Abstract
The COVID-19 pandemic posed a setback to health maintenance screenings worldwide. These delays have impacted minorities and those of low socioeconomic status in the same way that disparities in cancer screenings have historically trended. Here, we evaluated the performance of a student-run free clinic in maintaining women up-to-date with cancer screenings before, during, and after the pandemic in relation to national trends. We identified all women eligible for screening mammography and cervical cancer screenings between 2018 and 2022 at the clinic (N = 185). Adequate adherence to screening was defined according to the American Cancer Society (ACS) recommendations for breast mammography, and the United States Preventive Services Task Force (USPSTF) guidelines for cervical cancer screenings. For cervical cancer screening, 166 female patients seen between 2018 and 2022 were eligible, and up-to-date proportions were as follows: 81.3% in 2018; 90.9% in 2019; 83.3% in 2020; 93.3% in 2021; 93.8% in 2022. For breast surveillance, 143 women were eligible for screening mammography, and up-to-date proportions were as follows: 66.7% in 2018; 62.5% in 2019; 91.7% in 2020; 73.1% in 2021; 84.1% in 2022. These proportions were higher than or near national averages.
In conclusion, adherence remained steady during the pandemic and was not subject to the declines seen nationally. Our clinic represents an effective model for promoting women’s health maintenance and tempering the disparities seen among women of low socioeconomic status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Free healthcare clinics serve a role in meeting healthcare gaps by providing cancer screenings for women who otherwise would not obtain these preventive services. The Building Relationships & Initiatives Dedicated to Gaining Equality (BRIDGE) Healthcare Clinic is a student-run clinic in Tampa, Florida that provides primary care services for members of the community living below the 200% poverty line. Cervical and breast cancer screenings are offered to eligible females. In light of the pandemic milieu there was a decrease in female health maintenance and screenings nationally [1, 2]. We evaluated women’s cancer screening rates at the BRIDGE clinic over 2018–2022 to discern the impact of the pandemic on clinic performance.
While the overall incidence of invasive cervical carcinoma has declined from 10 per 100,000 females to 7.8 per 100,000 over the past twenty years [3], the disease bears an overall mortality rate of approximately 55% [4]. Approximately 90% of human papilloma virus infections self-resolve; however, 10% remain latent in the squamous epithelium of the ectocervix, propagating epithelial dysplasia that can progress to high-grade intraepithelial lesions and eventually invasive carcinoma over decades [5], explaining the high incidence of cervical cancer diagnosis in females between 35 and 54 years old [6]. An approximate 70% decrease in cervical cancer rates in the U.S. is attributed to the implementation of cervical cancer screening in the 1960s [7]. The U.S. Preventative Services Task Force (USPSTF) recommends that women 21–29 years old receive a Pap test every three years, and females 30–65 years old to receive either high-risk human papilloma virus (HPV) testing or HPV plus cytology co-testing every five years, with discontinuation after 65 years of age given adequate prior screening [8]. While the national average for insured females being up-to-date with cervical cancer screenings is a propitious 79.3%, the proportion of up-to-date uninsured females is 60.3% [9]. Racial and socioeconomic disparities also impact rates of cervical cancer screening [10, 11]. Incidentally, cervical cancer is found to be detected at later stages and presents with poorer outcomes in those of lower socioeconomic status or without insurance [12, 13].
Screening mammography implemented in 1976 has contributed to a decline in breast cancer mortality [14]. However, breast cancer is still the most common cancer in women and is the leading cause of premature mortality [15]. In 2022, it is expected that 287,850 women will be diagnosed with breast cancer, and 43,250 will die from the disease [16]. The American Cancer Society (ACS) recommends that women of average risk for breast cancer aged 40–44 have the opportunity to receive a yearly mammogram; women between 45 and 54 receive a yearly mammogram, and women older than 55 years old receive a mammogram every 2 years [15]. However, screening mammography is less likely to occur in women of low income, without insurance, and of ethnic minorities [17]. Here, we evaluated our program to gauge the performance of cervical and breast cancer screening efforts at the student-run free clinic in comparison to national trends from 2018 to 2022.
Methods
A quality performance review was conducted to assess the screening status of all women aged 21–75 years seen at the BRIDGE clinic between January 9th, 2018 and May 17th, 2022 (N = 185). The study was completed by clinic student directors.
