Abstract
This paper is one of the outcomes of the 5th International Conference "Controversies in Vitamin D" held in Stresa, Italy from 15 to 18 September 2021 as part of a series of annual meetings which was started in 2017. The scope of these meetings is to discuss controversial issues about vitamin D. Publication of the outcomes of the meeting in international journals allows a wide sharing of the most recent data with the medical and academic community. Vitamin D and malabsorptive gastrointestinal conditions was one of the topics discussed at the meeting and focus of this paper. Participants to the meeting were invited to review available literature on selected issues related to vitamin D and gastrointestinal system and to present their topic to all participants with the aim to initiate a discussion on the main outcomes of which are reported in this document. The presentations were focused on the possible bidirectional relationship between vitamin D and gastrointestinal malabsorptive conditions such as celiac disease, inflammatory bowel diseases (IBDs) and bariatric surgery. In fact, on one hand the impact of these conditions on vitamin D status was examined and on the other hand the possible role of hypovitaminosis D on pathophysiology and clinical course of these conditions was also evaluated. All examined malabsorptive conditions severely impair vitamin D status. Since vitamin D has known positive effects on bone this in turn may contribute to negative skeletal outcomes including reduced bone mineral density, and increased risk of fracture which may be mitigated by vitamin D supplementation. Due to the immune and metabolic extra-skeletal effects there is the possibility that low levels of vitamin D may negatively impact on the underlying gastrointestinal conditions worsening its clinical course or counteracting the effect of treatment. Therefore, vitamin D status assessment and supplementation should be routinely considered in all patients affected by these conditions. This concept is strengthened by the existence of a possible bidirectional relationship through which poor vitamin D status may negatively impact on clinical course of underlying disease. Sufficient elements are available to estimate the desired threshold vitamin D level above which a favourable impact on the skeleton in these conditions may be obtained. On the other hand, ad hoc controlled clinical trials are needed to better define this threshold for obtaining a positive effect of vitamin D supplementation on occurrence and clinical course of malabsorptive gastrointestinal diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The 5th International Conference “Controversies in Vitamin D” was held in Stresa, Italy, 15–18 September 2021 as part of this series that started in 2017 [1,2,3,4,5,6,7,8]. The objective of this conference, which featured international experts and leaders, was to review and discuss controversial topics regarding vitamin D. Besides the well-known benefits of vitamin D on skeletal health, new evidence highlights its role also in multiple conditions not specifically related to the skeleton often referred to as extra-skeletal actions. Examples include diabetes mellitus, obesity, kidney and neurological diseases, malignant disorders and infections including COVID-19 [9, 10]. Additionally, the gastrointestinal tract has been a topic of current interest [4]. During the conference, discrete sessions addressed aspects of vitamin D on aging [8], COVID-19 [11], and the gastrointestinal system. Participants prepared for these sessions by reviewing the available literature on their assigned topic. After each topic was covered by presentations, open sessions enabled full discussion to reach consensus. A separate document was prepared for each component of the conference.
This paper presents topics related to vitamin D and the gastrointestinal system.
2 Background
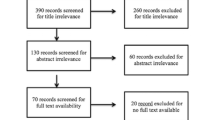
Vitamin D is a requirement for efficient intestinal calcium absorption. Any gastrointestinal disease, as well as any surgical gastrointestinal intervention such as bariatric surgery, can lead to impaired gastrointestinal function. One key consequence, namely vitamin D malabsorption can reduce vitamin D and calcium levels leading to negative consequences on skeletal health [7] (Fig. 1).
The relationship between gastrointestinal diseases and vitamin D is classically considered unidirectional with the gastrointestinal diseases leading to hypovitaminosis D. Emerging evidence, however, has shown that hypovitaminosis D itself can negatively influence the clinical course of the gastrointestinal disease, whether it be disease activity or recurrence [7]. These newer concepts have been advanced because vitamin D receptors, which are highly expressed in intestinal epithelial cells, mediate the pleotropic actions of vitamin D which include immunomodulatory actions. To this end, vitamin D has the potential to regulate gut mucosal immunity, a key pathophysiological aspect of inflammatory bowel diseases (IBDs), such as Crohn’s disease (CsD) and ulcerative colitis (UC). Celiac disease (CD) is also potentially affected by the immunomodulatory actions of vitamin D. Thus, the current concept being advanced in this paper is that there is a bidirectionality to vitamin D and the gastrointestinal tract. Gastrointestinal diseases associated with malabsorption can lead to variable degrees of vitamin D deficiency and its classical consequences on skeletal and extra-skeletal health (Fig. 2). Hypovitaminosis D can also lead to exacerbation or recurrence of diseases of the gastrointestinal tract, particularly in IBDs, and potentially also attenuate the efficacy of bariatric surgery (Fig. 2). This concept helps to underscore the guidelines that place vitamin D adequacy as a cornerstone of therapeutics for the examined gastrointestinal diseases [7].
The respective relative influence of a) Gastrointestinal conditions on hypovitaminosis D occurrence and b) Vitamin D influence on disease’s course in Bariatric Surgery, Celiac Disease and Inflammatory Bowel Diseases. Higher intensity of red corresponds to greater clinical role in the different malabsorptive gastrointestinal conditions
This paper summarizes the evidence for this bidirectional relationship between vitamin D and the gastrointestinal tract as summarized by the deliberations at this international conference.
3 Calcium intestinal absorption in healthy individuals
The intestine is the first and best studied target for active vitamin D, 1.25-dihydroxyvitamin D [1.25(OH)2D]. The ratio of transcellular to paracellular calcium absorption directly follows from the levels of transcription of various genes, including those best known to be under regulation by 1.25(OH)2D, and in particular Trpv6, S100g (aka calbindin 9 k), Atp2b1 (aka Pmca1b), highly expressed by both the duodenum and cecum [12,13,14,15,16]. The vitamin D receptor (VDR) and those genes involved in the paracellular pathway such as claudins 2, 12, 15 are more widely distributed throughout the intestine [17,18,19]. Moreover, the contribution of transcellular vs paracellular pathways likewise varies, and age modifies both this balance and the degree to which 1.25(OH)2D regulates overall absorption [20]. For example, in rodents prior to weaning, intestinal calcium absorption is not dependent on vitamin D and relies primarily on the paracellular pathway.
Another factor that contributes to calcium absorption is transit time. Although the efficiency of calcium absorption is highest in the duodenum, the transit time is short, around 3 min. Transit time is longest, 2 h or so, in the ileum which is the major site of calcium absorption (65–88% in adult rodents) while having the lowest ratio of transcellular to paracellular absorption [21]. Similar studies in human subjects also demonstrate that the ileum is the main site for calcium absorption [13].
The previous paradigm for transcellular calcium transport was incomplete, since blocking or deleting the proteins known to be involved in this process, such as either or both Trpv6 and CaBP9k, as well as myosin 1A, do not completely block it [22,23,24]. Other calcium binding proteins in the cytoplasm have been suggested, including CaM, parvalbumin, and sorcin (soluble-resistant calcium binding protein), but none of these has been carefully studied. On the other hand, deletion of Pmca1b does reduce calcium absorption and blocks 1.25(OH)2D action, resulting in reduction in growth and bone mineralization [15].
With regard to paracellular absorption, solvent drag plays a large part in moving calcium across the tight junctions between the epithelial cells. Solvent flow follows the osmotic gradient which is maintained distal to the tight junction by the Na/K ATPase and sodium glucose cotransporter of the basolateral membrane which may be stimulated by 1.25(OH)2D, while the claudins and occludins contribute to charge selectivity [20, 21]. Claudin 2, 12, 15 are negatively charged and enable cations such as sodium and calcium to pass [17,18,19]. The expression of claudins 2 and 12 are stimulated by 1.25(OH)2D [17,18,19].
Another factor that may help regulate calcium absorption is the calcium sensing receptor (CaSR), expressed on the membranes of the small intestine cell [25, 26]. Stimulation of the CaSR pharmacologically blocks 1.25(OH)2D-induced calcium absorption. In preliminary experiments with an intestinal specific deletion of CaSR, calcium absorption at higher calcium loads was increased. Although 1.25(OH)2D induces the CaSR in other tissues, this has not been tested in the intestine. Other regulators include estrogen, prolactin, growth hormone, and IGF1, but these remain little explored [27,28,29]. A number of other dietary (such as oxalate and phytate) or hormonal (e.g. estrogens) can interfere with calcium absorption [30].
4 Vitamin D and gut microbiome
Several studies showed that gut microbiota regulate intestinal vitamin D metabolism and circulating vitamin D levels were affected by probiotic supplements [31]. A study evaluating the association between the vitamin D metabolites and the gut microbiome indicated that serum 1.25(OH)2D level explained 5% of variance in α-diversity and, 2% of variance in β-diversity of intestinal microbiota. Higher levels of 1.25(OH)2D and higher hormone-to-prohormone [1.25(OH)2D/25(OH)D] activation ratios, but not 25(OH)D itself, were more likely to possess butyrate-producing bacteria that are associated with heathier gut microbiota [31]. The association of active vitamin D metabolites with more favorable gut microbial diversity provide promising targets for intervention [31]. Schaffler et al. reported that vitamin D3 supplementation altered the gut microbiota composition only in CsD in remission, but not in vitamin D deficient healthy controls, [32] suggesting that administration of vitamin D has potential as an adjuvant therapy for CsD patients. In another study, increased serum 25(OH)D was associated with increased beneficial bacteria and decreased pathogenic bacteria. There was a dose-dependent increase in bacteria linked to decreased IBDs activity after vitamin D3 supplementation [33]. Further experimental data demonstrated that probiotics stimulate VDR expression and activity. Besides the effect on VDR, some clinical and experimental data indicate that probiotic bacteria may increase vitamin D levels [34]. In the gut lumen, the mucus layer and the underlying epithelium serve to keep resident microbiota at bay [35, 36]. Vitamin D ensures an appropriate level of antimicrobial peptides in the mucus and maintains epithelial integrity by reinforcing intercellular junctions.
Gut microbiota and the metabolites they produce constitute an important part of the mucosal barrier, but the relationship between disturbance of the gut flora and the development of IBDs is not fully understood [33, 37,38,39,40,41].
In sum, serum vitamin D levels affect the distribution of fecal microbiota, and elevated vitamin D levels are generally associated with higher levels of beneficial bacteria and reduced levels of pathogenic bacteria [36, 41, 42]. Gut microbiota helps to maintain gut immunity and is essential for protection against pathogens. Vitamin D/VDR regulates functions of Paneth cells and modulates release of antimicrobial peptides in gut microbiota-host interactions. Meanwhile, beneficial microbial metabolites, e.g., butyrate, upregulate the VDR signaling.
