Abstract
Food insecurity is linked with poor physical and mental health outcomes, including anxiety, depression and stress. Rural residents in particular face unique challenges obtaining healthy food; the COVID-19 pandemic exacerbated the relationship between food insecurity and mental health outcomes. This study examines the relationship between food insecurity and stress, and the moderating influence of household characteristics, neighborhood social environment and food environment on this relationship, using a sample of 630 rural South Carolina (SC) residents during COVID-19. Two measures of stress were used in this study: current levels of stress and changes in stress since COVID-19. Results showed a gradient pattern between food insecurity and stress: rural residents with high food insecurity were 6.1 times more likely and those with moderate food insecurity were 3.4 times more likely to report higher level of general stress than those with low food insecurity; rural residents with high food insecurity were 3.3 times more likely and those with moderate food insecurity were 2.0 times more likely to report greater increase in stress after COVID-19 than those with low food insecurity. Neighborhood social environment and food environment provided a buffering effect on the relationship between food insecurity and stress. A stronger social environment after COVID-19 and higher levels of easiness in food access mitigated the negative impacts of food insecurity on stress. Efforts to ameliorate food insecurity should address these broader contextual variables, involving community-level factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sufficient access to sustaining, nutritious food is a basic physiological need, and yet millions of individuals in the United States are not able to meet this basic need. Food insecurity is defined as the limited or uncertain availability of nutritionally adequate and safe foods, or “limited ability to acquire acceptable foods in socially acceptable ways” [1]. Lack of food security poses significant challenges over time, leading to malnutrition, extreme chronic stress, poor mental and physical health, and a myriad of chronic diseases [2,3,4].
Rural populations are especially vulnerable to food insecurity. While the national food insecurity rate dropped to its lowest in decades to 10.8% in 2018, the food insecurity rates of rural populations remained above the national average at 12.7% [5]. Economic instability, low healthy food access, transportation barriers, and financial insecurity pose barriers to individuals living in rural communities, making it more difficult for them to maintain food security and live healthy lifestyles. The COVID-19 pandemic intensified food insecurity throughout the rural United States and introduced or reinforced stressors experienced at the household level. Many people who have been most impacted by the pandemic were food insecure or at risk of food insecurity before COVID-19 and have since faced greater hardship, resulting in food insecurity rates that doubled nationwide and tripled among households with children [6, 7, 8].
According to stress process theory, negative life events are major stressors that motivate efforts to cope with behavioral demands and with the emotional reactions evoked by them [9, 10]. Arguably, the burden of high or marginal food insecurity is a major stressor as it is a type of deprivation of basic human needs. The literature suggests a clear relationship between food insecurity and stress, especially for rural populations [11,12,13,14,15]. Further, Liu et al. (2014) determine that mental distress acts as a mediator in the relationship between housing/food insecurity and sleep insufficiency. Therefore, food insecurity has been found to not only indirectly lead to stress, but stress can in turn moderate the relationship(s) between food insecurity and biological factors such as weight gain and sleep quality.
In accordance with stress process theory, the buffering hypothesis suggests that psychosocial resources can mitigate the negative impact of stressors on psychological well-being [18, 19]. Household factors, including marital status, presence of children in the home, and household income, influence the risk of stress among adults caused by food security status [17, 20, 21]. Marriage has been consistently identified as a protective factor for health and well-being, including greater emotional and financial support [22, 23]. In families with children, adults may experience challenges associated with accessing and managing food that generate higher levels of stress, psychological distress, and emotional responses, and ultimately impact parenting practices and child development, compared to those who do not experience such challenges [24,25,26,27]. Those living in low-income households may experience greater challenges meeting the basic needs of housing, food, and transportation, work-family conflict, job control, and inequity in responsibility for domestic work for women, leading to increased vulnerability to feelings of distress [16, 20, 21].
Much research on food insecurity focuses on individual and household determinants of food insecurity; however, it is important to also consider community-level variables that provide context related to the physical and social community environments [28,29,30]. This approach aligns with the social determinants of health (SDOH) perspective that addresses “the conditions in which people are born, grow, live, work and age” [31]. SDOH include community-level factors such as community stress, food supply, food access, social cohesion, trust in one’s neighbors and the presence of informal networks and formal social support mechanisms, each of which helps to reduce the impact of food insecurity on families [30, 32,33,34,35,36,37].
Several studies have examined the impact of the COVID-19 pandemic on the relationship between food security and stress. From the early stages of the COVID-19 pandemic, food insecure adults—including those who worried about food accessibility—were more likely to experience depression, anxiety, stress and suicidal thoughts or feelings, compared to those who were food secure [38,39,40]. Mental health issues are particularly challenging for rural residents. Research suggests that nearly one-fifth of rural residents in the U.S. have a mental illness, yet these individuals have less access to necessary medical care compared to urban counterparts [41]. However, research on how food insecurity contributes to mental health disparity during the COVID pandemic among rural residents is limited.
This study investigates the relationship between food insecurity, household and community environments, and levels of stress among residents in nine counties in rural South Carolina during COVID-19 by investigating two research questions: (1) whether food insecurity is positively associated with current stress level and increase in stress after COVID-19 among rural adults; and (2) whether the association of food insecurity with stress and increase in stress is buffered by the absence of minor children in the household, marriage, higher income, and stronger neighborhood social environment and food environment. This study extends previous research by differentiating marginal and high food insecurity and by investigating what factors moderate the effects of food insecurity on stress for rural residents during the pandemic. Both current level of stress and change in stress after the onset of the COVID-19 pandemic are examined in order to provide new information on the pandemic’s impact on people’s psychological well-being.