Up-to-date (UTD) cervical cancer screening was defined according to the 2018 USPSTF guidelines: females 21–29 years receive a Pap test every 3 years; females 30–65 years can receive either high-risk HPV testing or HPV plus cytology co-testing every 5 years, and discontinuation of screening can occur after 65 years of age given adequate prior screening [8].
UTD breast cancer screening was defined according to the 2015 ACS guidelines [15, 18]. The clinic adheres to these guidelines for women at average risk of breast cancer: mammography is offered to women 40–44 years old; mammography is completed yearly for women 45–54 years old, and mammography can be performed biennially for women 55–75 years old. Simple proportions of demographic characteristics and screening were calculated using SPSS.
Results
185 women between the ages of 21 and 75 years old were seen at the BRIDGE clinic between January 9th, 2018 and May 17th, 2022.
Cervical Cancer Screening
166 female BRIDGE patients seen between 2018 and 2022 were eligible for cervical cancer screening according to the 2018 USPSTF guidelines (Table 1). The median age of these women was 48 years old. Of patients with documented preferred languages, 84% were Spanish speaking only. Most patients (73.5%) identified as Hispanic or Latino. Of patients with documented methods of cervical cancer screening for the prior screening event, the majority (73%) received co-testing, comprised of Pap smear cytology plus high-risk HPV screening. 94% of patients had screenings performed at BRIDGE Clinic, with the remaining performed at other sites. One patient was HIV positive. Five screenings bore atypical squamous cells. Of these, each had appropriate follow-up pap or colposcopy, and one yielded a result of grade 3 carcinoma in situ (CIN3), which was referred to a collaborating cancer center for follow-up care.
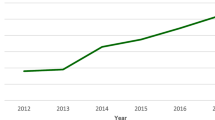
Overall, 92% of eligible women were UTD on screenings between 2018 and 2022. Those who were not were either no-shows to gynecology appointments, had not made gynecological appointments, or refused gynecological care. In 2018, 81.3% were UTD; in 2019, 90.9% of eligible female patients seen were UTD; in 2020, 83.3% were UTD; in 2021, 93.3% were UTD; in 2022, 93.8% were UTD (Fig. 1).
Breast Cancer Screening
143 women seen between 2018 and 2022 met criteria for breast cancer screening according to the ACS guidelines (Table 2). The median age was 53 years old; 16.1% were within the 40–44 age range, 41.3% were between 45 and 54 years old, and 42.7% were between 55 and 75 years old. Of the women for whom a language preference was indicated, 87% were Spanish speaking only. The majority (83.2%) of mammograms were performed at Moffitt Cancer Center. Of eligible women, 13.3% had a known family history of breast cancer.
Overall, 79.7% of eligible women were UTD with mammography between 2018 and 2022. Abnormal scans were followed with appropriate biopsy or other imaging. In 2018, 66.7% of the 15 eligible women were UTD, with all scans revealing benign findings (BIRADS1 or 2). In 2019, 62.5% of the 8 eligible women seen were UTD. One scan returned BIRADS4, but biopsy revealed benign fibro-adenomatous changes. In 2020, 91.7% of the 12 eligible women seen were UTD, with all prior scans returning benign findings. In 2021, 73.1% of the 26 eligible seen were UTD with scans revealing benign findings. In 2022, 84.1% of the 82 eligible women seen were UTD, with investigations in a 62-year-old female revealing ductal carcinoma in situ (Fig. 1).
By age group, 73.9% of the 23 females within the 40–44-year-old range were UTD with breast cancer screening according to ACS guidelines. 74.6% of the 59 women 45–54 years old were UTD with annual mammograms, and 86.9% of the 61 women 55–75 years old were UTD with biennial mammograms.
Discussion
Women’s health maintenance screenings are an essential driver of the lower rates of breast and cervical cancer seen in recent decades [7, 14]. A consequence of the lower screening rates seen in those of disadvantaged socioeconomic backgrounds [11, 17] is greater mortality in such populations from these cancers [12, 13, 19, 20]. Free clinics providing these services can intervene to rectify this inequity. We demonstrated how the BRIDGE clinic was able to maintain adequate screenings before, during, and after the COVID-19 pandemic at proportions that exceeded national averages. In 2018, of all women eligible for pap smears in the United States, the rate of those with updated screenings was 68.1% [9] and this was slightly lower for women living below the 200% poverty line, of which 64.1% were UTD with screenings [9]. The BRIDGE clinic surpassed this national average in 2018, reaching 81.3% of women UTD with cervical cancer screening. The proportion of women updated with screening mammography also superseded national averages in 2018 [21]. In 2019, nationally, 73.5% of women were UTD with cervical cancer screenings, and again this was slightly lower for women below 200% poverty line at 64.2% [22], while the BRIDGE clinic reached 90.9% adherence for cervical cancer screenings. Breast cancer screenings at BRIDGE in 2019 were 62.5%, similar to the national averages of individuals below the 200% poverty level at 68.3% [23].