5 Gastrointestinal malabsorptive conditions
The clinical gastrointestinal conditions that were discussed during the Conference were CD, IBDs and bariatric surgery. A common denominator of these diseases was the malabsorptive state leading to decreased circulating 25(OH)D levels as the widely accepted biochemical marker of vitamin D status [2]. Additionally, vitamin D deficiency may have negative effects on the underlying gastrointestinal conditions due to some of its extraskeletal immunomodulatory and metabolic effects [4]. Vitamin D is increasingly viewed as an immune modulator capable of directly impacting both innate and adaptive immune responses [36, 41, 43,44,45,46] (Fig. 2). In innate immunity, vitamin D inhibits LPS-induced p38 activation and IL-6 and TNF-α production by monocytes and downregulates TLR-9 expression. Vitamin D also favors an anti-inflammatory phenotype of macrophages, inhibits the innate NF-κB and MAPK signaling in dendritic cells. The activation of NLRP3 inflammasome is downregulated by vitamin D. In adaptive immunity, vitamin D downregulates Th1/Th17 while it upregulates Treg and Th2. Vitamin D, through the VDR, inhibits the proliferation of B-cells and T-cells and the expression of pro-inflammatory cytokines, such as IL-2, IFN- γ, IL-12, IL-17 and TNF-α from T-cells [43, 47,48,49,50,51]. Conversely, vitamin D enhances the production of anti-inflammatory cytokines, such as IL-4 and IL-10 [52,53,54] (Fig. 3).
The birectional pathophysiological relationships between the malabsorptive gastrointestinal diseases leading to the occurrence of hypovitaminosis D (upper part of the figure) and the different mechanisms through which low vitamin D could influence the underlying gastrointestinal conditions (lower part of the figure)
6 Celiac disease
The most prevalent malabsorption condition, affecting about 0.7% of the world population, is CD. CD is characterized histologically by intestinal villus atrophy, crypt hyperplasia and lymphocytic infiltration. In the setting of long-standing CD, low bone mineral density (BMD) is a common finding, due to secondary hyperparathyroidism triggered by calcium and vitamin D malabsorption. Screening for CD among patients with osteoporosis is a matter of debate unless there are concomitant clinical signs of malabsorption. In patients with CD the initiation of a gluten free diet improves BMD, controls the secondary hyperparathyroidism, reduces bone alkaline phosphatase activity and improves vitamin D status in more than 80% of patients. Time-course of improvement depends in part on duration and severity of the disease.
6.1 Vitamin D status in celiac disease
Lower vitamin D levels are commonly observed in patients affected by CD (Fig. 2). Pediatric retrospective studies report vitamin D deficiency in 9–52% of CD patients [55]. In adult patients, older reports place the percentage of the vitamin D deficiency in CD between 20.3 and 59% [56]. A more recent published meta-analysis including 24 articles and 25 sets of data evaluating a total of 1137 CD patients and 2613 controls, showed that the average 25(OH)D level in CD patients was 3.34 ng/mL (8.36 nmol/L) lower than controls. Confirming the negative effect of chronic inflammation and intestinal damage of CD on the vitamin D intestinal absorption (Fig. 1), this meta-analysis reported that, after a gluten free diet, the average 25(OH)D level in treated patients was 6.24 ng/mL (15.6 nmol/L) higher than untreated patients [57]. Other prospective reports showed that the high prevalence of vitamin D deficiency observed in these patients at diagnosis, slightly decreased after starting and during the gluten free diet [56].
6.2 Skeletal impact of vitamin D status in celiac disease
Hypocalcemia and skeletal disease are frequent findings in CD and may even represent the presenting features of the disease [58]. In the setting of a long-standing CD, low BMD is a common finding due the concomitant presence of calcium and vitamin D malabsorption with secondary hyperparathyroidism, and higher levels of proinflammatory cytokines, including IL-1 beta, IL-2, IL-6, and tumor necrosis factor alpha. These factors help to account for accelerated bone turnover and skeletal demineralization. Markers of bone resorption including serum bone-specific alkaline phosphatase and urinary pyridinoline cross-links, and markers of bone formation including osteocalcin have been demonstrated to be higher in individuals with CD, newly diagnosed individuals with CD and those with refractory CD when compared to patients on a gluten free diet or healthy controls [59].
The few studies of pediatric patients affected by CD show either normal or low bone mineral content at the time of diagnosis [60]. Among newly diagnosed patients with CD, 43% to 63% has Z-scores that could be interpreted to be low (between -1.0 and -2.5) or 12–21% to be very low (< -2.5) [59]. Individuals with a subclinical CD demonstrate a higher BMD compared to those with a classic disease presentation, although still lower compared to healthy controls [59].
Worsened BMD correlates with earlier onset of disease, disease activity and higher anti-transglutaminase antibodies levels, as well as menopausal status, low serum vitamin D and low dietary calcium intake [59]. Several studies have shown that a gluten free diet can improve BMD parameters with a complete normalization of bone mass only when the diagnosis was made early and a strict diet was rigorously followed [60].
Beyond the conventional evaluation of bone health with quantitative assessment of BMD by dual energy X-ray absorptiometry (DXA), novel imaging methodology is also available to assess skeletal health. For example, high resolution peripheral quantitative computed tomography (HR-pQCT) is a non-invasive method to quantitate volumetric and microarchitectural features of several peripheral skeletal sites. In a prospective study enrolling 31 premenopausal women with newly diagnosed CD and 22 healthy women of similar age, HRpQCT analysis showed that patients with CD were significantly lower in total volumetric density mg/cm3, trabecular density mg/cm3, number of trabeculae 1/mm, trabecular thickness per mm, and in cortical volumetric density [61]. These skeletal microarchitectural deficits were observed more in symptomatic CD as compared to subclinical CD.
Alterations in nutrient absorption and chronic systemic inflammation both are responsible for quantitative and qualitative deficits of bone health in CD with increased fracture risk. In a meta-analysis of case-controlled prospective studies, CD at baseline was associated with a 30% increase in the risk of any fracture and a 69% increase in the risk of hip fracture [60]. Individuals with CD were 1.92 times more likely to have sustained any fracture at some point in their lives [62]. Two studies evaluated the relationship between unrecognized CD and fracture risk. Unrecognized CD cases were subjects with positive CD autoantibodies but no clinical diagnosis of the disease. In a study of Finnish men and women aged 50 and over, the authors reported that low-energy fractures were statistically more common among the seropositive participants than the seronegative ones [63]. In a cross-sectional study of Swedish women aged 50 years and over, seropositive participants (n = 90, of whom 18.9% had fractures) were slightly but not statistically more likely to have fractures than the comparison group (n = 390, of whom 12.5% had fractures). [64]. In these two studies, fractures were ascertained only from self-report or a diagnostic registry without a specific radiological morphometric evaluation. The limitation of these studies could be interpreted to be an underreporting of the actual incidence of fractures.
6.3 Skeletal impact of vitamin D supplementation in celiac disease
Since CD is a cause of secondary osteoporosis, screening for skeletal disease and adequate therapeutic management in the setting of CD is a priority. The therapeutic approach includes, thus, not only a gluten free diet, but also adequate vitamin D and calcium supplementation. In a 1-year follow-up study following the implementation of a gluten free diet and vitamin D supplementation in 26 newly diagnosed patients with CD, improvements were demonstrated in trabecular bone with regard to volume, density, and thickness. With such a short follow-up, however, the values were still significantly lower compared to healthy controls [65]. A study evaluating CD patients treated with a gluten free diet and calcium (1.0 g/day) plus alfacalcidol (0.25–1 μg/day) supplementation for one year, showed a significantly increase in mean BMD, most definitively in the lumbar spine (mean 7.3%) [66]. Another study evaluating CD patients with low BMD treated with a gluten free diet and calcium (1.0 g/day) plus an annual injection of cholecalciferol (600.000 IU) (if vitamin 25(OH)D < 20 ng/ml) showed an improvement of 35.9% in the lumbar spine [67]. These studies have led to a general consensus that vitamin D levels should be measured at diagnosis and that supplementation be provided to restore levels to normal (Fig. 3). As for any condition associated with a metabolic disease, the normal level is considered by most experts to be > 30 ng/mL (> 75 nmol/l). Along with vitamin D and a strict gluten free diet, supplementation with calcium is also important [68].
6.4 Impact of vitamin D status and supplementation on disease activity in celiac disease
While the evidence implicating CD in abnormalities of vitamin D absorption are clear, as summarized above, no human data are available on the possible direct or indirect effects of vitamin D status and supplementation on pathological features of CD. However, recent data on experimental animals on a possible favorable role of vitamin D on CD features are intriguing [69] (Fig. 2). While animal models do not reproduce all pathological features of CD pathology, they are nevertheless noteworthy. For example, Non-Obese Diabetic ShiLtJ (NOD/ShiLtJ) mice spontaneously develop autoimmune disorders and, in particular, a celiac-like disease when exposed to grains. Alterations at the level of small intestine are very similar to those seen in human subjects with CD, namely reduction of villi length, intraepithelial infiltration of CD3 + lymphocytes and villi atrophy. Cholecalciferol administration may activate intestinal mucosa regeneration by inducing a significant change in gene expression [69]. Nutritionally, NOD/ShiLtJ mice with this model of CD consumed 10 g on average less food/week as compared to healthy controls. When they were treated with 50 and 130 µg/kg of cholecalciferol, food intake was significantly improved compared to these mice who were not given vitamin D. While food intake was improved, there were no significant improvements in body weight or in levels of serum 25(OH)D. Nevertheless, only the mice administered cholecalciferol showed regression of lesions to normal histological features (grade 0). With increasing doses of cholecalciferol, villi length, morphology, atrophy, and cell infiltration improved towards mucosal features similar to those seen in healthy control mice. The group receiving the higher dose of cholecalciferol (130 ug/kg) did not show the significantly increased expression of CD3, high expression of infiltrating lymphocytes, villus atrophy, crypt hyperplasia, or extensive ZO-1 expression.
6.5 Optimal vitamin D levels in celiac disease
Optimal care of patients with CD starts with referral to a specialist or Celiac Disease Center. An initial assessment of the patient’s current nutritional and biochemical status, and potential risk factors for associated short- and long-term complications should be performed. Specific nutritional supplements, including vitamin D, may be necessary [70]. The amount of vitamin D will vary depending upon the activity of the disease ranging from a simple nutritional amount of vitamin D (600–800 IU per day) to in some cases pharmacological doses (4.000 IU per day or more) [68] (Fig. 4). Vitamin D-fortified milk/ plant-based alternatives and other natural sources of vitamin D can complement the dietary regimen [71].