Methods
Data Collection
The survey examined food access, physical activity, and neighborhood environments across nine rural counties in South Carolina. Counties were deemed rural if the county population was less than 50,000 or the county was in a micropolitan core based statistical area. Eligible participants were ≥ 18 years old and current resident of the included counties. Data collection occurred in two phases, using two modalities. Telephone interviews were conducted from August 2020 to March 2021 and in-person surveys were administered in July 2021. Community partners helped to publicize the study throughout the partner communities. Trained university students administered the survey, verbally obtained consent, read survey items, and recorded responses using Qualtrics software™. Upon survey completion, respondents were mailed a $10 incentive card and printed informed consent form. Institutional Review Board approval was obtained from BLINDED INSTITUTION (IRB # 2020 − 188). Across the nine counties, 1,115 potential survey respondents were contacted, of whom 713 completed the survey, for a 64% response rate. In sum, 580 surveys were completed via telephone and 133 were completed in person. After list-wise deletion of missing cases, this study included 630 respondents.
Measures
Overall Stress
The overall stress level was measured with a question developed by the team based on existing literature [14]. Respondents were asked “Thinking about the amount of stress in your life, would you say that most days are…,” choosing from a 5-point scale, ranging from “not at all stressful” to “very stressful.”
Change in Stress
Following the inquiry about the amount of overall stress in the respondent’s life, respondents were asked to compare their level of stress before the COVID-19 pandemic to their stress level at the time of the survey. Respondents were asked “How was your stress level before the COVID-19 pandemic as compared to now?” and the 5-point ordinal response scale ranged from “much less stressful now than before COVID-19” to “much more stressful now than before COVID-19.”
Food Insecurity
The following items from the USDA’s (2012) U.S. Household Food Security Survey were used to assess food security status in the three months prior to the survey:
-
1.
The food that I bought just didn’t last and I didn’t have money to get more. (Affirmative response = Sometimes or often true)
-
2.
I couldn’t afford to eat balanced meals. (Affirmative response = Sometimes or often true)
-
3.
Did you ever cut the size of your meals or skip meals because there wasn’t enough money for food? (Affirmative response = Yes)
-
4.
How often did this happen? (Affirmative response = almost every day or 2–3 days)
-
5.
In the last three months, did you ever eat less than you felt you should because there wasn’t enough money for food? (Affirmative response = Yes).
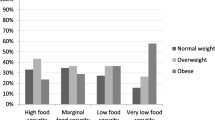
Based on the sum of affirmative responses to these five items, households were classified as experiencing low (0 or 1 affirmative response), moderate (2, 3 or 4 affirmative responses) or high food insecurity (5 affirmative responses). This approach to categorizing various levels of food insecurity is similar to that used in the USDA’s abbreviated measure of food insecurity [43].
Household Characteristics
The survey included the following household characteristics, which were used in the current study: marital status (married/partnered, widowed, divorced/separated, and never married), whether children under age 18 were living in the household, and household income (less than $20k, $20k-$35k, $35k-$50k, $50k-$75k, more than $75k and a missing income category for respondents who did not report household income).
Neighborhood Social Environment
The measure of neighborhood social environment, as a subset of broader SDOH, was created by combining respondents’ answers to the following three survey items, modeled after Sampson et al.’s (1997) research on sense of belonging, social cohesion, and collective efficacy:
-
Sense of belonging: How would you describe your sense of belonging to your local community? With possible responses ranging on a 4-point scale from “very weak” to “very strong.”
-
Social cohesion: How strongly would you agree or disagree (on a 4-point scale ranging from “strongly disagree” to “strongly agree”) that: (1) people around here are willing to help their neighbors; (2) this is a close-knit neighborhood; (3) people in this neighborhood can be trusted; (4) people in this neighborhood generally don’t get along with one another; (5) people in this neighborhood do not share the same values.
-
Collective efficacy: How likely would you say (on a 4-point scale ranging from “very unlikely” to “very likely”) it is that neighbors know each other well enough that they can be counted on to intervene in various ways if: (1) children were skipping school and hanging out on a street corner; (2) children were spray-painting graffiti on a local building; (3) children were showing disrespect to an adult; (4) a fight broke out in front of their house; (5) the fire station or other community resource, such as park or community center, closest to their home was being threatened with budget cuts.
Although these items may be somewhat conceptually different measures of community, they were highly correlated with one another. Therefore, similar to Sampson et al. (1997), the measures were combined into one measure of the neighborhood social environment by averaging scores on these items after reverse-coding the negatively worded questions; the scores ranged from 1 to 4 with higher values associated with perceptions of a stronger neighborhood social environment. The value for Cronbach’s Alpha was 0.85.
Respondents were also asked how likely people in their neighborhood were to (1) help their neighbors and (2) intervene when necessary before the COVID-19 pandemic compared to now, with responses ranging (on a 5-point scale) from “much less likely now than before COVID-19” to “much more likely now than before COVID-19.” Responses to these two items were averaged to create an index measuring change in neighborhood social environment after the onset of COVID-19 ranging from 1 to 5 with higher values indicating perceptions of a stronger neighborhood social environment since the COVID-19 onset (Cronbach’s alpha = 0.74).