While national data is not yet available for cervical and breast cancer screenings in 2020, regional studies report declines in screenings, and deficits have been documented in all types of cancer screenings [2]. A retrospective study of changes in cervical cancer screening rates among 1.5 million women in the Kaiser Permanente Southern California Network before, during, and after stay-at-home orders were instituted during 2020 revealed a 78% decrease in cervical cancer screenings for women between 21 and 29 years old, and 82% decrease in rates for women 30–65 years old [24]. Furthermore, the CDC’s National Breast and Cervical Cancer Early Detection Program saw an 87% decrease in the number of mammograms performed during 2020 compared to averages in the preceding five years [25]. A global meta-analysis published during 2021 containing data on screening for breast and cervical cancer found significant declines in screening incidences when comparing rates before and during the pandemic [26]. Despite these national trends, BRIDGE has continued to show maintenance of high levels of completed screenings.
We expect that BRIDGE will continue to surpass national averages due to the diligent health maintenance efforts and monthly gynecological-focused clinic nights. The propitious screening rates at the BRIDGE clinic during the pandemic may be a composite of multiple factors. The student-run free clinic closed for only three months between March 2020 and June 2020, and monthly gynecology clinic nights resumed upon re-opening, in addition to the regular schedule of two to three gynecology patients seen by the volunteer gynecologist each week. Furthermore, efforts by the volunteer gynecologist at BRIDGE ensured that before and after the pandemic, patients were caught up with screenings. The practice of performing co-test cytology and high-risk HPV for patients over 30 years old may also contribute to the auspicious screening retention due to the 5-year screening interval that confers some flexibility to changes in schedule, whereas screening at more frequent intervals would be significantly impacted by clinic closures.
Future Directions
The 2020 update from the American Cancer Society regarding cervical cancer screening recommended HPV testing alone as the method of screening starting at 25 years old, every five years [27]. This is based on data showing improved sensitivity and negative predictive value of HPV testing compared to cytology alone [28, 29]. Adopting this screening method may be a way to decrease the number of tests and appointments, identify which patients need more frequent follow-ups, and ensure longer-term protection after negative tests. Self-sampling for HPV positivity has been seen as an accurate collection method and may be an alternative way to mitigate barriers to cervical cancer screening [30, 31].
A nationwide survey published in 2020 investigated the factors associated with cervical cancer screenings and revealed that having an income under $30,000, a low level of knowledge of HPV, and lack of insurance were significant barriers to screening [32]. Racial disparities were also seen, as white women were 2.39 times as likely to obtain screenings than black women. Socioeconomic disparities in breast cancer screenings are also seen, with factors such as lack of access or insurance, transportation, and delays from the COVID-19 pandemic all contributing to a lower likelihood of screening mammography receipt [33, 34] as well as a disproportionate impact of breast cancer incidence and mortality in minorities [35, 36]. Free clinics meet these needs and intervene to temper disparities, increase access, and educate patients on the importance of screening. Additionally, given the possibility of future shifts to HPV-based testing alone, education will be important in reducing the stigma of screening and increasing acceptance [37] as this method has greater long-term protection and fewer visits for individuals with negative results [27].
Conclusions
Despite national trends showing screening deficits during the pandemic, the BRIDGE clinic has continued to maintain high levels of screenings. Efforts to understand and identify the barriers to women’s cancer screenings will continue. While student-run free clinics can ameliorate the disparity seen in women of low incomes without insurance for cervical cancer, it is also important to incorporate education on HPV and the necessity of screenings to ensure that these women will take advantage of gynecological services. Similarly, for screening mammography, efforts should focus on educating patients on the necessity of receiving screenings, individually working with patients and social work services to mediate logistic barriers, and vigilance on the part of clinics to identify patients whose screenings have lapsed to rebound from pandemic-era delays and equilibrate out of inequities in women’s health maintenance.