The respective relative a) Vitamin D supplemention dose required and b) Vitamin D supplementation impaired efficacy in correcting hypovitaminosis D occurrence in Bariatric Surgery, Celiac Disease and Inflammatory Bowel Diseases. Higher intensity of red corresponds to greater role in the different malabsorptive gastrointestinal conditions
No ‘gold standard’ for adequate 25(OH)D levels in CD exist but levels between 20 ng/mL and 50 ng/mL (50–125 nmol/L), the standard nutritional recommendation for healthy subjects without metabolic bone disease, may be adjusted upwards to > 30 ng/mL (> 75 nmol/l) [7]. In those with osteoporosis, the most important initial therapeutic approach is to make sure that the patient is on a gluten free diet with adequate vitamin D and calcium supplementation. Often, this intervention can be associated with marked gains in BMD. Only after the dietary and nutritional needs are met and the patient has been monitored for expected improvement, or in the case of incident clinical or morphometric fractures, bone protective pharmacological interventions can be considered [72].
7 Inflammatory bowel diseases
IBDs are categorized primarily as CsD and UC. Both IBDs display heterogeneity in inflammatory and symptomatic features between patients and within individuals over time. The etiology of IBDs has not been fully elucidated. The proposed underlying pathophysiological mechanism is the result of inappropriate activation of the immune system against environmental triggers in genetically predisposed individuals. Proposed risk factors associated with IBDs include altered intestinal flora, a diet rich in carbohydrates and fats, living in urban areas and a stressful lifestyle [73]. In this setting, an aberrant and hyperactivated innate immune response to intestinal luminal agents, possibly facilitated by an altered mucosal barrier function, results in the stimulation of dendritic cells with subsequent activation of the inflammatory response and a cascade, leading to active and chronic intestinal inflammation [73].
7.1 Vitamin D status in IBDs
Through its interaction with the VDR in gut cells, vitamin D exerts a spectrum of effects ranging from immune modulation and reduced Th1-driven inflammation to cell differentiation and intercellular adhesion, and increased colonic bacterial clearance to increased expression of intestinal epithelium tight junctions.
Patients affected by IBDs are quite often characterized by vitamin D deficiency (Fig. 2) due to multiple factors such as inadequate sun exposure, dietary restrictions, glucocorticoid treatment [74] and, in some instances, impaired absorption of nutrients (Fig. 1). Hypovitaminosis D is reported to be as high as 60% in IBD patients [74]. A systematic review with meta-analysis including 14 studies and comprising 1891 participants (938 IBD cases and 953 controls) showed that IBD patients had 64% higher odds of vitamin D deficiency when compared with controls [73], and another recent review have reported an overall prevalence of hypovitaminosis D of 31.6% in UC and 38.1% in CsD, respectively [75].
7.2 Skeletal impact of vitamin D status in IBDs
The highly reported prevalence of hypovitaminosis D, in addition to poor nutrition, chronic low-grade inflammation and the frequent corticosteroid use, is thought to impair skeletal health and lead to a high risk of bone fragility and fractures.
The association between IBDs, low BMD and fractures has been examined in several studies. A higher risk of fracture in IBDs [76] was followed by a prevalence of osteopenia ranging from 22 to 77%, and of fragility fractures from 17 to 41% [77]. A meta-analysis evaluating 16 studies including 1338 patients with IBDs and 808 controls has been published [78]. The mean ages (30–47) and gender distribution (49–53% women) were similar between the two groups. Along with a significantly lower mean BMD and Z-scores for IBD patients versus controls at all sites (femoral neck, total femur and lumbar spine), there was a significant 38% increase in global risk of fractures. These significant differences in bone density and fracture risk were maintained when stratified for the type of IBD, UC vs CsD.
Recent findings have also pointed out an impairment of bone quality in subjects with IBDs using the trabecular bone score (TBS), a texture analysis of the lumbar spine image from DXA. Utilizing TBS in a case–control study, CsD was associated with a significantly lower TBS, but not lumbar BMD when these patients were subclassified with stricture or penetrating disease as compared with those with only luminal disease. Thus, bone quality but not bone density was worse among those with more advanced CsD [79]. A cross-sectional study of 81 IBD patients (48 with CsD and 33 with UC) and 81 healthy controls reported that, compared with the healthy controls, IBD was associated with lower lumbar spine BMD, hip BMD and TBS. The patients with advanced CsD had lower TBS and lumbar spine BMD values compared with those with less severe disease [80]. Furthermore, in CsD, a low TBS was proposed to be an early negative prognostic feature [81]. Another non-invasive approach, using HR-pQCT, compared 49 young adult male patients with childhood-onset IBD and 245 matched young adult male controls. In IBD, median cortical area, median total vBMD, median cortical vBMD, median trabecular volume fraction were all lower than the control subjects [82].
7.3 Skeletal impact of vitamin D supplementation in IBDs
Vitamin D supplementation has been demonstrated to prevent bone loss in patients with CsD. Seventy-five non-hospitalized patients with CsD were randomly assigned to receive either an oral supplement of 1000 IU/day vitamin D for 1 year or no supplementation. BMD decreased significantly in controls but not in patients who received supplementation. Furthermore, BMD increased among patients who reached according to authors adequate serum levels of vitamin D with the supplementation (68%) versus BMD increases in only 18% of patients with hypovitaminosis D [83]. Also, an increase of volumetric bone density after vitamin D supplementation was prospectively observed even in paediatric patients with IBDs [84]. Fifty-five patients (aged 5–19 years) with IBDs were assessed using peripheral quantitative computed tomography after a median of 13.8 months of daily use of 2000 IU of cholecalciferol. The Z-scores of trabecular BMD and cortical bone cross-sectional area improved significantly during the follow-up period, and cholecalciferol supplementation was positively associated with trabecular BMD.
7.4 Impact of vitamin D status and supplementation on disease activity in IBDs
Low 25(OH)D has also been proposed as a biomarker for disease activity and as a predictor of poor clinical outcomes [85,86,87,88].
Vitamin D exerts its biological effects on the intestine in IBDs by maintaining mucosal barrier integrity, modulating the immune system and the composition of the gut microbiota [5, 35, 36, 86, 89,90,91,92,93]. Vitamin D deficiency or impaired VDR signaling could worsen colitis through multiple effects, including effects on bacterial diversity reducing butyrate-producing microbiota, the main substrate of intestinal epithelial cell and one of the factors regulating local immune response (Fig. 1).
A cross-sectional study observed an inverse association between serum vitamin D and disease activity in 182 patients with CsD reporting that subjects characterized by a CsD Activity Index (CDAI) levels below 150 (i.e. quiescent disease), had a median serum level of vitamin D higher than patients with mild or moderate disease [94]. A subsequent study also revealed that vitamin D levels inversely correlated with activity scores in 37 patients with CsD [95]. A study exclusively performed on 50 patients with UC supported the association between lower levels of vitamin D and disease activity observing a significantly higher concentration of serum vitamin D in the group with mild disease activity as compared to the moderate disease activity group [96]. Furthermore, lower vitamin D, negatively influencing disease activity in patients with CsD, was also independently associated with lower health-related quality of life (HRQOL) of patients affected [97]. The negative impact of poor vitamin D status on the clinical course of IBDs (Fig. 2) was also recently confirmed by a study enrolling 711 patients with CsD and 764 with UC who had not undergone surgery before vitamin D was assessed [98]. Both in CsD and in UC patients, lower vitamin D levels were associated with higher disease activity scores and C-reactive protein (CRP) levels. Severe hypovitaminosis D (< 10 ng/mL) was associated with ileocolonic disease and complicated behavior in CsD and was relevant to the disease extent in UC. Moreover, in multivariable analysis, severe deficiency of vitamin D (< 10 ng/mL) was an independent risk factor for surgery in both CsD and UC.
Different meta-analyses have investigated the correlation between vitamin D supplementation and IBDs disease activity (Fig. 4) [99,100,101]. In the first meta-analysis including 18 randomized clinical trials (RCTs) and involved 908 IBD patients, vitamin D improved 25(OH)D levels more significantly than the control group (placebo group) (ng/mL, weighted mean deviation = 7.85, 95% CI (5.52, 10.18), p < 0.001) [99] (Fig. 4). Vitamin D reduced the relapse rate more significantly than the control group (Fig. 4), but there were no significant differences between the low-dose and high-dose vitamin D treatment. The erythrocyte sedimentation rate (ESR) and CRP of patients treated with vitamin D and the control group showed no statistically significant difference. In a large meta-analysis including 27 studies comprising 8316 IBD patients (3115 UC, 5201 CsD), the association of vitamin D status with clinical outcomes was evaluated [100]. Low 25(OH)D status, mostly defined with a serum level < 20 ng/mL (19 studies) (in 5 studies < 30 ng/mL, in 1 < 10 ng/mL, in 1 < 12 ng/mL, in 1 < 35 ng/mL) was associated with increased risk of disease activity: OR 1.53 (95% CI 1.32‐1.77), mucosal inflammation: OR 1.25 (95% CI 1.06‐1.47); low quality of life (QOL) scores: OR 1.30 (95% CI 1.06‐1.60); and future clinical relapse: OR 1.23 (95% CI 1.03‐1.47). In another pooled analysis of 17 trials with 1127 IBD patients, oral vitamin D supplementation effectively increased the concentration of serum 25(OH)D and decreased serum CRP levels, but it did not decrease ESR, disease activity index, and relapse rate [101]. In another recent systematic review with meta-analysis including 12 RCTs, the risk of clinical relapse and disease activity in IBD patients treated with vitamin D supplementation compared with placebo was evaluated [102]. Vitamin D supplementation reduced the overall risk of clinical relapse in IBD patients (ITT: RR, 0.64; CI 0.46–0.89; I2 = 25% and PP: RR, 0.62; CI 0.41–0.92; I2 = 18%), especially in CsD patients in clinical remission (RR, 0.47; 95% CI, 0.27 to 0.82; I2 = 0%). Concerning the impact of vitamin D supplementation on the alteration of disease activity score, this meta-analysis showed a slight, although not statistically significant, effect on CsD patients and no effect in UC patients (SMD, -0.29; 95% CI, -0.71 to 0.14; and SMD, 0.24; 95% CI, -0.61 to 1.10, respectively).
The conflicting results of these meta-analyses derive from the different primary outcomes of the studies, the small number of patients included in the studies and the high prevalence of observational studies over the RCTs included in the meta-analysis. Only a few RCTs have examined the effects of vitamin D supplementation on outcome of IBDs. However, there is substantial heterogeneity in the cut-off values defining the degree of vitamin D deficiency, the dosage regimens, and duration of treatment with vitamin D, as well as the disease subtypes and comorbidities.