Food Environment
Respondents were asked how easy it was to access (purchase or get) each of the following items in their local community: fresh fruits and vegetables; locally grown or home-made food items; food support services; farmers’ market or produce stands; and affordable food. The 3-point response options to each item included not easy, somewhat easy, and very easy. Because factor analysis showed that answers to these five items loaded on one single factor which explains 44% of the variances, the scores on these items were averaged to create an index on ease of food access which ranged 1 to 3 with higher scores indicating easier access. Respondents were also asked how their access to fresh, locally grown food in their community was different before the COVID-19 pandemic compared to now, and the 4-point response scale ranged from 1 “very different” to 4 “exactly the same.”
Covariates
Demographic variables included gender (male, female), age (18–44, 45–64, and 65+), race (White, Black, and other races), and employment status (employed, unemployed, retired, and unable to work).
Analytic Procedures
Descriptive statistics for all variables were calculated first for all respondents and then for respondents in the three food insecurity categories separately. Chi-square tests for categorical variables and ANOVA tests for continuous variables were used to examine whether distributions of these variables significant differ by levels of food insecurity. Because overall stress and change in stress before and after the COVID-19 were ordinal variables, an ordinal logistic regression was used to examine the effects of food security status on individuals’ overall stress level and change in stress level since COVID-19. For each stress outcome, we first estimated a model which included household characteristics, neighborhood social environment and its change since COVID-19, food environment and its change since COVID-19, demographic covariates, and food insecurity to examine whether food insecurity was associated with each stress outcome after other individual, household and community characteristics were controlled for. Then, the interaction effects of food insecurity with household characteristics and with neighborhood social environment and food environment measures were tested. For clarity and ease of interpretation, these interaction terms were entered separately. We also estimated a model with all these interaction terms included in one model which produced similar results. All statistical analyses in this study were performed using Stata 14 [45].
Results
Descriptive statistics are represented in Table 1. The respondents were mostly female (84%). More than half of the respondents were Black (56%) and about 40% were white. About 45% were married, 32% had children under 18 in the household, 44% were employed, and 58% had a family income less than $35,000. Regarding food insecurity status, 69% of respondents were categorized as experiencing low food insecurity, 20% experienced moderate food insecurity, and 11% experienced high food insecurity. On a scale from 1 to 5, the average overall stress level was 2.83 and the average change in stress since COVID-19 was 3.44, demonstrating a trend toward experiencing more stress during the pandemic than before the pandemic. On a scale from 1 to 4, the average neighborhood social environment score was 2.99 and on a scale from 1 to 5, the average change in neighborhood social environment was 3.08. On a scale from 1 to 3, the average ease of food access was 2.21, and on a scale from 1 (very different) to 4 (exactly the same), the average score on change in food access since COVID-19 was 2.79.
In looking at the differences by level of food insecurity, the three food insecurity groups varied significantly in overall stress level, change in stress since COVID-19, neighborhood social environment, ease of food access, and similarity in access to fresh food before and after COVID-19. Compared to those with low food insecurity, respondents with high food insecurity reported higher levels of overall stress, increased stress since COVID-19 onset, weaker neighborhood social environment, more difficult food access, and a greater change in access to fresh food since COVID-19 onset. Additionally, the three food insecurity groups significantly differed on all sociodemographic characteristics except gender; those with higher food insecurity levels tended to be younger, Black, unmarried and unemployed or not able to work and to have minor children in the household and to have a lower family income.
Food Insecurity and Overall Stress
Results from ordered logistic regression on overall stress level are presented in Table 2. After controlling for sociodemographic characteristics, household characteristics, neighborhood social environment, change in neighborhood social environment since the onset of COVID-19, and ease of food access, food insecurity status measures were significantly associated with overall stress level (Model 1). Respondents with moderate food insecurity were 3.36 times as likely and high food insecurity were 6.09 times as likely to report higher overall stress compared to low food insecurity respondents. Among household and community characteristics, the results show that widowed (OR = 0.55) and divorced/separated (OR = 0.52) respondents had lower levels of overall stress than those who were married. Neighborhood social environment (OR = 0.55) and ease of food access (OR = 0.66) were negatively associated with overall stress level. As for individual sociodemographic variables, female respondents had higher levels of overall stress than male respondents while Blacks and retired respondents had lower levels of overall stress than white and employed respondents.
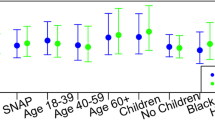
Models 2 to 5 report the interaction effects of food insecurity with presence of minor children in the household and neighborhood social environment and food environment measures on overall stress. There was a significant negative interaction between high level of food insecurity and presence of minor children in the household (Model 2, OR = 0.35); there was less difference in stress level between those with high food insecurity and those with low food insecurity if there were minor children in the household. Model 3 shows that there was no significant interaction between food insecurity and neighborhood social environment. However, Model 4 shows a significant negative interaction between moderate level of food insecurity and change in neighborhood social environment after COVID-19 (OR = 0.5); there was less difference in stress level between those with moderate food insecurity and those with low food insecurity when neighborhood social environment became stronger after COVID-19. Model 5 shows a marginally significant negative interaction between high level of food insecurity and ease of food access (OR = 0.38); there was less difference in stress level between those with high food insecurity and those with low food insecurity with increasing easiness in food access.
