Abstract
Purpose
Cushing’s disease (CD) results from autonomous adrenocorticotropic hormone (ACTH) secretion by corticotroph adenomas, leading to excessive cortisol production, ultimately affecting morbidity and mortality. Pasireotide is the only FDA approved tumor directed treatment for CD, but it is effective in only about 25% of patients, and is associated with a high rate of hyperglycemia. Neuromedin B (NMB), a member of the bombesin-like peptide family, regulates endocrine secretion and cell proliferation. Here, we assessed NMB and NMB receptor (NMBR) expression in human corticotroph adenomas and the effects of NMBR antagonist PD168368 on murine and human corticotroph tumors.
Methods
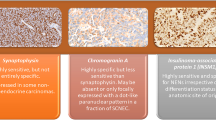
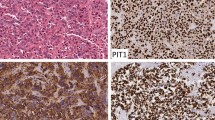
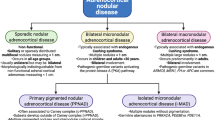
To investigate NMB and NMBR expression, real-time qPCR and immunostaining on human pathological specimens of corticotroph, non-functional and somatotroph adenomas were performed. The effects of PD168368 on hormone secretion and cell proliferation were studied in vitro, in vivo and in seven patient-derived corticotroph adenoma cells. NMB and NMBR were expressed in higher extent in human corticotroph adenomas compared with non-functional or somatotroph adenomas.
Results
In murine AtT-20 cells, PD168368 reduced proopiomelanocortin (Pomc) mRNA/protein expression and ACTH secretion as well as cell proliferation. In mice with tumor xenografts, tumor growth, ACTH and corticosterone were downregulated by PD168368. In patient-derived adenoma cells, PD168368 reduced POMC mRNA expression in four out of seven cases and ACTH secretion in two out of five cases. A PD168368-mediated cyclin E suppression was also identified in AtT-20 and patient-derived cells.
Conclusion
NMBR antagonist represents a potential treatment for CD and its effect may be mediated by cyclin E suppression.







Similar content being viewed by others
Data Availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Newell-Price J, Bertagna X, Grossman AB, Nieman LK (2006) Cushing’s syndrome. Lancet 367(9522):1605–1617. https://doi.org/10.1016/S0140-6736(06)68699-6
Dekkers OM, Horváth-Puhó E, Jørgensen JO, Cannegieter SC, Ehrenstein V, Vandenbroucke JP et al (2013) Multisystem morbidity and mortality in Cushing’s syndrome: a cohort study. J Clin Endocrinol Metab 98(6):2277–2284. https://doi.org/10.1210/jc.2012-3582
Valassi E, Tabarin A, Brue T, Feelders RA, Reincke M, Netea-Maier R et al (2019) High mortality within 90 days of diagnosis in patients with Cushing’s syndrome: results from the ERCUSYN registry. Eur J Endocrinol 181(5):461–472. https://doi.org/10.1530/EJE-19-0464
Fleseriu M, Auchus R, Bancos I, Ben-Shlomo A, Bertherat J, Biermasz NR et al (2021) Consensus on diagnosis and management of Cushing’s disease: a guideline update. Lancet Diabetes Endocrinol 9(12):847–875. https://doi.org/10.1016/S2213-8587(21)00235-7
Pivonello R, De Leo M, Cozzolino A, Colao A (2015) The treatment of Cushing’s disease. Endocr Rev 36(4):385–486. https://doi.org/10.1210/er.2013-1048
Boscaro M, Ludlam WH, Atkinson B, Glusman JE, Petersenn S, Reincke M et al (2009) Treatment of pituitary-dependent Cushing’s disease with the multireceptor ligand somatostatin analog pasireotide (SOM230): a multicenter, phase II trial. J Clin Endocrinol Metab 94(1):115–122. https://doi.org/10.1210/jc.2008-1008
Colao A, Petersenn S, Newell-Price J, Findling JW, Gu F, Maldonado M et al (2012) A 12-month phase 3 study of pasireotide in Cushing’s disease. N Engl J Med 366(10):914–924. https://doi.org/10.1056/NEJMoa1105743