Emerging evidence suggests that vitamin D deficiency may unfavorably affect response to biological therapy, being associated with an increased risk of both primary non-response and secondary loss of response to the drugs. Normal vitamin D levels (vitamin D level was classified as low or normal based on the reference lab’s normal range: the lower cut-off for normal vitamin D levels ranged from 9 to 33 ng/ml depending on the assay) at induction with anti-TNF-α were associated with 2.64 increased odds of remission at 3 months compared to patients with low vitamin D levels (OR 2.64, 95% CI 1.31–5.32, p = 0.0067) [103] and serum vitamin D level ≤ 25 ng/mL identified patients losing response to biological drugs [104]. The same holds for an increased risk of primary non-response to vedolizumab (OR 26.10, 95% CI 14.30–48.90, p < 0.001) and failure at 1-year follow-up (OR 6.10, 95% CI 3.06–12.17, p < 0.001) [105]. Furthermore, vitamin D deficiency may worsen corticosteroid-related osteopenia/osteoporosis and increase the risk of immunomodulator-related infections, relevant complications possibly observed in patients with IBDs.
7.5 Optimal vitamin D levels in IBDs
No ‘gold standard’ for adequate 25(OH)D levels in IBDs exist, but most data suggest that a 25(OH)D level > 75 nmol/L (> 30 ng/mL) is beneficial compared with IBD patients with 25(OH)D < 50 nmol/L (< 20 ng/mL) in terms of inflammatory markers and clinical scores. In IBD patients, many experts have challenged the standard nutritional guidelines as in other diseases associated with skeletal damage. The doses required to reach recommended levels of > 30 ng/mL may exceed the nutritional guidelines for supplementation such as 600–800 IU/day because of reduced absorption. Simply put, patients should be given as much vitamin D as they need to achieve satisfactory levels of circulating 25(OH)D. In a recent meta-analysis, an attempt was made to define a daily vitamin D dosage that is most likely to yield significant results, assuming its effectiveness as adjuvant therapy. Meta-regression suggested that vitamin D dose may indeed influence treatment effectiveness, and it is to be expected to observe this effect with high dose vitamin D regimens [102].
8 Bariatric surgery
Bariatric surgery is typically associated with substantial weight loss in morbidly obese patients who commonly are characterized by low pre-surgical vitamin D levels [6]. The long-term positive effects on weight and diabetes prevention after bariatric surgery can be offset, at least in part, by bone loss and higher fracture risk. These latter consequences are thought to be related to altered bone metabolism through mechanical unloading, hormonal and bone marrow fat modifications, low vitamin D, as well as nutritional and calcium deficiencies. Due to the increasing prevalence of obesity and type 2 diabetes, indication and use of bariatric surgery have progressively and rapidly expanded. The most widely used bariatric surgery procedures are the laparoscopy sleeve gastrectomy (LSG) and the laparoscopic Roux-en Y gastric bypass (LRYGB) that are characterized by variable degrees of malabsorption. Endoscopic bariatric and metabolic therapies (EBMT) represent another progressive alternative that offers higher efficacy than pharmacotherapy and at the same time is less invasive and has a lower incidence of complications than classical surgical treatment. In some procedures, the cost of endoscopic treatments may be lower than those of bariatric surgery [106].
8.1 Vitamin D status in bariatric surgery
Several epidemiological studies demonstrate a close relationship between obesity and hypovitaminosis D. The mechanisms underlying this association are still uncertain and undoubtedly multifactorial [107]. Among these factors, lower vitamin D intake and sun exposure, as well as sequestration and volumetric dilution of vitamin D into a larger than normal adipose tissue reservoirs are relevant [108, 109]. Lower expression levels of vitamin D activating enzymes (25-hydroxylase and 1α-hydroxylase) in adipose tissue may also contribute to vitamin D insufficiency in obesity [110].
Patients undergoing bariatric surgery as a therapeutic choice to lose weight and to reduce long-term complications related to obesity are almost invariably characterized, nevertheless, by lower vitamin D levels (Figs. 1, 2, and 3), as reported by previous different studies. In a prospective follow-up study, which included data from 164 morbidly obese patients undergoing bariatric surgery, 96 (58.5%) underwent LSG and 68 (41.5%) LRYGB, a normal vitamin D level (> 30 ng/mL) was preoperatively found in only 5.7% of patients. The prevalence of vitamin D insufficiency (> 20 and < 30 ng/mL), deficiency (> 10 and < 20 ng/mL) and severe deficiency (< 10 ng/mL), was reported in the 15.1%, 59.1% and 20.1% of patients, respectively [111]. Similar findings were observed in a retrospective study including 211 patients presenting for bariatric surgery and evaluated preoperatively for nutritional deficiencies, reporting a rate of vitamin D insufficiency (> 20 and < 30 ng/mL) and deficiency (< 20 ng/mL) of 20% and 80%, respectively [112]. In a single-blind, parallel clinical trial, evaluating different vitamin D supplementation therapeutic options after bariatric surgery, patients included were characterized by a preoperative rate of normal (> 30 ng/mL), insufficient (> 20 and < 30 ng/mL) and deficient (< 20 ng/mL) vitamin D status of 22.48%, 15.5% and 62.01%, respectively [113].
In LSG, characterized by a restrictive surgical procedure, more than 80% of the stomach is transected, causing a rapid transit of nutrients through the gastric lumen. Results on the prevalence of vitamin D deficiency after LSG are inconsistent. According to some studies it ranges from 14 to 72% 1-year post-surgery [6].
LRYGB has both restrictive and malabsorptive features. It is likely that the malabsorption induced by the surgical bypass procedure modifies the delivery of pancreatic secretions and bile salts leading to reduced vitamin D absorption. Moreover, intestinal fractional calcium absorption decreases from about 33% to about 7%, 6 months after surgery [114]. Daily supplementation with relatively low dose of vitamin D (800 IU) had a limited effect on preventing deficiency [6].
A less common surgical procedure is the biliopancreatic diversion (BPD) which causes massive malabsorption of minerals and fat-soluble vitamins. Vitamin D deficiency and increased PTH levels are common findings in patients undergoing BPD (ranging from 60 to 100% according to different studies) despite replacement with high oral doses of vitamin D [6].
8.2 Skeletal consequences of vitamin D status in bariatric surgery
During the last decade, bariatric procedures characterized by poor vitamin D status have been associated with likely multifactorial bone loss and skeletal fragility with higher risk of fractures. Prospective studies have shown that the magnitude of skeletal changes varies by skeletal region and surgical procedure [115]. DXA-measured bone loss at the femoral neck and total hip ranges from 5 to 11% 1 year after BPD and LRYGB surgery, while the BMD loss after restrictive procedures ranges from no change to 14%. Spine BMD changes are inconsistent with studies reporting 12-month reductions of 3–8% after BPD and LRYGB, but no change or even slight gains after restrictive procedures. Based on observational studies, bariatric surgery is also associated with a 21–44% higher risk of all fractures [116]. Fracture risk is reported to be time-dependent and increases approximately 3 years after bariatric surgery. The bariatric procedures that have a malabsorptive component (LRYGB and BPD) have clearly been associated with the highest risk of fracture compared to the restrictive procedures.
8.3 Skeletal effects of vitamin D supplementation in bariatric surgery
A prospective open-label study was conducted in a single bariatric surgical center, to assess the safety and effectiveness of once-yearly intramuscular high-dose vitamin D injection (600.000 IU: currently discouraged due to possible side effects) followed by a regular oral intake of vitamin D supplements (total oral dose of 1.280 IU daily). In the year following injection in BPD patients, BMD was assessed at baseline and 12 months post-injection. A slight, but not significant, reduction at both femoral neck and lumbar spine BMD across the study period was reported [117]. Other non-controlled studies, however, have reported significant postoperative BMD reductions despite both high-dose (> 2.000 IU daily) and low-dose (< 2.000 IU daily) oral vitamin D supplementations [118, 119] (Fig. 4).
Postoperative maintenance of vitamin D through vitamin D supplementation and, perhaps, intramuscular administration are important considerations to prevent bone loss and to maintain bone mass. Furthermore, the demonstrated positive influence of vitamin D adequacy on body composition should also be considered in the postoperative period (Fig. 4) [10]. Unfortunately, clinical guidelines are lacking on presurgical vitamin D assessment and normalization as well as on how to monitor and manage vitamin D deficiency following bariatric surgery.
8.4 Impact of vitamin D status and supplementation on metabolic outcomes in bariatric surgery
Adipose tissue is a direct target of vitamin D, which plays a role in modulating its development, distribution, and metabolic and endocrine functions [120]. The VDR in pre-adipocytes and adipocytes, in both subcutaneous and visceral adipose tissue [121] is clearly the mediator of these properties. Moreover, due to its lipophilic structure, vitamin D accumulates in adipose tissues, the major site of vitamin D storage.
The role of vitamin D in adipocyte metabolism is still relatively unknown. Recent studies conducted in vitro on mouse adipocytes showed that 1.25(OH)2D increases basal and adrenergically stimulated lipolysis and decreases de novo lipogenesis [122], suggesting that active vitamin D has catabolic effects in adipocytes by decreasing lipid and triglycerides accumulation. Adipocyte size could be reduced, as a result. Moreover, vitamin D is known to affect insulin actions and glucose metabolism in adipose tissue, by increasing glucose transport in adipocytes through enhanced GLUT4 translocation [123].
The well-known anti-inflammatory actions of vitamin D reduce inflammation in adipose tissue. In both preadipocytes and adipocytes, 1.25(OH)2D suppresses expression of multiple cytokines, including IL-6, IL-1β, IL-8 [124].
It follows, therefore, that vitamin D supplementation could represent a possibly additional pre- and post-operative measure to maintain weight loss in patients after bariatric surgery (Fig. 4). In fact, some but not all interventional studies, RCTs and meta-analyses have highlighted possible vitamin D anti-obesity properties which however need confirmation through solid evidences. A meta-analysis focused on vitamin D supplementation in overweight and obese individuals with different conditions evaluated 11 RCTs with a total of 947 subjects, with a mean time of the follow-up from 1 to 12 months and different vitamin D interventions (from 25.000 to 600.000 IU/monthly of cholecalciferol). This meta-analysis reported that cholecalciferol supplementation decreased BMI by -0.32 kg/m2 and waist circumference by -1.42 cm, but did not statistically affect weight loss [125].
A meta-analysis analyzed RCTs of oral vitamin D supplementation in obese individuals without weight loss, in obese subjects on medical weight loss regimens, and in those following bariatric surgery [126]. The latter group included specifically 6 RCTs (2 study duration < 12 months, 4 > 12 months) with a total of 615 patients evaluated. Treatment with vitamin D daily equivalent to between 800 and 7142 IU did not affect weight loss in any of the studies. However, weaked statistical power considerations limited any conclusions that could be drawn [126]. Additionally, it should be noted that vitamin D has been consistently shown to have relevant positive effects on muscle structure and function [127] and a role for vitamin D has been advocated in sarcopenic obesity [10]. Therefore, although no specific data are available on the adjuvant effect of vitamin D supplementation in weight reduction following bariatric surgery it can be hypothesized that ensuring vitamin D adequacy may help patients lose weight and/or improve body composition.