Food Insecurity and Change in Stress Since COVID-19
Results from ordered logistic regression on change in stress level after the onset of COVID-19 are presented in Table 3. After controlling for sociodemographic characteristics, household characteristics, neighborhood social environment, change in neighborhood social environment since COVID-19, ease of food access, and change in easiness of food access since COVID-19, food insecurity status measures were significantly associated with change in stress level since COVID-19 (Model 1). Respondents with moderate food insecurity were 1.97 times as likely and those with high level of food insecurity were 3.27 times as likely to report greater increase in stress since COVID-19, compared to those with low level of food insecurity. Among household and community characteristics, the results show that widowed respondents were less likely to have greater increase in stress after COVID-19. Easiness in food access (OR = 0.56) and similarity in access to fresh food before and after COVID-19 (OR = 0.77) were negatively associated with increase in stress after COVID-19. As for individual demographic characteristics, Black respondents had lower increases in stress after COVID-19 than white respondents (OR = 0.73).
Models 2 to 6 estimated the interaction effects of food insecurity with presence of minor children in the household and neighborhood social environment and food environment measures on change in stress after COVID-19. While there was no significant interaction effect of food insecurity with presence of minor children in the household and neighborhood social environment, four interaction terms were significant or marginally significant and negative, including the interactions of moderate food insecurity with change in neighborhood social environment (Model 4, OR = 0.73) and with change in easiness of food access (Model 6, OR = 0.67) and the interactions of high food insecurity with change in neighborhood social environment (Model 4, OR = 0.37) and with easiness of food access (Model 5, OR = 0.40). More specifically, there was less difference in stress level change after COVID-19 between those with moderate or high food insecurity and those with low food insecurity when the strength of neighborhood social environment after COVID-19 increased more. There was less difference in stress level change after COVID-19 between those with high food insecurity and those with low food insecurity with increasing easiness of food access. There was less difference in stress level change after COVID-19 between those with moderate food insecurity and those with low food insecurity if there was less change in easiness of food access before and after COVID-19.
For both current overall stress level and change in stress since COVID-19, the interactions between food insecurity and other household characteristics were estimated, including marital status and household income, and these interactions were not significant for either current stress level or change in stress (not shown). Access to fresh food before and after COVID-19 was not a significant predictor of overall stress level and the interaction terms between this variable and food insecurity measures were also not significant, and thus it was not included in the models for overall stress presented in Table 2.
Discussion
The first research goal aimed to determine whether food insecurity is positively associated with current stress level and change in stress after COVID-19 among adults living in rural counties and this study found strong support for this relationship. The data show that rural residents with high food insecurity reported the highest level of general stress and the greatest increase in stress after COVID-19 and those with low food insecurity reported the lowest levels on both measures of stress.
Our second goal was to examine the moderating effects of household, community and food access variables on the relationship between food insecurity and stress. The evidence for the moderating effect of household characteristics is mixed. While several measures of social and food environments were in the expected direction, the effect of children on the relationship between food insecurity and general stress was unexpected, and the results show no moderating effects of marital status and family income. The finding that the relationship between food insecurity and general stress was not intensified when children are present in the home is inconsistent with the literature that parents in food insecure households—including those who are marginally food insecure—experience significantly higher levels of stress and associated emotions of shame, guilt, stigma, and sadness, compared to parents of food secure households [25, 2627, 42, 48]. This may be because parents included in this study had already reached a threshold of significant stress according to the stress measure used, or because the sample was skewed towards households with children. It is also possible that the influence of children on the relationship between food insecurity and stress may have been somewhat altered during the pandemic in new ways. For instance, many families were provided with meals for their children in ways that went far beyond prior food provisioning programs for children. Regarding the insignificant interaction effect between food access and household income, it is possible that factors beyond finances drove food access and associated stress during COVID-19. Further research is needed to understand the intricate relationship between stress levels and food insecurity among rural households with children.
When assessing the relationship between food insecurity and stress, it is also essential to consider how families obtain food, especially during COVID-19 when many families have struggled to access healthy foods [35]. Federal food assistance programs, local support, and informal subsistence sources improved families’ access to nutritional, affordable food and to resources that alleviate stress [36, 49]. In the height of the pandemic, schools across the country provided food assistance among families at risk of experiencing food insecurity to offset increased vulnerabilities associated with long-term COVID-19 related school closures [50,51,52,53,54]. When considering the study results, it is possible that families with children in the home may have experienced greater food access through the schools during COVID-19, compared to before the pandemic. The school-based support provided during this time may have buffered the impact of long-term school closures on food insecurity among families in vulnerable situations, emphasizing the significance of social programs and policies to support these families.
Contrary to expectations and previous literature [22, 55], no interaction effect was found between family income or marital status and food insecurity on stress. Instead, individuals who indicated they were widowed or divorced reported less stress than those who were married. Regarding changes in stress levels, widowed respondents were less likely to experience a greater increase in stress after COVID-19, as compared to married respondents. The findings may suggest that individuals who are widowed are less likely to have children in the home and may be less stressed about the burden of feeding additional people. In addition, if these findings are gendered, women who are widowed may be less stressed due to the reduced burden of household labor that exists in a larger family [21]. Further, older adults, specifically retirees, are better able to isolate themselves, are more cautious of health risks, and have demonstrated resiliency related to potential mental health effects of COVID-19 [56, 57]. More research is needed in the future to determine whether these unexpected relationships between marital status and stress hold true beyond the pandemic period and beyond a rural sample.