References
Becker, N. V., Moniz, M. H., Tipirneni, R., Dalton, V. K., & Ayanian, J. Z. (2021). Utilization of women’s Preventive Health Services during the COVID-19 pandemic. JAMA Health Forum, 2(7), e211408–e211408. https://doi.org/10.1001/jamahealthforum.2021.1408.
Joung, R. H., Nelson, H., Mullett, T. W., Kurtzman, S. H., Shafir, S., Harris, J. B., Yao, K. A., Brajcich, B. C., Bilimoria, K. Y., & Cance, W. G. (2022). Jun 1). A national quality improvement study identifying and addressing cancer screening deficits due to the COVID-19 pandemic. Cancer, 128(11), 2119–2125. https://doi.org/10.1002/cncr.34157.
Cervix Uteri Recent trends in SEER Age-adjusted incidence rates, 2000–2019. Surveillance, Epidemiology, and End Results Program. Retrieved May 9, 2022, from https://seer.cancer.gov/statistics-network/explorer/application.html?site=57&data_type=1&graph_type=2&compareBy=race&chk_race_1=1&rate_type=2&hdn_sex=3&age_range=1&stage=101&advopt_precision=1&advopt_show_ci=on&advopt_display=2
Arbyn, M., Smith, S. B., Temin, S., Sultana, F., & Castle, P. (2018, Dec 5). Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. Bmj, 363, k4823. https://doi.org/10.1136/bmj.k4823
Shanmugasundaram, S., & You, J. (2017). Aug 18). Targeting Persistent Human Papillomavirus infection. Viruses, 9(8), https://doi.org/10.3390/v9080229.
Howlader, N., Krapcho, N. A., Miller, M., Brest, D., Yu, A., Ruhl, M., Tatalovich, J., Mariotto, Z., Lewis, A., Chen, D. R., Feuer, H. S., & Cronin, E. J. KA (Eds.). (1975–2017). SEER Cancer Statistics Review, National Cancer Institute. https://seer.cancer.gov/csr/1975_2017/
Safaeian, M., Solomon, D., & Castle, P. E. (2007). Cervical cancer prevention–cervical screening: science in evolution. Obstetrics and gynecology clinics of North America, 34(4), 739–ix. https://doi.org/10.1016/j.ogc.2007.09.004.
Force, U. P. S. T. (2018). Screening for cervical Cancer: US Preventive Services Task Force Recommendation Statement. Journal Of The American Medical Association, 320(7), 674–686. https://doi.org/10.1001/jama.2018.10897.
National Center for Health Statistics. Health, United States, 2019. Table 34. https://doi.org/https://www.cdc.gov/nchs/hus/contents2019.htm
MacLaughlin, K. L., Jacobson, R. M., Breitkopf, R., Wilson, C., Jacobson, P. M., Fan, D. J., St. Sauver, C., J. L., & Rutten, L. J. F. (2019). 2019/02/01). Trends over Time in Pap and Pap-HPV cotesting for Cervical Cancer Screening. Journal of Women’s Health, 28(2), 244–249. https://doi.org/10.1089/jwh.2018.7380.
Buskwofie, A., David-West, G., & Clare, C. A. (2020). 2020/04/01/). A review of Cervical Cancer: incidence and disparities. Journal of the National Medical Association, 112(2), 229–232. https://doi.org/10.1016/j.jnma.2020.03.002.
Simard, E. P., Fedewa, S., Ma, J., Siegel, R., & Jemal, A. (2012). Widening socioeconomic disparities in cervical cancer mortality among women in 26 states, 1993–2007. Cancer, 118(20), 5110–5116. https://doi.org/10.1002/cncr.27606.
Akers, A. Y., Newmann, S. J., & Smith, J. S. (2007). 2007/05/01/). Factors underlying disparities in Cervical Cancer incidence, screening, and treatment in the United States. Current Problems in Cancer, 31(3), 157–181. https://doi.org/10.1016/j.currproblcancer.2007.01.001.