8.5 Optimal levels of vitamin D before and after bariatric surgery
Currently, there are no specific guidelines and no consensus on goals for adequate vitamin D supplementation in bariatric patients, pre- and post-surgery.
A very recent published meta-analysis was conducted to examine the effect of vitamin D supplements on serum level of 25(OH)D in the patients undergoing bariatric surgery [128]. Nine clinical trials were included in the meta-analysis. Vitamin D supplementation in patients undergoing bariatric surgery modestly improves vitamin D status particularly, in the doses above 2850 IU/day and in the patients with BMI greater than 50 kg/m2.
In the meta-analyses conducted by Bassatne et al., including 6 RCTs, four conducted in patients following LSGB, one in LSG, and another one combining both LRYGB and LSG patients, only vitamin D doses ≥ 2000 IU/d led consistently to mean 25(OH)D concentration > 30 ng/ml [126]. The average increment in 25(OH)D concentration per 100 IU/day of vitamin D dose in this population ranged between 0.4 and 1.1 ng/ml with doses of 600–3500 IU/day, and 0.2–0.4 ng/ml at doses exceeding 3500 IU/day [126].
LSG consisting in a stomach transection is considered to promote weight loss mainly, but not totally, with a restrictive effect leading to a minor, but not insignificant, malabsorptive impact on nutrients and vitamin D absorption. Daily doses of at least 3.000 IU of vitamin D have been required in these patients to reach the recommended threshold of 28 ng/mL [6]. On the other hand, RYGB has both restrictive and malabsorptive features to promote substantial weight loss, leading to a greater impact on nutrient malabsorption. Doses up to 5.000 IU per day have stabilized levels in these subjects whereas supplementation with usual doses of vitamin D (800 IU daily) had a limited effect on preventing vitamin D deficiency [6].
The consensus is that high doses of vitamin D supplementation and, perhaps, intramuscular vitamin D administration should be considered in all patients before and after bariatric surgery (Fig. 4).
9 Conclusions
Malabsorptive gastrointestinal conditions such as celiac disease, IBDs and bariatric surgery negatively affect through multiple mechanisms vitamin D absorption and metabolism (Figs. 1, 2, and 3) leading to hypovitaminosis D the severity of which depends on the different underlying conditions (Fig. 2) and on the severity of each condition with consequent higher risk of skeletal complications including hypocalcemia, impaired BMD and increased risk of fractures. Therefore, vitamin D status assessment and supplementation should be routinely considered in all patients affected by these malabsorptive gastrointestinal conditions. This concept is strengthened by the existence of a possible bidirectional relationship through which poor vitamin D status may negatively impact on clinical course of underlying disease (Figs. 2 and 3) particularly in IBDs (Fig. 2). Sufficient elements are available to estimate the desired threshold vitamin D level above which a favourable impact on the skeleton may be obtained and available data suggest variable efficacy and needs in dose and route of administration of vitamin D in order to reach target levels (Fig. 4) according to the different conditions. On the other hand, ad hoc controlled clinical trials are needed to better define this threshold for obtaining a positive effect of vitamin D supplementation on occurrence and clinical course of malabsorptive gastrointestinal diseases with the final goal of a possibly personalized supplementation of vitamin D which should also consider the specific genetic and epigenetic background of the affected patients.
Data availability
Not applicable for this paper.
References
Giustina A, Adler RA, Binkley N, Bouillon R, Ebeling PR, Lazaretti-Castro M, Marcocci C, Rizzoli R, Sempos CT, Bilezikian JP. Controversies in Vitamin D: summary statement from an international conference. J Clin Endocrinol Metab. 2019;104:234–40. https://doi.org/10.1210/jc.2018-01414.
Sempos CT, Heijboer AC, Bikle DD, Bollerslev J, Bouillon R, Brannon PM, DeLuca HF, Jones G, Munns CF, Bilezikian JP, Giustina A, Binkley N. Vitamin D assays and the definition of hypovitaminosis D: Results from the first international conference on controversies in vitamin D. Br J Clin Pharmacol. 2018;84:2194–207. https://doi.org/10.1111/bcp.13652.
Ebeling PR, Adler RA, Jones G, Liberman UA, Mazziotti G, Minisola S, Munns CF, Napoli N, Pittas AG, Giustina A, Bilezikian JP, Rizzoli R. Management of endocrine disease: Therapeutics of vitamin D. Eur J Endocrinol. 2018;179:R239–59. https://doi.org/10.1530/EJE-18-0151.
Bouillon R, Marcocci C, Carmeliet G, Bikle D, White JH, Dawson-Hughes B, Lips P, Munns CF, Lazaretti-Castro M, Giustina A, Bilezikian J. Skeletal and extraskeletal actions of vitamin D: Current evidence and outstanding questions. Endocr Rev. 2019;40:1109–51. https://doi.org/10.1210/er.2018-00126.
A. Giustina, R.A. Adler, N. Binkley, J. Bollerslev, R. Bouillon, B. Dawson-Hughes, P.R. Ebeling, D. Feldman, A.M. Formenti, M. Lazaretti-Castro, C. Marcocci, R. Rizzoli, C.T. Sempos, J.P. Bilezikian, Consensus statement from 2nd International Conference on Controversies in Vitamin D. Rev. Endocr. Metab. Disord. 21, 89–116 (2020). https://doi.org/10.1007/s11154-019- 09532-w.
Giustina A, Bouillon R, Binkley N, Sempos C, Adler RA, Bollerslev J, Dawson-Hughes B, Ebeling PR, Feldman D, Heijboer A, Jones G, Kovacs CS, Lazaretti-Castro M, Lips P, Marcocci C, Minisola S, Napoli N, Rizzoli R, Scragg R, White JH, Formenti AM, Bilezikian JP. Controversies in Vitamin D: a statement from the third international conference. JBMR. 2020;4:e10417. https://doi.org/10.1002/jbm4.10417.
Bilezikian JP, Formenti AM, Adler RA, Binkley N, Bouillon R, Lazaretti-Castro M, Marcocci C, Napoli N, Rizzoli R, Giustina A. Vitamin D: dosing, levels, form, and route of administration: does one approach fit all. Rev Endocr Metab Disord. 2021;22:1201–18. https://doi.org/10.1007/s11154-021-09693-7.
Giustina A, Bouillon R, Dawson-Hughes B, Ebeling PR, Lazaretti-Castro M, Lips P, Marcocci C, Bilezikian JP (2022) Vitamin D in the older population: a consensus statement. Endocrine. 1–14. Advance online publication. https://doi.org/10.1007/s12020-022-03208-3
di Filippo L, Frara S, Giustina A. The emerging osteo-metabolic phenotype of COVID-19: clinical and pathophysiological aspects. Nat Rev Endocrinol. 2021;17(8):445–6. https://doi.org/10.1038/s41574-021-00516-y.
Di Filippo L, De Lorenzo R, Giustina A, Rovere-Querini P, Conte C. Vitamin D in Osteosarcopenic Obesity. Nutrients. 2022;14(9):1816. https://doi.org/10.3390/nu14091816.
Bilezikian JP, Binkley N, De Luca HF, Fassio A, Formenti AM, Fuleihan GE, Heijboer AC, Giustina A. Consensus and controversial aspects of vitamin D and COVID-19. J Clin Endocrinol Metab. 2022;dgac719. https://doi.org/10.1210/clinem/dgac719.
Kellett GL. Alternative perspective on intestinal calcium absorption: proposed complementary actions of Ca(v)1.3 and TRPV6. Nutr Rev. 2011;69(7):347–70.
Hoenderop JG, Nilius B, Bindels RJ. Calcium absorption across epithelia. Physiol Rev. 2005;85(1):373–422.
Benn BS, Ajibade D, Porta A, Dhawan P, Hediger M, Peng JB, Jiang Y, Oh GT, Jeung EB, Lieben L, Bouillon R, Carmeliet G, Christakos S. Active intestinal calcium transport in the absence of transient receptor potential vanilloid type 6 and calbindin-D9k. Endocrinology. 2008;149(6):3196–205.
Ryan ZC, Craig TA, Filoteo AG, Westendorf JJ, Cartwright EJ, Neyses L, Strehler EE, Kumar R. Deletion of the intestinal plasma membrane calcium pump, isoform 1, Atp2b1, in mice is associated with decreased bone mineral density and impaired responsiveness to 1, 25-dihydroxyvitamin D3. Biochem Biophys Res Commun. 2015;467(1):152–6.
Bikle DD, Munson S. 1.25-Dihydroxyvitamin D increases calmodulin binding to specific proteins in the chick duodenal brush border membrane. J Clin Invest. 1985;76(6):2312–6.
Fujita H, Chiba H, Yokozaki H, Sakai N, Sugimoto K, Wada T, Kojima T, Yamashita T, Sawada N. Differential expression and subcellular localization of claudin-7, -8, -12, -13, and -15 along the mouse intestine. J Histochem Cytochem. 2006;54(8):933–44.
Fujita H, Sugimoto K, Inatomi S, Maeda T, Osanai M, Uchiyama Y, Yamamoto Y, Wada T, Kojima T, Yokozaki H, Yamashita T, Kato S, Sawada N, Chiba H. Tight junction proteins claudin-2 and -12 are critical for vitamin D-dependent Ca2+ absorption between enterocytes. Mol Biol Cell. 2008;19(5):1912–21.
Van Itallie CM, Fanning AS, Anderson JM. Reversal of charge selectivity in cation or anion-selective epithelial lines by expression of different claudins. Am J Physiol Renal Physiol. 2003;285(6):F1078–84.
Rievaj J, Pan W, Cordat E, Alexander RT. The Na(+)/H(+) exchanger isoform 3 is required for active paracellular and transcellular Ca(2)(+) transport across murine cecum. Am J Physiol Gastrointest Liver Physiol. 2013;305(4):G303–13.
Duflos C, Bellaton C, Pansu D, Bronner F. Calcium solubility, intestinal sojourn time and paracellular permeability codetermine passive calcium absorption in rats. J Nutr. 1995;125(9):2348–55.
Turner JR, Rill BK, Carlson SL, Carnes D, Kerner R, Mrsny RJ, Madara JL. Physiological regulation of epithelial tight junctions is associated with myosin light-chain phosphorylation. Am J Physiol. 1997;273(4):C1378–85.
Munson S, Wang Y, Chang W, Bikle DD. Myosin 1a regulates osteoblast differentiation independent of intestinal calcium transport. J Endocr Soc. 2019;3(11):1993–2011.