The results indicated some buffering effects of the social and food environments on the relationship between food insecurity and stress. A stronger social environment after COVID-19 and higher levels of easiness in food access mitigated the negative impacts of food insecurity on stress. This supports the buffering hypothesis regarding the protective effect of psychosocial resources for those experiencing negative life events [18, 19]. However, this buffering effect is not always stronger for the high food insecure group in comparison to this effect for the moderate insecure group. This may be because the negative impacts of food insecurity are particularly strong for families who were moderately food insecure during COVID-19, to the extent that community connections would not provide much psychological relief to these families.
The study results points to an opportunity to continue to enhance rural residents’ access to healthy food, as well as to identify additional stressors in residents’ lives. There is a clear opportunity to link food distributions and associated food access programs with efforts intended to address related stressors—using a multifaceted approach to promote community well-being. Research has shown that prior to COVID-19, charitable sources of food were directed more toward counties with smaller populations [58]. Thus, rural communities may have been especially well prepared to start or expand food support programs during the COVID-19 pandemic, as evidenced by research showing that rural residents benefitted from expanded community food resources and expanded federal food assistance, especially through the Pandemic Supplemental Nutrition Assistance Program (PSNAP), during COVID-19 [59]. Such programs provide families with essential access to healthy food and can contribute to greater longer term positive outcomes, such as those associated with mental health and stress. Importantly, expanding access to food can strengthen sense of community and community belonging, as evidenced by research emphasizing the role of food banks in fostering a sense of community for residents of rural communities [46, 47, 60,61,62,63,64].
Although the study uncovered novel findings regarding food insecurity and stress, there are several limitations. The entire study population has been deemed “rural,” so no comparisons can be made between rural and suburban or urban environments. Additionally, the cross-sectional design precludes us from assessing the causal relationships between the variables of interest. The measure of food insecurity may not adequately capture the complexity of food insecurity over time, including the fact that families often have intermittent experiences with food insecurity and have different experiences depending on their receiving government support or support from informal channels [65, 66]. The findings may have limited generalizability as the sample was a convenience sample of residents in nine counties in one state and the data were collected during the COVID − 19 pandemic.
Conclusion
This study has revealed an interconnection between food insecurity and stress and the moderating impacts of food access and neighborhood social environment. Efforts to ameliorate food insecurity should address these broader contextual variables, involving community-level contextual factors. Further research should also continue exploring the relationship between food insecurity and mental health concerns, particularly beyond the COVID-19 pandemic. As stress is a critical indicator for overall mental and physical health, results from this study enhance understanding of the broader impacts of food insecurity on stress and other measures of well-being. The results add to the growing body of literature related to food insecurity and stress among rural populations, inform future research in these regions, and provide insights for developing and implementing effective policy and systemic interventions to promote community resources and increase the impact of healthy food assistance and related programs.
Availability of Study Data and Material
Due to privacy and ethical concerns, neither the data nor the source of the data can be made available.
Code Availability
Not applicable.
References
Coleman-Jensen, A., Rabbit, M. P., Hashad, R. N., Hales, L., & Gregory, C. A. (2022). Measurement. U.S. Department of Agriculture, Economic Research Service Retrieved from https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/measurement/.
Maynard, M., Andrade, L., Packull-McCormick, S., Perlman, C. M., Leos-Toro, C., & Kirkpatrick, S. I. (2018). Food insecurity and mental health among females in high-income countries. International Journal of Environmental Research and Public Health, 15(7), 1424. https://doi.org/10.3390/ijerph15071424.
Quintiliani, L. M., Whiteley, J. A., Zhu, J., Quinn, E. K., Murillo, J., Lara, R., & Kane, J. (2021). Examination of food insecurity, socio-demographic, psychosocial, and physical factors among residents in public housing. Ethnicity and Disease, 31(1), 159–164. https://doi.org/10.18865/ed.31.1.159.
Seligman, H. K., & Schillinger, D. (2010). Hunger and socioeconomic disparities in chronic disease. The New England Journal of Medicine, 363(1), 6–9. https://doi.org/10.1056/NEJMp1000072.
Haynes-Maslow, L., Andress, L., Byker-Shanks, C., Hardison-Moody, A., Pitts, S. J., Patton-Lopez, M., & Prewitt, T. E. (2020). Examining food insecurity in the rural United States: A qualitative study. Feeding America Retrieved from http://bestpractices.nokidhungry.org/sites/default/files/2020-02/Rural%20Food%20Insecurity%20Qualitative%20Research%20Brief.pdf
Feeding America (2021). The Impact of the Coronavirus on Food Insecurity in 2020 and 2021. FeedingAmerica.org Retrieved from https://www.feedingamerica.org/sites/default/files/2021-03/National%20Projections%20Brief_3.9.2021_0.pdf
Mueller, J. T., McConnell, K., Burow, P. B., Pofahl, K., Merdjanoff, A. A., & Farrell, J. (2021). Impacts of the COVID-19 pandemic on rural America. Pnas, 118(1), https://doi.org/10.1073/pnas.2019378118.