Berry, D. A., Cronin, K. A., Plevritis, S. K., Fryback, D. G., Clarke, L., Zelen, M., Mandelblatt, J. S., Yakovlev, A. Y., Habbema, J. D., & Feuer, E. J. (2005, Oct 27). Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med, 353(17), 1784–1792. https://doi.org/10.1056/NEJMoa050518
Oeffinger, K. C., Fontham, E. T. H., Etzioni, R., Herzig, A., Michaelson, J. S., Shih, Y. C. T., Walter, L. C., Church, T. R., Flowers, C. R., LaMonte, S. J., Wolf, A. M. D., DeSantis, C., Lortet-Tieulent, J., Andrews, K., Manassaram-Baptiste, D., Saslow, D., Smith, R. A., Brawley, O. W., & Wender, R. (2015). Breast Cancer screening for women at average risk: 2015 Guideline Update from the American Cancer Society. Journal Of The American Medical Association, 314(15), 1599–1614. https://doi.org/10.1001/jama.2015.12783.
Cancer, F. (2022). & Fig. 2022 Retrieved May 17, from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf
Hall, I. J., Sabatino, T. F., Thompson, S. A., Graubard, T. D., & Breen, B. I. (2018). N. Patterns and Trends in Cancer Screening in the United States Retrieved July 2, 2022, from https://www.cdc.gov/pcd/issues/2018/17_0465.htm
The American Cancer Society guidelines for the prevention and early detection of cervical cancer American Cancer Society. Retrieved July 2, 2022 from https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html#references
Byers, T. E., Wolf, H. J., Bauer, K. R., Bolick-Aldrich, S., Chen, V. W., Finch, J. L., Fulton, J. P., Schymura, M. J., Shen, T., Van Heest, S., & Yin, X. (2008, Aug 1). The impact of socioeconomic status on survival after cancer in the United States: findings from the National Program of Cancer Registries Patterns of Care Study. Cancer, 113(3), 582–591. https://doi.org/10.1002/cncr.23567
Sprague, B. L., Trentham-Dietz, A., Gangnon, R. E., Ramchandani, R., Hampton, J. M., Robert, S. A., Remington, P. L., & Newcomb, P. A. (2011, Apr 1). Socioeconomic status and survival after an invasive breast cancer diagnosis. Cancer, 117(7), 1542–1551. https://doi.org/10.1002/cncr.25589
Sabatino, S. A., Thompson, T. D., White, M. C., et al. (2021). Cancer Screening Test receipt — United States, 2018. Mmwr. Morbidity And Mortality Weekly Report, 70, 29–35.
NIH Online summary of US cancer control measures. Cervical Cancer Screening, 2019 Retrieved August 9 (2022). from https://progressreport.cancer.gov/detection/cervical_cancer
NIH Online summary of US cancer control measures. Breast Cancer Screening (2019). Retrieved August 9, 2022, from https://progressreport.cancer.gov/detection/breast_cancer
Miller, M. J., & Qin, X. L. (2021). Impact of COVID-19 on Cervical Cancer Screening Rates among Women aged 21–65 years in a large Integrated Health Care System — Southern California, January 1–September 30, 2019, and January 1–September 30, 2020. Mmwr. Morbidity And Mortality Weekly Report, 70, 109–113. https://doi.org/10.15585/mmwr.mm7004a1.
DeGroff, A., Miller, J., Sharma, K., Sun, J., Helsel, W., Kammerer, W., Rockwell, T., Sheu, A., Melillo, S., Uhd, J., Kenney, K., Wong, F., Saraiya, M., & Richardson, L. C. (2021). 2021/10/01/). COVID-19 impact on screening test volume through the national breast and cervical Cancer early detection program, January–June 2020, in the United States. Preventive Medicine, 151, 106559. https://doi.org/10.1016/j.ypmed.2021.106559.
Mayo, M., Potugari, B., Bzeih, R., Scheidel, C., Carrera, C., & Shellenberger, R. A. (2021). 2021/12/01/). Cancer Screening During the COVID-19 Pandemic: A Systematic Review and Meta-analysis. Mayo Clinic Proceedings: Innovations, Quality & Outcomes, 5(6), 1109–1117. https://doi.org/10.1016/j.mayocpiqo.2021.10.003
Fontham, E. T. H., Wolf, A. M. D., Church, T. R., Etzioni, R., Flowers, C. R., Herzig, A., Guerra, C. E., Oeffinger, K. C., Shih, Y. C. T., Walter, L. C., Kim, J. J., Andrews, K. S., DeSantis, C. E., Fedewa, S. A., Manassaram-Baptiste, D., Saslow, D., Wender, R. C., & Smith, R. A. (2020). Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA: A Cancer Journal for Clinicians, 70(5), 321–346. https://doi.org/10.3322/caac.21628.