Mace OJ, Morgan EL, Affleck JA, Lister N, Kellett GL. Calcium absorption by Cav1.3 induces terminal web myosin II phosphorylation and apical GLUT2 insertion in rat intestine. J Physiol. 2007;580(Pt. 2):605–16.
Lee JJ, Liu X, O'Neill D, Beggs MR, Weissgerber P, Flockerzi V, Chen XZ, Dimke H, Alexander RT. Activation of the calcium sensing receptor attenuates TRPV6-dependent intestinal calcium absorption. JCI Insight. 2019;5.
Chanpaisaeng K, Teerapornpuntakit J, Wongdee K, Charoenphandhu N. Emerging roles of calcium-sensing receptor in the local regulation of intestinal transport of ions and calcium. Am J Physiol Cell Physiol. 2021;320(3):C270–8.
Charoenphandhu N, Krishnamra N. Prolactin is an important regulator of intestinal calcium transport. Can J Physiol Pharmacol. 2007;85(6):569–81.
Charoenphandhu N, Nakkrasae LI, Kraidith K, Teerapornpuntakit J, Thongchote K, Thongon N, Krishnamra N. Two-step stimulation of intestinal Ca(2+) absorption during lactation by long-term prolactin exposure and suckling-induced prolactin surge. Am J Physiol Endocrinol Metab. 2009;297(3):E609–19.
Nakkrasae LI, Thongon N, Thongbunchoo J, Krishnamra N, Charoenphandhu N. Transepithelial calcium transport in prolactin-exposed intestine-like Caco-2 monolayer after combinatorial knockdown of TRPV5, TRPV6 and Ca(v)1.3. J Physiol Sci. 2010;60(1):9–17.
Van Cromphaut SJ, Rummens K, Stockmans I, Van Herck E, Dijcks FA, Ederveen AG, Carmeliet P, Verhaeghe J, Bouillon R, Carmeliet G. Intestinal calcium transporter genes are upregulated by estrogens and the reproductive cycle through vitamin D receptor-independent mechanisms. J Bone Mineral Res Off J Am Soc Bone Miner Res. 2003;18(10):1725–36. https://doi.org/10.1359/jbmr.2003.18.10.1725.
Thomas RL, Jiang L, Adams JS, Xu ZZ, Shen J, Janssen S, et al. Vitamin D metabolites and the gut microbiome in older men. Nat Commun. 2020;11(1):5997. https://doi.org/10.1038/s41467-020-19793-8.
Schäffler H, Herlemann DP, Klinitzke P, Berlin P, Kreikemeyer B, Jaster R, et al. Vitamin D administration leads to a shift of the intestinal bacterial composition in Crohn’s disease patients, but not in healthy controls. J Dig Dis. 2018;19(4):225–34. https://doi.org/10.1111/1751-2980.12591.
Charoenngam N, Shirvani A, Kalajian TA, Song A, Holick MF. The Effect of Various Doses of Oral Vitamin D(3) Supplementation on Gut Microbiota in Healthy Adults: A Randomized, Double-blinded, Dose-response Study. Anticancer Res. 2020;40(1):551–6. https://doi.org/10.21873/anticanres.13984.
Pagnini C, Di Paolo MC, Graziani MG, Delle Fave G. Probiotics and vitamin D/vitamin D receptor pathway interaction: Potential therapeutic implications in inflammatory bowel disease. Front Pharmacol. 2021;12:747856. https://doi.org/10.3389/fphar.2021.747856.
Fakhoury HMA, Kvietys PR, AlKattan W, Anouti FA, Elahi MA, Karras SN, Grant WB. Vitamin D and intestinal homeostasis: Barrier, microbiota, and immune modulation. J Steroid Biochem Mol Biol. 2020;200:105663. https://doi.org/10.1016/j.jsbmb.2020.105663.
Vernia F, Valvano M, Longo S, Cesaro N, Viscido A, Latella G. Vitamin D in inflammatory bowel diseases. Mechanisms of action and therapeutic implications. Nutrients. 2022;14(2):269. https://doi.org/10.3390/nu14020269.
Matsuoka K, Kanai T. The gut microbiota and inflammatory bowel disease. Semin Immunopathol. 2015;37(1):47–55. https://doi.org/10.1007/s00281-014-0454-4.
Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14(10):573–84. https://doi.org/10.1038/nrgastro.2017.88.
Zuo T, Ng SC. The gut microbiota in the pathogenesis and therapeutics of inflammatory bowel disease. Front Microbiol. 2018;9:2247. https://doi.org/10.3389/fmicb.2018.02247.
Lavelle A, Sokol H. Gut microbiota-derived metabolites as key actors in inflammatory bowel disease. Nat Rev Gastroenterol Hepatol. 2020;17(4):223–37. https://doi.org/10.1038/s41575-019-0258-z.
Wu Z, Liu D, Deng F. The role of vitamin D in immune system and inflammatory bowel disease. J Inflamm Res. 2022;15:3167–85. https://doi.org/10.2147/JIR.S363840.
Battistini C, Ballan R, Herkenhoff ME, Saad SMI, Sun J. Vitamin D modulates intestinal microbiota in inflammatory bowel diseases. Int J Mol Sci. 2020;22(1):362. https://doi.org/10.3390/ijms22010362.
Bora S, Cantorna MT. The role of UVR and vitamin D on T cells and inflammatory bowel disease. Photochem Photobiol Sci. 2017;16(3):347–53. https://doi.org/10.1039/c6pp00266h.
Dionne S, Duchatelier CF, Seidman EG. The influence of vitamin D on M1 and M2 macrophages in patients with Crohn’s disease. Innate Immun. 2017;23(6):557–65. https://doi.org/10.1177/1753425917721965.
Mudambi K, Bass D. Vitamin D: a brief overview of its importance and role in inflammatory bowel disease. Transl Gastroenterol Hepatol. 2018;3:31. https://doi.org/10.21037/tgh.2018.05.03.
Schardey J, Globig AM, Janssen C, Hofmann M, Manegold P, Thimme R, Hasselblatt P. Vitamin D inhibits pro-inflammatory T cell function in patients with inflammatory bowel disease. J Crohns Colitis. 2019;13(12):1546–57. https://doi.org/10.1093/ecco-jcc/jjz090.
Griffin MD, Lutz W, Phan VA, Bachman LA, McKean DJ, Kumar R. Dendritic cell modulation by 1alpha,25 dihydroxyvitamin D3 and its analogs: a vitamin D receptor-dependent pathway that promotes a persistent state of immaturity in vitro and in vivo. Proc Natl Acad Sci USA. 2001;98(12):6800–5. https://doi.org/10.1073/pnas.121172198.
Mathieu C, Adorini L. The coming of age of 1.25-dihydroxyvitamin D(3) analogs as immunomodulatory agents. Trends Mol Med. 2002;8(4):174–9. https://doi.org/10.1016/s1471-4914(02)02294-3.
Mahon BD, Wittke A, Weaver V, Cantorna MT. The targets of vitamin D depend on the differentiation and activation status of CD4 positive T cells. J Cell Biochem. 2003;89(5):922–32. https://doi.org/10.1002/jcb.10580.
Sadeghi K, Wessner B, Laggner U, Ploder M, Tamandl D, Friedl J, Zügel U, Steinmeyer A, Pollak A, Roth E, Boltz-Nitulescu G, Spittler A. Vitamin D3 down-regulates monocyte TLR expression and triggers hyporesponsiveness to pathogen-associated molecular patterns. Eur J Immunol. 2006;36(2):361–70. https://doi.org/10.1002/eji.200425995.
Chen J, Bruce D, Cantorna MT. Vitamin D receptor expression controls proliferation of naïve CD8+ T cells and development of CD8 mediated gastrointestinal inflammation. BMC Immunol. 2014;15:6. https://doi.org/10.1186/1471-2172-15-6.
Cantorna MT, Snyder L, Lin YD, Yang L. Vitamin D and 1.25(OH)2D regulation of T cells. Nutrients. 2015;7(4):3011–21. https://doi.org/10.3390/nu7043011.
Korf H, Wenes M, Stijlemans B, Takiishi T, Robert S, Miani M, Eizirik DL, Gysemans C, Mathieu C. 1.25-Dihydroxyvitamin D3 curtails the inflammatory and T cell stimulatory capacity of macrophages through an IL-10-dependent mechanism. Immunobiology. 2012;217(12):1292–300. https://doi.org/10.1016/j.imbio.2012.07.018.
Verma R, Kim JY. 1.25-dihydroxyvitamin D3 facilitates M2 polarization and upregulates TLR10 expression on human microglial cells. Neuroimmunomodulation. 2016;23(2):75–80. https://doi.org/10.1159/000444300.
Ahlawat R, Weinstein T, Pettei MJ. Vitamin D in pediatric gastrointestinal disease. Curr Opin Pediatr. 2017;29(1):122–7. https://doi.org/10.1097/MOP.0000000000000451.
Zingone F, Ciacci C. The value and significance of 25(OH) and 1.25(OH) vitamin D serum levels in adult coeliac patients: A review of the literature. Digest Liver Dis. 2018;50(8):757–60. https://doi.org/10.1016/j.dld.2018.04.005.
Lu C, Zhou W, He X, Zhou X, Yu C. Vitamin D status and vitamin D receptor genotypes in celiac disease: a meta-analysis. Crit Rev Food Sci Nutr. 2021;61(12):2098–106. https://doi.org/10.1080/10408398.2020.1772716.
Shaker JL, Brickner RC, Findling JW, Kelly TM, Rapp R, Rizk G, Haddad JG, Schalch DS, Shenker Y. Hypocalcemia and skeletal disease as presenting features of celiac disease. Arch Intern Med. 1997;157(9):1013–6.
Micic D, Rao VL, Semrad CE. Celiac disease and its role in the development of metabolic bone disease. J Clin Densitom. 2020;23(2):190–9. https://doi.org/10.1016/j.jocd.2019.06.005.
Bianchi ML, Bardella MT. Bone and celiac disease. Calcif Tissue Int. 2002;71(6):465–71. https://doi.org/10.1007/s00223-001-2131-6.
Zanchetta MB, Costa F, Longobardi V, Longarini G, Mazure RM, Moreno ML, Vázquez H, Silveira F, Niveloni S, Smecuol E, Temprano MDL, Hwang HJ, González A, Mauriño EC, Bogado C, Zanchetta JR, Bai JC. Significant bone microarchitecture impairment in premenopausal women with active celiac disease. Bone. 2015;76:149–57. https://doi.org/10.1016/j.bone.2015.03.005.
Heikkilä K, Pearce J, Mäki M, Kaukinen K. Celiac disease and bone fractures: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2015;100(1):25–34. https://doi.org/10.1210/jc.2014-1858.