Schanzenbach, D. W., & Pitts, A. (2020). How much has food insecurity risen? Evidence from the Census Household Pulse Survey. Institute for Policy Research Rapid Research Report Retrieved from https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-10-june-2020.pdf.
Pearlin, L. I. (1989). The sociological study of stress. Journal of Health and Social Behavior, 30(3), 241–256. https://doi.org/10.2307/2136956.
Pearlin, L. I., Schieman, S., Fazio, E. M., & Meersman, S. C. (2005). Stress, health, and the life course: some conceptual perspectives. Journal of Health and Social Behavior, 46(2), 205–219. https://doi.org/10.1177/002214650504600206.
Compton, M. T., & Shim, R. S. (2015). The Social Determinants of Mental Health. Focus, 13(4), 419–425. https://doi.org/10.1176/appi.focus.20150017.
Laraia, B. (2013). Food Insecurity and Chronic Disease. American Society for Nutrition, 4, 203–212. https://doi.org/10.3945/an.112.003277.
Liu, Y., Rashid, S. N., Greenlund, K. J., Chapman, D. P., & Croft, J. B. (2014). Relationships between Housing and Food Insecurity, frequent Mental Distress, and Insufficient Sleep among adults in 12 US States, 2009. Preventing Chronic Disease, 11, E37. https://doi.org/10.5888/pcd11.130334.
Martin, M. S., Maddocks, E., Chen, Y., Gilman, S. E., & Colman, I. (2016). Food insecurity and mental illness: disproportionate impacts in the context of perceived stress and social isolation. Public Health, 132, 86–91. https://doi.org/10.1016/j.puhe.2015.11.014.
Wall-Bassett, E., Li, Y., & Matthews, F. (2017). The association of food insecurity and stress among college students in rural North Carolina. Journal of Nutrition Education and Behavior, 49(7), S75. https://doi.org/10.1016/j.jneb.2017.05.218.
Siefert, K., Heflin, C. M., Corcoran, M. E., & Williams, D. R. (2008). Food insufficiency and the physical and mental health of low-income women. Women & Health, 32(1), 159–177. https://doi.org/10.1300/J013v32n01_08.
Vozoris, N. T., & Tarasuk, V. S. (2003). Household food insufficiency is associated with poorer health. The Journal of Nutrition, 133(1), 120–126. https://doi.org/10.1093/jn/133.1.120.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. https://doi.org/10.1037/0033-2909.98.2.310.
Taylor, S. E., & Stanton, A. L. (2007). Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology, 3(1), 377–401. https://doi.org/10.1146/annurev.clinpsy.3.022806.091520.
Parekh, N., Ali, S. H., O’Connor, J., Tozan, Y., Jones, A. M., Capasso, A., Foreman, F., & DiClemente, R. J. (2021). Food insecurity among households with children during the COVID-19 pandemic: results from a study among social media users across the United States. Nutrition Journal, 20(73), https://doi.org/10.1186/s12937-021-00732-2.
Fan, L., & Moen (2019). Stress proliferation? Precarity and work-family conflict at the intersection of gender and household income. Journal of Family Issues, 40(18), https://doi.org/10.1177/0192513X19862847.
DeMaris, A. (2018). Marriage advantage in subjective well-being: causal effect or unmeasured heterogeneity? Marriage & family review, 54(4), 335–350. https://doi.org/10.1080/01494929.2017.1359812.
Waite, L. J., & Gallagher, M. (2001). The case for marriage: why married people are happier, healthier, and better off financially. New York, NY: Crown Publishing Group.
Belsky, D. W., Moffitt, T. E., Arseneault, L., Melichor, M., & Caspi, A. (2010). Context and sequelae of food insecurity in children’s development. American Journal of Epidemiology, 172, 809–818. https://doi.org/10.1093/aje/kwq201.
Leung, C. W., Laraia, B. A., Feiner, C., Solis, K., Stewart, A. L., Adler, N. E., & Epel, E. S. (2022). The psychological distress of Food Insecurity: a qualitative study of the emotional experiences of parents and their coping strategies. Journal of the Academy of Nutrition and Dietetics. https://doi.org/10.1016/j.jand.2022.05.010.
Lindow, P., Yen, I. H., Xiao, M., & Leung, C. W. (2022). ‘You run out of hope’: an exploration of low-income parents’ experiences with food insecurity using Photovoice. Public health nutrition, 25(4), 987–993. https://doi.org/10.1017%2FS1368980021002743.
Ling, J., Duren, P., & Robbins, L. B. (2022). Food Insecurity and Mental Well-Being among low-income families during COVID-19 pandemic. American Journal of Health Promotion. https://doi.org/10.1177/08901171221089627.
Nolen, E., Cubbin, C., & Brewer, M. (2022). The effect of maternal food insecurity transitions on housing insecurity in a population-based sample of mothers of young children. AIMS Public Health, 9(1), 1–16. https://doi.org/10.3934/publichealth.2022001.
Kepper, M. M., Myers, C. A., Denstel, K. D., Hunter, R. F., Guan, W., & Broyles, S. T. (2019). The neighborhood social environment and physical activity: a systematic scoping review. International Journal of Behavioral Nutrition and Physical Activity, 16(124), https://doi.org/10.1186/s12966-019-0873-7.