Lacroix A, Gu F, Gallardo W, Pivonello R, Yu Y, Witek P et al (2018) Efficacy and safety of once-monthly pasireotide in Cushing’s disease: a 12 month clinical trial. Lancet Diabetes Endocrinol 6(1):17–26. https://doi.org/10.1016/S2213-8587(17)30326-1
Manetti L, Deutschbein T, Schopohl J, Yuen KCJ, Roughton M, Kriemler-Krahn U et al (2019) Long-term safety and efficacy of subcutaneous pasireotide in patients with Cushing’s disease: interim results from a long-term real-world evidence study. Pituitary 22(5):542–551. https://doi.org/10.1007/s11102-019-00984-6
Pivonello R, De Leo M, Cozzolino A, Colao A (2020) Medical treatment of Cushing’s disease: an overview of the current and recent clinical trials. Front Endocrinol (Lausanne) 11:648. https://doi.org/10.3389/fendo.2020.00648
Castinetti F, Nieman LK, Reincke M, Newell-Price J (2021) Approach to the patient treated with steroidogenesis inhibitors. J Clin Endocrinol Metab 106(7):2114–2123. https://doi.org/10.1210/clinem/dgab122
Fukuoka H, Cooper O, Ben-Shlomo A, Mamelak A, Ren SG, Bruyette D et al (2011) EGFR as a therapeutic target for human, canine, and mouse ACTH-secreting pituitary adenomas. J Clin Invest 121(12):4712–4721. https://doi.org/10.1172/JCI60417
Liu NA, Jiang H, Ben-Shlomo A, Wawrowsky K, Fan XM, Lin S et al (2011) Targeting zebrafish and murine pituitary corticotroph tumors with a cyclin-dependent kinase (CDK) inhibitor. Proc Natl Acad Sci U S A 108(20):8414–8419. https://doi.org/10.1073/pnas.1018091108
Liu NA, Araki T, Cuevas-Ramos D, Hong J, Ben-Shlomo A, Tone Y et al (2015) Cyclin E-mediated human proopiomelanocortin regulation as a therapeutic target for Cushing disease. J Clin Endocrinol Metab 100(7):2557–2564. https://doi.org/10.1210/jc.2015-1606
Shen Y, Ji C, Jian X, Zhou J, Zhang Q, Qiao N et al (2021) Regulation of the EGFR Pathway by HSP90 Is Involved in the Pathogenesis of Cushing’s Disease. Front Endocrinol (Lausanne) 11601984. https://doi.org/10.3389/fendo.2020.601984
Kageyama K, Asari Y, Sugimoto Y, Niioka K, Daimon M (2020) Ubiquitin-specific protease 8 inhibitor suppresses adrenocorticotropic hormone production and corticotroph tumor cell proliferation. Endocr J 67(2):177–184. https://doi.org/10.1507/endocrj.EJ19-0239
Treppiedi D, Di Muro G, Marra G, Barbieri AM, Mangili F, Catalano R et al (2021) USP8 inhibitor RA-9 reduces ACTH release and cell growth in tumor corticotrophs. Endocr Relat Cancer 28(8):573–582. https://doi.org/10.1530/ERC-21-0093
Lu J, Chatain GP, Bugarini A, Wang X, Maric D, Walbridge S et al (2017) Histone deacetylase inhibitor SAHA is a promising treatment of cushing disease. J Clin Endocrinol Metab 102(8):2825–2835. https://doi.org/10.1210/jc.2017-00464
Zhang D, Damoiseaux R, Babayan L, Rivera-Meza EK, Yang Y, Bergsneider M et al (2021) Targeting corticotroph HDAC and PI3-Kinase in Cushing disease. J Clin Endocrinol Metab 106(1):e232–e246. https://doi.org/10.1210/clinem/dgaa699
Chen Z, Jia Q, Zhao Z, Zhang Q, Chen Y, Qiao N et al (2021) Transcription factor ASCL1 acts as a novel potential therapeutic target for the treatment of the Cushing’s disease. J Clin Endocrinol Metab 106(1):e232–e246. https://doi.org/10.1210/clinem/dgaa699
Ohki-Hamazaki H, Neuromedin B, Prog Neurobiol (2000) 62(3):297–312. https://doi.org/10.1016/s0301-0082(00)00004-6
Itoh S, Takashima A, Itoh T, Morimoto T (1995) Effects of neuromedins and related peptides on the body temperature of rats. Jpn J Physiol 45(1):37–45. https://doi.org/10.2170/jjphysiol.45.37
Minamino N, Kangawa K, Matsuo H, Neuromedin C (1984) A bombesin-like peptide identified in porcine spinal cord. Biochem Biophys Res Commun 119(1):14–20. https://doi.org/10.1016/0006-291x(84)91611-5