Ogilvie, G. S., van Niekerk, D. J., Krajden, M., Martin, R. E., Ehlen, T. G., Ceballos, K., Peacock, S. J., Smith, L. W., Kan, L., Cook, D. A., Mei, W., Stuart, G. C., Franco, E. L., & Coldman, A. J. (2010). Mar 24). A randomized controlled trial of human papillomavirus (HPV) testing for cervical cancer screening: trial design and preliminary results (HPV FOCAL Trial). Bmc Cancer, 10, 111. https://doi.org/10.1186/1471-2407-10-111.
Castle, P. E., Kinney, W. K., Xue, X., Cheung, L. C., Gage, J. C., Zhao, F. H., Fetterman, B., Poitras, N. E., Lorey, T. S., Wentzensen, N., Katki, H. A., & Schiffman, M. (2018). Jan 2). Effect of several negative Rounds of Human Papillomavirus and Cytology co-testing on Safety Against Cervical Cancer: an Observational Cohort Study. Annals Of Internal Medicine, 168(1), 20–29. https://doi.org/10.7326/m17-1609.
Arbyn, M., Smith, S. B., Temin, S., Sultana, F., & Castle, P. (2018, Dec 5). Detecting cervical precancer and reaching underscreened women by using HPV testing on self samples: updated meta-analyses. Bmj, 363, k4823. https://doi.org/10.1136/bmj.k4823
Wentzensen, N., Clarke, M. A., & Perkins, R. B. (2021). Oct). Impact of COVID-19 on cervical cancer screening: Challenges and opportunities to improving resilience and reduce disparities. Preventive Medicine, 151, 106596. https://doi.org/10.1016/j.ypmed.2021.106596.
Johnson, N. L., Head, K. J., Scott, S. F., & Zimet, G. D. (2020). Jul/Aug). Persistent disparities in Cervical Cancer Screening Uptake: knowledge and sociodemographic determinants of Papanicolaou and Human Papillomavirus Testing among Women in the United States. Public Health Reports, 135(4), 483–491. https://doi.org/10.1177/0033354920925094.
Satish, T., Raghunathan, R., Prigoff, J. G., Wright, J. D., Hillyer, G. A., Trivedi, M. S., Kalinsky, K., Crew, K. D., Hershman, D. L., & Accordino, M. K. (2021). Aug). Care Delivery Impact of the COVID-19 pandemic on breast Cancer Care. JCO Oncol Pract, 17(8), e1215–e1224. https://doi.org/10.1200/op.20.01062.
Tsapatsaris, A., Babagbemi, K., & Reichman, M. B. (2022, Feb). Barriers to breast cancer screening are worsened amidst COVID-19 pandemic: a review. Clinical Imaging, 82, 224–227. https://doi.org/10.1016/j.clinimag.2021.11.025.
Newman, L. A. (2017). Oct). Breast Cancer disparities: socioeconomic factors versus Biology. Annals Of Surgical Oncology, 24(10), 2869–2875. https://doi.org/10.1245/s10434-017-5977-1.
Rauscher, G. H., Allgood, K. L., Whitman, S., & Conant, E. (2012, Feb). Disparities in screening mammography services by race/ethnicity and health insurance. Journal Of Women’S Health (2002), 21(2), 154–160. https://doi.org/10.1089/jwh.2010.2415.
Nothacker, J., Nury, E., Mathieu, M., Raatz, H., Meerpohl, J., & Schmucker, C. (2022). Women’s attitudes towards a human papillomavirus-based cervical cancer screening strategy: a systematic review. BMJ Sexual & Reproductive Health, 0805. https://doi.org/10.1136/bmjsrh-2022-201515.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
GJ drafted the manuscript; GJ, CM, YB performed data collection; GJ and SL contributed to literature review; LG and EG critically revised final draft. All authors significantly contributed to both intellectual development of the project and reviewing the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Johnson, G., Miquel-Chambers, C., Blas, Y. et al. Women’s Health Maintenance Efforts at a Student-Run Free Clinic in South Florida Exceeded National Trends During the COVID-19 Pandemic. J Community Health 48, 501–507 (2023). https://doi.org/10.1007/s10900-023-01190-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-023-01190-z