Vilppula A, Kaukinen K, Luostarinen L, Krekelä I, Patrikainen H, Valve R, Luostarinen M, Laurila K, Mäki M, Collin P. Clinical benefit of gluten-free diet in screen-detected older celiac disease patients. BMC Gastroenterol. 2011;11:136. https://doi.org/10.1186/1471-230X-11-136.
Agardh D, Björck S, Agardh CD, Lidfeldt J. Coeliac disease-specific tissue transglutaminase autoantibodies are associated with osteoporosis and related fractures in middle-aged women. Scand J Gastroenterol. 2009;44(5):571–8. https://doi.org/10.1080/00365520902718929.
Zanchetta MB, Longobardi V, Costa F, Longarini G, Mazure RM, Moreno ML, Vázquez H, Silveira F, Niveloni S, Smecuol E, de la Paz Temprano M, Massari F, Sugai E, González A, Mauriño EC, Bogado C, Zanchetta JR, Bai JC. Impaired bone microarchitecture improves after one year on gluten-free diet: A prospective longitudinal HRpQCT study in women with celiac Disease. J Bone Miner Res. 2017;32(1):135–42. https://doi.org/10.1002/jbmr.2922.
Szymczak J, Bohdanowicz-Pawlak A, Waszczuk E, Jakubowska J. Low bone mineral density in adult patients with coeliac disease. Endokrynol Pol. 2012;63(4):270–6.
Kumar M, Rastogi A, Bhadada SK, Bhansali A, Vaiphei K, Kochhar R. Effect of zoledronic acid on bone mineral density in patients of celiac disease: a prospective, randomized, pilot study. Indian J Med Res. 2013;138(6):882–7.
Duerksen D, Pinto-Sanchez MI, Anca A, Schnetzler J, Case S, Zelin J, Smallwood A, Turner J, Verdú E, Butzner JD, Rashid M. Management of bone health in patients with celiac disease: Practical guide for clinicians. Can Fam Phys Med Fam Can. 2018;64(6):433–8.
Trasciatti S, Piras F, Bonaretti S, Marini S, Nencioni S, Biasci E, Egan CG, Nannipieri F. Effect of oral cholecalciferol in a murine model of celiac disease: A dose ranging study. J Steroid Biochem Mol Biol. 2022;220:106083. https://doi.org/10.1016/j.jsbmb.2022.106083.
Kupper C. Dietary guidelines and implementation for celiac disease. Gastroenterology. 2005;128(4 Suppl 1):S121–7. https://doi.org/10.1053/j.gastro.2005.02.024.
Mager DR, Cyrkot S, Lirette C, Brill H, Dowhaniuk J, Mileski H, Basualdo-Hammond C, Nasser R, Assor E, Marcon M, Turner JM. Nutritional considerations of a paediatric gluten-free food guide for coeliac disease. Br J Nutr. 2022;127(3):421–30. https://doi.org/10.1017/S0007114521000994.
Fouda MA, Khan AA, Sultan MS, Rios LP, McAssey K, Armstrong D. Evaluation and management of skeletal health in celiac disease: position statement. Can J Gastroenterol. 2012;26(11):819–29. https://doi.org/10.1155/2012/823648.
Del Pinto R, Pietropaoli D, Chandar AK, Ferri C, Cominelli F. Association between inflammatory bowel disease and vitamin D deficiency: A systematic review and meta-analysis. Inflamm Bowel Dis. 2015;21(11):2708–17. https://doi.org/10.1097/MIB.0000000000000546.
Abraham BP, Prasad P, Malaty HM. Vitamin D deficiency and corticosteroid use are risk factors for low bone mineral density in inflammatory bowel disease patients. Dig Dis Sci. 2014;59(8):1878–84. https://doi.org/10.1007/s10620-014-3102-x.
Parizadeh SM, Jafarzadeh-Esfehani R, Hassanian SM, Mottaghi-Moghaddam A, Ghazaghi A, Ghandehari M, Alizade-Noghani M, Khazaei M, Ghayour-Mobarhan M, Ferns GA, Parizadeh SMR, Avan A. Vitamin D in inflammatory bowel disease: From biology to clinical implications. Complement Ther Med. 2019;47:102189. https://doi.org/10.1016/j.ctim.2019.08.023.
Von Tirpitz C, Pischulti G, Klaus J, Rieber A, Brückel J, Böhm BO, Adler G, Reinshagen M. Pathologische Knochendichte bei chronischentzündlichen Darmerkrankungen-Prävalenz und Risikofaktoren [Pathological bone density in chronic inflammatory bowel diseases–prevalence and risk factors]. Z Gastroenterol. 1999;37(1):5–12.
Ali T, Lam D, Bronze MS, Humphrey MB. Osteoporosis in inflammatory bowel disease. Am J Med. 2009;122(7):599–604. https://doi.org/10.1016/j.amjmed.2009.01.022.
Szafors P, Che H, Barnetche T, Morel J, Gaujoux-Viala C, Combe B, Lukas C. Risk of fracture and low bone mineral density in adults with inflammatory bowel diseases. A systematic literature review with meta-analysis. Osteoporos Int. 2018;29(11):2389–97. https://doi.org/10.1007/s00198-018-4586-6.
Krajcovicova A, Kuzma M, Hlavaty T, Hans D, Koller T, Jackuliak P, Leskova Z, Sturdik I, Killinger Z, Payer J. Decrease of trabecular bone score reflects severity of Crohn’s disease: results of a case-control study. Eur J Gastroenterol Hepatol. 2018;30(1):101–6. https://doi.org/10.1097/MEG.0000000000000997.
Soare I, Sirbu A, Martin S, Diculescu M, Mateescu B, Tieranu C, Fica S. Assessment of bone quality with trabecular bone score in patients with inflammatory bowel disease. Sci Rep. 2021;11(1):20345. https://doi.org/10.1038/s41598-021-99669-z.
Levy-Shraga Y, Megnazi O, Modan-Moses D, Tripto-Shkolnik L, Gruber N, Haberman Y, Shouval DS, Weiss B. Trabecular bone score in children and adolescents with inflammatory bowel diseases. J Clin Densitom. 2021;24(2):243–51. https://doi.org/10.1016/j.jocd.2020.10.008.
Sigurdsson GV, Schmidt S, Mellström D, Ohlsson C, Saalman R, Lorentzon M. Young adult male patients with childhood-onset IBD have increased risks of compromised cortical and trabecular bone microstructures. Inflamm Bowel Dis. 2022;izac181. Advance online publication. https://doi.org/10.1093/ibd/izac181
Vogelsang H, Ferenci P, Resch H, Kiss A, Gangl A. Prevention of bone mineral loss in patients with Crohn’s disease by long-term oral vitamin D supplementation. Eur J Gastroenterol Hepatol. 1995;7(7):609–14.
Hradsky O, Soucek O, Maratova K, Matyskova J, Copova I, Zarubova K, Bronsky J, Sumnik Z. Supplementation with 2000 IU of cholecalciferol is associated with improvement of trabecular bone mineral density and muscle power in pediatric patients with IBD. Inflamm Bowel Dis. 2017;23(4):514–23. https://doi.org/10.1097/MIB.0000000000001047.
Tabatabaeizadeh SA, Tafazoli N, Ferns GA, Avan A, Ghayour-Mobarhan M. Vitamin D, the gut microbiome and inflammatory bowel disease. J Res Med Sci. 2018;23:75. https://doi.org/10.4103/jrms.JRMS_606_17.
Rigterink T, Appleton L, Day AS. Vitamin D therapy in children with inflammatory bowel disease: A systematic review. World journal of clinical pediatrics. 2019;8(1):1–14. https://doi.org/10.5409/wjcp.v8.i1.1.
Kellermann L, Jensen KB, Bergenheim F, Gubatan J, Chou ND, Moss A, Nielsen OH. Mucosal vitamin D signaling in inflammatory bowel disease. Autoimmun Rev. 2020;19(11):102672. https://doi.org/10.1016/j.autrev.2020.102672.
Nielsen OH, Rejnmark L, Moss AC. Role of vitamin D in the natural history of inflammatory bowel disease. J Crohns Colitis. 2018;12(6):742–52. https://doi.org/10.1093/ecco-jcc/jjy025.
Gubatan J, Moss AC. Vitamin D in inflammatory bowel disease: more than just a supplement. Curr Opin Gastroenterol. 2018;34(4):217–25. https://doi.org/10.1097/MOG.0000000000000449.
Nielsen OH, Hansen TI, Gubatan JM, Jensen KB, Rejnmark L. Managing vitamin D deficiency in inflammatory bowel disease. Frontline gastroenterology. 2019;10(4):394–400. https://doi.org/10.1136/flgastro-2018-101055.
Del Pinto R, Ferri C, Cominelli F. Vitamin D axis in inflammatory bowel diseases: Role, current uses and future perspectives. Int J Mol Sci. 2017;18(11):2360. https://doi.org/10.3390/ijms18112360.
Wang Y, Zhao X, Sun B, Yu H, Huang X. Molecular dynamics simulation study of the vanillate transport channel of Opdk. Arch Biochem Biophys. 2012;524(2):132–9. https://doi.org/10.1016/j.abb.2012.05.008.
Domazetovic V, Iantomasi T, Bonanomi AG, Stio M. Vitamin D regulates claudin-2 and claudin-4 expression in active ulcerative colitis by p-Stat-6 and Smad-7 signaling. Int J Colorectal Dis. 2020;35(7):1231–42. https://doi.org/10.1007/s00384-020-03576-0.
Jørgensen SP, Hvas CL, Agnholt J, Christensen LA, Heickendorff L, Dahlerup JF. Active Crohn’s disease is associated with low vitamin D levels. J Crohns Colitis. 2013;7(10):e407–13. https://doi.org/10.1016/j.crohns.2013.01.012.
Ham M, Longhi MS, Lahiff C, Cheifetz A, Robson S, Moss AC. Vitamin D levels in adults with Crohn’s disease are responsive to disease activity and treatment. Inflamm Bowel Dis. 2014;20(5):856–60. https://doi.org/10.1097/MIB.0000000000000016.
Dolatshahi S, Pishgar E, Jamali R. Does serum 25 hydroxy vitamin D level predict disease activity in ulcerative colitis patients? Acta Clin Belg. 2016;71(1):46–50. https://doi.org/10.1080/17843286.2015.1110895.
Ulitsky A, Ananthakrishnan AN, Naik A, Skaros S, Zadvornova Y, Binion DG, Issa M. Vitamin D deficiency in patients with inflammatory bowel disease: association with disease activity and quality of life. J Parenter Enter Nutr. 2011;35(3):308–16. https://doi.org/10.1177/0148607110381267.
