordpress.com/2013/11/policy-brief-4.pdf. Accessed 30 Jan 2023
Stoecker WV, Bosworth KT, Rottnek F. Missouri’s fentanyl problem: the China connection. Mo Med. 2020;117(4):362–9.
Xun Li & Luc Anselin. rgeoda: R library for spatial data analysis. Published online 2022. https://CRAN.R-project.org/package=rgeoda. Accessed 30 Jan 2023
Wagner J, Neitzke-Spruill L, Donnelly EA, O’Connell DJ, Anderson TL. The current community context of overdose deaths: relations among drug types, drug markets, and socioeconomic neighborhood characteristics. Sociol Forum. 2021;36(4):1005–27. https://doi.org/10.1111/socf.12746.
Donnelly EA, Wagner J, Stenger M, Cortina HG, O’Connell DJ, Anderson TL. Opioids, race, and drug enforcement: exploring local relationships between neighborhood context and Black–White opioid-related possession arrests. Crim Justice Policy Rev. 2021;32(3):219–44. https://doi.org/10.1177/0887403420911415.
Doe-Simkins M, El-Sabawi T, Carroll JJ. Whose concerns? It’s time to adjust the lens of research on police-involved overdose response. Am J Public Health. 2022;112(9):1239–41. https://doi.org/10.2105/AJPH.2022.306988.
Banks DE, Duello A, Paschke M, Grigsby E, Winograd RP. Identifying drivers of increasing opioid overdose deaths among Black individuals: a qualitative model drawing on experience of peers and community health workers. Harm Reduct J. 2023;20(5):1–9. https://doi.org/10.1186/s12954-023-00734-9.
Latimore AD, Bergstein RS. “Caught with a body” yet protected by law? Calling 911 for opioid overdose in the context of the Good Samaritan Law. Int J Drug Policy. 2017;50:82–9. https://doi.org/10.1016/j.drugpo.2017.09.010.
U.S. Census Bureau. QuickFacts: United States; East St. Louis City, Illinois. Published online n.d. Accessed June 18, 2020. https://www.census.gov/quickfacts/fact/table/US,eaststlouiscityillinois/POP010220
Acknowledgments
Research reported in this publication was supported by the National Center for Advancing Translational Sciences (KL2 TR002346; PI: Reeds) to Devin Banks. This content is solely the responsibility of the authors and does not necessarily represent the views of the funder(s).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Banks, D.E., Scroggins, S., Paschke, M.E. et al. Examining Increasing Racial Inequities in Opioid Overdose Deaths: a Spatiotemporal Analysis of Black and White Decedents in St. Louis, Missouri, 2011–2021. J Urban Health 100, 436–446 (2023). https://doi.org/10.1007/s11524-023-00736-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-023-00736-9