Teixeira, S., & Zuberi, A. (2018). Neighborhood social and environmental factors and asthma among children living in low-income neighborhoods: the importance of informal social control. Family & Community Health, 41(4), 214–224. https://doi.org/10.1097/FCH.000000000000202.
Robert Wood Johnson Foundation. (n.d.). Social determinants of health. Retrieved from https://www.rwjf.org/en/our-focus-areas/topics/social-determinants-of-health.html.
Denney, J. T., Kimbro, R. T., Heck, K., & Cubbin, C. (2017). Social cohesion and food insecurity: Insights from the Geographic Research on Wellbeing (GROW) study. Journal of Maternal and Child Health, 21(2), 343–350. https://doi.org/10.1007/s10995-016-2119-5.
Martin, K. S., Rogers, B. L., Cook, J. T., & Joseph, H. M. (2004). Social capital is associated with decreased risk of hunger. Social & Science Medicine, 58(12), 2645–2654. https://doi.org/10.1016/j.socscimed.2003.09.026.
Suglia, S. F., Shelton, R. C., Hsaio, A., Wang, Y. C., Rundle, A., & Link, B. G. (2016). Why the neighborhood social environment is critical in obesity prevention. Journal of Urban Health, 93(2016), 206–212. https://doi.org/10.1007/s11524-015-0017-6.
Nelson, E., Bangham, C., Modi, S., Liu, X., Codner, A., Hicks, J. M., & Greece, J. (2022). Understanding the impacts of COVID-19 on the determinants of food insecurity: a state-specific examination. Preventive Medicine Reports, 28. https://doi.org/10.1016%2Fj.pmedr.2022.101871.
Whiting, E. F., & Ward, C. (2010). Food provisioning strategies, food insecurity, and stress in an economically vulnerable community: the Northern Cheyenne case. Agriculture and human values, 27(4), 489–504. https://doi.org/10.1007/s10460-009-9248-z.
Wilkinson, R., & Marmot, M. (Eds.). (2003). The social determinants of health: the solid facts (2nd ed.).). World Health Organization.
McAuliffe, C., Daly, Z., Black, J., Pumarino, J., Gadermann, A., Slemon, A., … Jenkins,E. K. (2021). Examining the associations between food worry and mental health during the early months of the COVID-19 pandemic in Canada. Canadian Journal of Public Health, 112(5), 843–852. https://doi.org/10.17269%2Fs41997-021-00557-w.
Wolfson, J. A., Garcia, T., & Leung, C. W. (2021). Food insecurity is associated with depression, anxiety, and stress: evidence from the early days of the COVID-19 pandemic in the United States. Health equity, 5(1), 64–71. https://doi.org/10.1089/heq.2020.0059.
Ahn, S., & Norwood, F. B. (2021). Measuring food insecurity during the COVID-19 pandemic of spring 2020. Applied Economic Perspectives and Policy, 43(1), 162–168. https://doi.org/10.1002/aepp.13069.
Morales, D. A., Barksdale, C. L., & Beckel-Mitchener, A. C. (2020). A call to action to address rural mental health disparities. Journal of Clinical and Translational Science, 4(5), 463–467. https://doi.org/10.1017/cts.2020.42.
Encinger, A., Kutaka, T. S., Chernyavskiy, P., Ibrahim, H., & Raikes, H. H. (2020). Relations among low-income preschool children’s self-regulation, marginal food security, and parental stress. Early Education and Development, 31(8), 1264–1280. https://doi.org/10.1080/10409289.2020.1749492.
U.S. Department of Agriculture (2012). U.S. household food security survey module: Six-item short form. Washington, DC. Retrieved from https://www.ers.usda.gov/media/8282/short2012.pdf.
StataCorp. (2015). Stata Statistical Software: release 14. College Station. TX: StataCorp LP.
Arenas, D. J., Thomas, A., Wang, J., & DeLisser, H. M. (2019). A systematic review and meta-analysis of depression, anxiety, and sleep disorders in US adults with food insecurity. Journal of General Internal Medicine, 34(12), 2874–2882. https://doi.org/10.1007/s11606-019-05202-4.
Jones, A. D. (2017). Food insecurity and mental health status: a global analysis of 149 countries. American Journal of Preventative Medicine, 53(2), 264–273. https://doi.org/10.1016/j.amepre.2017.04.008.
Lent, M. D., Petrovic, L. E., Swanson, J. A., & Olson, C. M. (2009). Maternal mental health and the persistence of food insecurity in poor rural families. Journal of Health Care for the Poor and Underserved, 20(3), 645–661. https://doi.org/10.1353/hpu.0.0182.
Black, M. M. (2012). Protect children from household food insecurity: promote access to food and stress-alleviating resources. Journal of Applied Research on Children: Informing Policy for Children at Risk, 3(1), 18.
Braun, A., Hawley, J. D., & Garner, J. A. (2022). Maintaining school foodservice operations in Ohio during COVID-19: “This [was] not the time to sit back and watch. International Journal of Environmental Research and Public Health, 19(10), https://doi.org/10.3390/ijerph19105991.
Kinsey, E. W., Hecht, A. A., Dunn, C. G., Levi, R., Read, M. A., Smith, C., Niesen, P., Seligman, H. K., & Hager, E. R. (2020). School closures during COVID-19: Opportunities for innovation in meal service. American Journal of Public Health, 110(10), 1635–1643. https://doi.org/10.2105/AJPH.2020.305875.