Greeley GH Jr, Spannagel A, Hill FL, Thompson JC (1986) Comparison of the actions of bombesin, gastrin-releasing peptide-27, neuromedin B, and gastrin-releasing peptide-10 in causing release of gastrin and gastric inhibitory peptide in rats. Proc Soc Exp Biol Med 183(1):136–139. https://doi.org/10.3181/00379727-183-42398
Namba M, Ghatei MA, Ghiglione M, Bloom SR (1986) Effects of decapeptide of mammalian bombesin and neuromedin B on pancreatic exocrine secretion in the rat. Digestion 34(2):105–114. https://doi.org/10.1007/0.1159/000199318
Otsuki M, Fujii M, Nakamura T, Tani S, Oka T, Yajima H et al (1987) Effects of neuromedin B and neuromedin C on exocrine and endocrine rat pancreas. Am J Physiol 252(4 Pt 1):G491–498. https://doi.org/10.1152/ajpgi.1987.252.4.G491
Namba M, Ghatei MA, Bishop AE, Gibson SJ, Mann DJ, Polak JM et al (1985) Presence of neuromedin B-like immunoreactivity in the brain and gut of rat and guinea-pig. Peptides 6(Suppl 3):257–263. https://doi.org/10.1016/0196-9781(85)90383-3
Oliveira KJ, Ortiga-Carvalho TM, Cabanelas A, Veiga MA, Aoki K, Ohki-Hamazaki H et al (2006) Disruption of neuromedin B receptor gene results in dysregulation of the pituitary-thyroid axis. J Mol Endocrinol 36(1):73–80. https://doi.org/10.1677/jme.1.01892
Malendowicz LK, Nussdorfer GG (1995) Investigations on the acute effects of neuropeptides on the pituitary-adrenocortical function in normal and cold-stressed rats. I. Bombesin and neuromedin B. Exp Toxicol Pathol 47(1):31–34. https://doi.org/10.1016/S0940-2993(11)80279-4
Kameda H, Miyoshi H, Shimizu C, Nagai S, Nakamura A, Kondo T et al (2014) Expression and regulation of neuromedin B in pituitary corticotrophs of male melanocortin 2 receptor-deficient mice. Endocrinology 155(7):2492–2499. https://doi.org/10.1210/en.2013-2077
Kageyama K, Oki Y, Sakihara S, Nigawara T, Terui K, Suda T (2013) Evaluation of the diagnostic criteria for Cushing’s disease in Japan. Endocr J 60(2):127–135. https://doi.org/10.1507/endocrj.ej12-0299
Park HJ, Kim SR, Kim MK, Choi KS, Jang HO, Yun I et al (2011) Neuromedin B receptor antagonist suppresses tumor angiogenesis and tumor growth in vitro and in vivo. Cancer Lett 312(1):117–127. https://doi.org/10.1016/j.canlet.2011.08.014
Minamino N, Kangawa K, Matsuo H (1983) Neuromedin B: a novel bombesin-like peptide identified in porcine spinal cord. Biochem Biophys Res Commun 114(2):541–548. https://doi.org/10.1016/0006-291x(83)90814-8
Siegfried JM, Krishnamachary N, Gaither Davis A, Gubish C, Hunt JD, Shriver SP (1999) Evidence for autocrine actions of neuromedin B and gastrin-releasing peptide in non-small cell lung cancer. Pulm Pharmacol Ther 12(5):291–302. https://doi.org/10.1006/pupt.1999.0210
Sun B, Halmos G, Schally AV, Wang X, Martinez M (2000) Presence of receptors for bombesin/gastrin-releasing peptide and mRNA for three receptor subtypes in human prostate cancers. Prostate 42(4):295–303. https://doi.org/10.1002/(sici)1097-0045(20000301)42:4<295::aid-pros7>3.0.co;2-b
Matusiak D, Glover S, Nathaniel R, Matkowskyj K, Yang J, Benya RV (2005) Neuromedin B and its receptor are mitogens in both normal and malignant epithelial cells lining the colon. Am J Physiol Gastrointest Liver Physiol 288(4):G718–728. https://doi.org/10.1152/ajpgi.00156.2004
Ryan RR, Katsuno T, Mantey SA, Pradhan TK, Weber HC, Coy DH et al (1999) Comparative pharmacology of the nonpeptide neuromedin B receptor antagonist PD168368. J Pharmacol Exp Ther 290(3):1202–1211
Moody TW, Jensen RT, Garcia L, Leyton J (2000) Nonpeptide neuromedin B receptor antagonists inhibit the proliferation of C6 cells. Eur J Pharmacol 409(2):133–142. https://doi.org/10.1016/s0014-2999(00)00828-1
Moody TW, Leyton J, Garcia-Marin L, Jensen RT (2003) Nonpeptide gastrin releasing peptide receptor antagonists inhibit the proliferation of lung cancer cells. Eur J Pharmacol 474(1):21–29. https://doi.org/10.1016/s0014-2999(03)01996-4