Ham NS, Hwang SW, Oh EH, Kim J, Lee HS, Park SH, Yang DH, Ye BD, Byeon JS, Myung SJ, Yang SK. Influence of severe vitamin D deficiency on the clinical course of inflammatory bowel disease. Dig Dis Sci. 2021;66(2):587–96. https://doi.org/10.1007/s10620-020-06207-4.
Li J, Chen N, Wang D, Zhang J, Gong X. Efficacy of vitamin D in treatment of inflammatory bowel disease: A meta-analysis. Medicine. 2018;97(46):e12662. https://doi.org/10.1097/MD.0000000000012662.
Gubatan J, Chou ND, Nielsen OH, Moss AC. Systematic review with meta-analysis: association of vitamin D status with clinical outcomes in adult patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2019;50(11–12):1146–58. https://doi.org/10.1111/apt.15506.
Guo Y, Zhang T, Wang Y, Liu R, Chang M, Wang X. Effects of oral vitamin D supplementation on inflammatory bowel disease: a systematic review and meta-analysis. Food Funct. 2021;12(17):7588–606. https://doi.org/10.1039/d1fo00613d.
Valvano M, Magistroni M, Cesaro N, Carlino G, Monaco S, Fabiani S, Vinci A, Vernia F, Viscido A, Latella G. Effectiveness of vitamin D supplementation on disease course in inflammatory bowel disease patients: Systematic review with meta-analysis. Inflamm Bowel Dis. 2022;izac253. Advance online publication. https://doi.org/10.1093/ibd/izac253
Winter RW, Collins E, Cao B, Carrellas M, Crowell AM, Korzenik JR. Higher 25-hydroxyvitamin D levels are associated with greater odds of remission with anti-tumour necrosis factor-α medications among patients with inflammatory bowel diseases. Aliment Pharmacol Ther. 2017;45(5):653–9. https://doi.org/10.1111/apt.13936.
Valvano M, Magistroni M, Mancusi A, D’Ascenzo D, Longo S, Stefanelli G, Vernia F, Viscido A, Necozione S, Latella G. The usefulness of serum vitamin D levels in the assessment of IBD activity and response to biologics. Nutrients. 2021;13(2):323. https://doi.org/10.3390/nu13020323.
Gubatan J, Rubin SJS, Bai L, Haileselassie Y, Levitte S, Balabanis T, Patel A, Sharma A, Sinha SR, Habtezion A. Vitamin D is associated with α4β7+ immunophenotypes and predicts vedolizumab therapy failure in patients with inflammatory bowel disease. J Crohns Colitis. 2021;15(12):1980–90. https://doi.org/10.1093/ecco-jcc/jjab114.
Král J, Machytka E, Horká V, Selucká J, Doleček F, Špičák J, Kovářová V, Haluzík M, Bužga M. Endoscopic treatment of obesity and nutritional aspects of bariatric endoscopy. Nutrients. 2021;13(12):4268. https://doi.org/10.3390/nu13124268.
Migliaccio S, Di Nisio A, Mele C, Scappaticcio L, Savastano S, Colao A, Obesity Programs of nutrition, Education, Research and Assessment (OPERA) Group. Obesity and hypovitaminosis D: causality or casualty? Int J Obes Suppl. 2019;9(1):20–31. https://doi.org/10.1038/s41367-019-0010-8
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–3. https://doi.org/10.1093/ajcn/72.3.690.
Drincic AT, Armas LA, Van Diest EE, Heaney RP. Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity (Silver Spring, Md). 2012;20(7):1444–8. https://doi.org/10.1038/oby.2011.404.
Wamberg L, Christiansen T, Paulsen SK, Fisker S, Rask P, Rejnmark L, Richelsen B, Pedersen SB. Expression of vitamin D-metabolizing enzymes in human adipose tissue -- the effect of obesity and diet-induced weight loss. Int J Obes. (2005), 2013;37(5), 651–657. https://doi.org/10.1038/ijo.2012.112
Lanzarini E, Nogués X, Goday A, Benaiges D, de Ramón M, Villatoro M, Pera M, Grande L, Ramón JM. High-dose vitamin D supplementation is necessary after bariatric surgery: A prospective 2-year follow-up study. Obes Surg. 2015;25(9):1633–8. https://doi.org/10.1007/s11695-015-1572-3.
Wang C, Guan B, Yang W, Yang J, Cao G, Lee S. Prevalence of electrolyte and nutritional deficiencies in Chinese bariatric surgery candidates. Surg Obes Relat Dis. 2016;12(3):629–34. https://doi.org/10.1016/j.soard.2015.12.009.
Sayadi Shahraki M, Khalili N, Yousefvand S, Sheikhbahaei E, Shahabi Shahmiri S. Severe obesity and vitamin D deficiency treatment options before bariatric surgery: a randomized clinical trial. Surg Obes Relat Dis. 2019;15(9):1604–11. https://doi.org/10.1016/j.soard.2019.05.033.
Schafer AL, Weaver CM, Black DM, Wheeler AL, Chang H, Szefc GV, Stewart L, Rogers SJ, Carter JT, Posselt AM, Shoback DM, Sellmeyer DE. Intestinal calcium absorption decreases dramatically after gastric bypass surgery despite optimization of vitamin D status. J Bone Miner Res. 2015;30(8):1377–85. https://doi.org/10.1002/jbmr.2467.
Scibora LM. Skeletal effects of bariatric surgery: examining bone loss, potential mechanisms and clinical relevance. Diabetes Obes Metab. 2014;16(12):1204–13. https://doi.org/10.1111/dom.12363.
Paccou J, Tsourdi E, Meier C, Palermo A, Pepe J, Body JJ, Zillikens MC. Bariatric surgery and skeletal health: A narrative review and position statement for management by the European Calcified Tissue Society (ECTS). Bone. 2022;154:116236. https://doi.org/10.1016/j.bone.2021.116236.
Einarsdóttir K, Preen DB, Clay TD, Kiely L, Holman CD, Cohen LD. Effect of a single “megadose” intramuscular vitamin D (600,000 IU) injection on vitamin D concentrations and bone mineral density following biliopancreatic diversion surgery. Obes Surg. 2010;20(6):732–7. https://doi.org/10.1007/s11695-009-0024-3.
Yu EW, Bouxsein ML, Putman MS, Monis EL, Roy AE, Pratt JS, Butsch WS, Finkelstein JS. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100(4):1452–9. https://doi.org/10.1210/jc.2014-4341.
Tsiftsis DD, Mylonas P, Mead N, Kalfarentzos F, Alexandrides TK. Bone mass decreases in morbidly obese women after long limb-biliopancreatic diversion and marked weight loss without secondary hyperparathyroidism. A physiological adaptation to weight loss? Obes Surg. 2009;19(11):1497–503. https://doi.org/10.1007/s11695-009-9938-z.
Mutt SJ, Hyppönen E, Saarnio J, Järvelin MR, Herzig KH. Vitamin D and adipose tissue-more than storage. Front Physiol. 2014;5:228. https://doi.org/10.3389/fphys.2014.00228.
Ding C, Gao D, Wilding J, Trayhurn P, Bing C. Vitamin D signalling in adipose tissue. Br J Nutr. 2012;108(11):1915–23.
Larrick BM, Kim KH, Donkin SS, Teegarden D. 1.25-Dihydroxyvitamin D regulates lipid metabolism and glucose utilization in differentiated 3T3-L1 adipocytes. Nutr Res (New York, NY). 2018;58:72–83. https://doi.org/10.1016/j.nutres.2018.07.004.
Manna P, Jain SK. Vitamin D up-regulates glucose transporter 4 (GLUT4) translocation and glucose utilization mediated by cystathionine-γ-lyase (CSE) activation and H2S formation in 3T3L1 adipocytes. J Biol Chem. 2012;287(50):42324–32. https://doi.org/10.1074/jbc.M112.407833.
Wamberg L, Cullberg KB, Rejnmark L, Richelsen B, Pedersen SB. Investigations of the anti-inflammatory effects of vitamin D in adipose tissue: results from an in vitro study and a randomized controlled trial. Horm Metab Res. 2013;45(6):456–62. https://doi.org/10.1055/s-0032-1331746.
Perna S. Is Vitamin D supplementation useful for weight loss programs? A systematic review and meta-analysis of randomized controlled trials. Medicina (Kaunas). 2019;55(7):368. https://doi.org/10.3390/medicina55070368.
Bassatne A, Chakhtoura M, Saad R, Fuleihan GE. Vitamin D supplementation in obesity and during weight loss: A review of randomized controlled trials. Metabolism. 2019;92:193–205. https://doi.org/10.1016/j.metabol.2018.12.010.
Gunton JE, Girgis CM, Baldock PA, Lips P. Bone muscle interactions and vitamin D. Bone. 2015;80:89–94. https://doi.org/10.1016/j.bone.2015.02.029.
Mokhtari Z, Hosseini E, Zaroudi M, Gibson DL, Hekmatdoost A, Mansourian M, Salehi-Abargouei A, Faghihimani Z, Askari G. The effect of vitamin D supplementation on serum 25-hydroxy vitamin D in the patients undergoing bariatric surgery: A systematic review and meta-analysis of randomized clinical trials. Obes Surg. 2022;32(9):3088–103. https://doi.org/10.1007/s11695-022-06121-w.
Acknowledgements
We would like to acknowledge the support of Fabio Perversi (Polistudium, Milan, Italy) for preliminary editorial assistance. We wish to acknowledge all participants in the Conference: Adrian Martineau, Neil Binkley, Anna Maria Formenti, Ghada El-Hajj Fuleihan, Angelo Fassio, Hector F. De Luca, Annemieke C. Heijboer, Daniel D. Bikle, Salvatore Minisola, Silvia Trasciatti, Nicola Napoli, Giulia Martina Cavestro, Giovanni Latella, David Feldman, Anastassios G. Pittas, René Rizzoli, and Fabio Massimo Ulivieri.
Funding
This work was supported, in part, by International Vitamin D Expert Association (IDEA). The conference was supported by an unrestricted educational grant by Abiogen Pharma, Pisa, Italy. The sponsors had no role in the selection of discussion topics, speakers, or authors, preparation, or review of this paper.
Author information
Authors and Affiliations
Contributions
All authors contributed equally.
Corresponding author
Ethics declarations
Conflict of interest
A.G. is consultant for Abiogen and Takeda and received research grant to Institution from Takeda. S.M. served as speaker for Abiogen, Bruno Farmaceutici, Diasorin, Geopharma, Sandoz, UCB. He also served in advisory board of Abiogen, Eli Lilly, Kyowa Kirin, Novo Nordisk, UCB. The other authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Giustina, A., di Filippo, L., Allora, A. et al. Vitamin D and malabsorptive gastrointestinal conditions: A bidirectional relationship?. Rev Endocr Metab Disord 24, 121–138 (2023). https://doi.org/10.1007/s11154-023-09792-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-023-09792-7