Poole, M. K., Fleishhacker, S. E., & Bleich, S. N. (2021). Addressing child hunger when school is closed–considerations during the pandemic and beyond. The New England Journal of Medicine, 384(e35), https://doi.org/10.1056/NEJMp2033629.
Lancker, W. V., & Parolin, Z. (2020). COVID-19, school closures, and child poverty: a social crisis in the making. The Lancet Public Health, 5(5), E243–E244. https://doi.org/10.1016/S2468-2667(20)30084-0.
Dongo, L., & Monte, L. (2022). National school lunch program still important part of safety net. United States Census Bureau Retrieved from https://www.census.gov/library/stories/2022/04/less-hunger-in-at-risk-households-during-pandemic-expansion-of-school-meals-program.html.
Lee, J. W., Shin, W. K., & Kim, Y. (2020). Impact of sex and marital status on the prevalence of perceived depression in association with food insecurity. PloS one, 15(6), https://doi.org/10.1371/journal.pone.0234105.
Bertoni, M., Celidoni, M., Bianco, C. D., & Weber, G. (2021). How did european retirees respond to the COVID-19 pandemic? Economics Letters, 203. https://doi.org/10.1016/j.econlet.2021.109853.
Richter, L., & Heidinger, T. (2021). Hitting close to home: the effect of COVID-19 illness in the social environment on psychological burden in older adults. Frontiers in Psychology, 12. https://doi.org/10.3389/fpsyg.2021.737787.
Gundersen, C., Dewey, A., Hake, M., Engelhard, E., & Crumbaugh, A. S. (2017). Food insecurity across the rural-urban divide: are counties in need being reached by charitable food assistance? The ANNALS of the American Academy of Political and Social Science, 672(1), 217–237. https://doi.org/10.1177/0002716217710172.
Cardarelli, K. M., DeWitt, E., Gillespie, R., Graham, R. H., Norman-Burgdolf, H., & Mullins, J. T. (2021). Policy implications of the COVID-19 pandemic on Food Insecurity in Rural America: evidence from Appalachia. International Journal of Environmental Research and Public Health, 18(23), https://doi.org/10.3390/ijerph182312792.
Bronte-Tinkew, J., Zaslow, M., Capps, R., Horowitz, A., & McNamara, M. (2007). Food insecurity works through depression, parenting, and infant feeding to influence overweight and health in toddlers. The Journal of nutrition, 137(9), 2160–2165. https://doi.org/10.1093/jn/137.9.2160.
Buck-McFadyen, E. (2013). The experience of food insecurity for rural families: Nursing practice and policy implications [Master’s Thesis, York University] YorkSpace, York University. http://hdl.handle.net/10315/31693.
Heflin, C. M., & Ziliak, J. P. (2008). Food insufficiency, food stamp participation, and mental health. Social Science Quarterly, 89(3), 706–727. https://doi.org/10.1111/j.1540-6237.2008.00556.x.
Hwang, J. Y., Kim, B., & Kim, K. (2014). A qualitative study on attitude, acceptability, and adaptation for home-delivered meal services in the korean elderly from the perspective of life context. Korean Journal of Community Nutrition, 19(5), https://doi.org/10.5720/kjcn.2014.19.5.459.
Whitaker, R. C., Phillips, S. M., & Orzol, S. M. (2006). Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics, 118(3), e859–e868. https://doi.org/10.1542/peds.2006-0239.
Bowen, S., Elliott, S., & Hardison-Moody, A. (2021). The structural roots of food insecurity: how racism is a fundamental cause of food insecurity. Sociology Compass, 15(7), e12846. https://doi.org/10.1111/soc4.12846.
Calloway, E. E., Fricke, H. E., Pinard, C. A., Smith, T. M., & Yaroch, A. L. (2015). Monthly SNAP Benefit Duration and its Association with Food Security, Hunger-Coping, and physiological hunger symptoms among low-income families. Journal of Applied Research on Children, 6(2), 5.
Acknowledgements
The research team would like to thank the community agencies and community members who participated in this study.
Funding
This work was supported by grants from [blinded for peer review] and [blinded for peer review].
Author information
Authors and Affiliations
Contributions
Study conceptualization: CK, YL, CM, SB, SG, LH; Investigation: CK, CH, SB, SG, CM, LH; Statistical analysis: YL; Initial draft preparation: CK, CM, YL; Review and editing: CK, YL, CM, SB, SG, LH, CH. All authors read and approved submission of the final article.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Ethics Approval
Humans subjects approval was obtained by the [blinded for peer review] University Institutional Review Board.
Consent to Participate
Consent to participate was obtained from study participants prior to their completing the survey. Participants were informed that their participation was completely voluntary and that they could choose to stop taking part in the interview/survey at any time.
Consent for Publication
Consent for publication was obtained from study participants at the time their consent to participate was obtained. Participants were informed that the results of this study may be shared through community forums, technical reports, journal articles, and educational presentations.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koob, C., Luo, Y., Mobley, C. et al. Food Insecurity and Stress Among Rural Residents in South Carolina: The Moderating Influences of Household Characteristics, Neighborhood Social Environment and Food Environment. J Community Health 48, 367–380 (2023). https://doi.org/10.1007/s10900-022-01176-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-022-01176-3