Jordan S, Lidhar K, Korbonits M, Lowe DG, Grossman AB (2000) Cyclin D and cyclin E expression in normal and adenomatous pituitary. Eur J Endocrinol 143(1):R1–6. https://doi.org/10.1530/eje.0.143r001
Roussel-Gervais A, Bilodeau S, Vallette S, Berthelet F, Lacroix A, Figarella-Branger D et al (2010) Cooperation between cyclin E and p27(Kip1) in pituitary tumorigenesis. Mol Endocrinol 24(9):1835–1845. https://doi.org/10.1210/me.2010-0091
Araki T, Liu NA (2018) Cell cycle regulators and lineage-specific therapeutic targets for Cushing Disease. Front Endocrinol (Lausanne) 9:444. https://doi.org/10.3389/fendo.2018.00444
Liu NA, Ben-Shlomo A, Carmichael JD, Wang C, Swerdloff RS, Heaney AP et al (2022) Treatment of Cushing’s Disease with Pituitary-Targeting Seliciclib. J Clin Endocrinol Metab dgac588. https://doi.org/10.1210/clinem/dgac588
Le Tourneau C, Faivre S, Laurence V, Delbaldo C, Vera K, Girre V et al (2010) Phase I evaluation of seliciclib (R-roscovitine), a novel oral cyclin-dependent kinase inhibitor, in patients with advanced malignancies. Eur J Cancer 46(18):3243–3250. https://doi.org/10.1016/j.ejca.2010.08.001
Theodoropoulou M, Arzberger T, Gruebler Y, Jaffrain-Rea ML, Schlegel J, Schaaf L et al (2004) Expression of epidermal growth factor receptor in neoplastic pituitary cells: evidence for a role in corticotropinoma cells. J Endocrinol 183(2):385–394. https://doi.org/10.1677/joe.1.05616
Reincke M, Sbiera S, Hayakawa A, Theodoropoulou M, Osswald A, Beuschlein F et al (2015) Mutations in the deubiquitinase gene USP8 cause Cushing’s disease. Nat Genet 47(1):31–38. https://doi.org/10.1038/ng.3166
Araki T, Liu X, Kameda H, Tone Y, Fukuoka H, Tone M et al (2017) EGFR induces E2F1-Mediated Corticotroph Tumorigenesis. J Endocr Soc 1(2):127–143. https://doi.org/10.1210/js.2016-1053
Fukuoka H, Shichi H, Yamamoto M, Takahashi Y (2020) The Mechanisms Underlying Autonomous adrenocorticotropic hormone secretion in Cushing’s Disease. Int J Mol Sci 21(23):9132. https://doi.org/10.3390/ijms21239132
Moody TW, Berna MJ, Mantey S, Sancho V, Ridnour L, Wink DA et al (2010) Neuromedin B receptors regulate EGF receptor tyrosine phosphorylation in lung cancer cells. Eur J Pharmacol 637(1–3):38–45. https://doi.org/10.1016/j.ejphar.2010.03.057
Acknowledgements
This work was supported by JSPS KAKENHI Grant Numbers 18H06229, 19K21329 and 20K17481, and the Akiyama Life Science Foundation. We thank Department of Surgical Pathology, Hokkaido University Hospital for cooperation in the preparation of archival pathological specimens. We thank Mark Cleasby, PhD from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This work was supported by JSPS KAKENHI Grant Numbers 18H06229, 19K21329 and 20K17481, and the Akiyama Life Science Foundation.
Author information
Authors and Affiliations
Contributions
Tomonori Sekizaki and Hiraku Kameda designed the study, performed experiments and acquired the data. Tomonori Sekizaki and Hiroaki Motegi obtained clinical samples. Tomonori Sekizaki and Hiraku Kameda drafted the manuscript, and all other authors reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board (No. 018–0201). All patients agreed to participate in the study and provided written informed consent.
Competing interests
The authors declare no potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sekizaki, T., Kameda, H., Nakamura, A. et al. Neuromedin B receptor as a potential therapeutic target for corticotroph adenomas. Pituitary 26, 597–610 (2023). https://doi.org/10.1007/s11102-023-01350-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-023-01350-3