Abstract
Purpose
We explored and compared perspectives of reproductive endocrinology and infertility specialists (REIs) and in vitro fertilization (IVF) patients regarding polygenic embryo screening (PES), a new type of preimplantation screening that estimates the genetic chances of developing polygenic conditions and traits in the future.
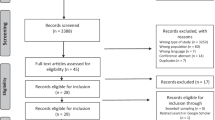
Methods
Qualitative thematic analysis of semi-structured interviews with US-based REIs and IVF patients.
Results
Clinicians and patients often held favorable views of screening embryos for physical or psychiatric conditions, though clinicians tended to temper their positive attitudes with specific caveats. Clinicians also expressed negative views about screening embryos for traits more frequently than patients, who generally held more positive views. Most clinicians were either unwilling to discuss or offer PES to patients or were willing to do so only under certain circumstances, while many patients expressed interest in PES. Both stakeholder groups envisioned multiple potential benefits or uses of PES and raised multiple potential, interrelated concerns about PES.
Conclusion
A gap exists between clinician and patient attitudes toward PES; clinicians generally maintained reservations about such screening and patients indicated interest in it. Clinicians and patients sometimes imagined using PES to prepare for the birth of a predisposed or “affected” individual—a rationale that is often associated with prenatal testing. Many clinicians and patients held different attitudes depending on what is specifically screened, despite the sometimes blurry distinction between conditions and traits. Considerations raised by clinicians and patients may help guide professional societies in developing guidelines to navigate the uncertain terrain of PES.

Similar content being viewed by others
Data availability
De-identified coded transcript excerpts will be made available upon reasonable request to the corresponding author.
Notes
While we recognize that the socio-ethical implications of this technology are similar to those of other types of preimplantation genetic tests, our use of the acronym PES (vs. PGT-P) highlights its clinical and technical differences from other types of preimplantation genetic tests.
References
Lázaro-Muñoz G, Pereira S, Carmi S, Lencz T. Screening embryos for polygenic conditions and traits: ethical considerations for an emerging technology. Genet Med. 2021;23:432–4. https://doi.org/10.1038/s41436-020-01019-3.
Wand H, Lambert SA, Tamburro C, et al. Improving reporting standards for polygenic scores in risk prediction studies. Nature. 2021;591, 211–219. https://doi.org/10.1038/s41586-021-03243-6.
Duncan L, Shen H, Gelaye B, et al. Analysis of polygenic risk score usage and performance in diverse human populations. Nat Commun. 2019;10:3328. https://doi.org/10.1038/s41467-019-11112-0.
Karavani E, Zuk O, Zeevi D, et al. Screening human embryos for polygenic traits has limited utility. Cell. 2019;179:1424-1435.e8. https://doi.org/10.1016/j.cell.2019.10.033.
Lencz T, Backenroth D, Granot-Hershkovitz E, et al (2021) Utility of polygenic embryo screening for disease depends on the selection strategy. Elife 10. https://doi.org/10.7554/eLife.64716.
Treff NR, Eccles J, Marin D, et al (2020) Preimplantation genetic testing for polygenic disease relative risk reduction: evaluation of genomic index performance in 11,883 adult sibling pairs. Genes (Basel) 11. https://doi.org/10.3390/genes11060648.
Turley P, Meyer MN, Wang N, et al. Problems with using polygenic scores to select embryos. N Engl J Med. 2021;385:78–86. https://doi.org/10.1056/NEJMsr2105065.
Bayefsky M. Who should regulate preimplantation genetic diagnosis in the United States? AMA J Ethics. 2018;20:1160–7.
Abu-El-Haija A, Reddi HV, Wand H, et al (2023) The clinical application of polygenic risk scores: a points to consider statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med 25. https://doi.org/10.1016/j.gim.2023.100803.
Wand H, Kalia SS, Helm BM, et al. Clinical genetic counseling and translation considerations for polygenic scores in personalized risk assessments: a practice resource from the National Society of Genetic Counselors. J Genet Couns. 2023;32:558–75. https://doi.org/10.1002/jgc4.1668.
Forzano F, Antonova O, Clarke A, et al. The use of polygenic risk scores in pre-implantation genetic testing: an unproven, unethical practice. Eur J Hum Genet. 2022;30:493–5. https://doi.org/10.1038/s41431-021-01000-x.
European Society of Human Reproduction and Embryology (2022) ESHRE supports the position of ESHG on embryo selection based on polygenic risk scores. https://www.eshre.eu/Europe/Position-statements/PRS. Accessed 23 Aug 2023.
Regalado A. The world’s first Gattaca baby tests are finally here. MIT Technol Rev. 2019. https://www.technologyreview.com/2019/11/08/132018/polygenic-score-ivf-embryo-dna-tests-genomic-prediction-gattaca/. Accessed 23 Aug 2023.
Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52:1893–907. https://doi.org/10.1007/s11135-017-0574-8.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. https://doi.org/10.1191/1478088706qp063oa.
Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632. https://doi.org/10.1016/j.ijnurstu.2020.103632.
O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. https://doi.org/10.1097/ACM.0000000000000388.
Siermann M, Valcke O, Vermeesch JR, et al. Limitations, concerns and potential: attitudes of healthcare professionals toward preimplantation genetic testing using polygenic risk scores. Eur J Hum Genet. 2023. https://doi.org/10.1038/s41431-023-01333-9.
Terek ST, Gamma A, Zak M, Butts H. Preimplantation testing of embryos for polygenic related conditions: the ethical concerns surrounding it and the position of genetic counselors. Fertility and Sterility. 2021;116(3):e56. https://doi.org/10.1016/j.fertnstert.2021.07.159.
Roche K, Racowsky C, Harper J. Utilization of preimplantation genetic testing in the USA. J Assist Reprod Genet. 2021;38:1045–53. https://doi.org/10.1007/s10815-021-02078-4/Published.
Neuhausser WM, Fouks Y, Lee SW, et al (2023) Acceptance of genetic editing and of whole genome sequencing of human embryos by patients with infertility before and after the onset of the COVID-19 pandemic. Reprod Biomed Online. 47. https://doi.org/10.1016/j.rbmo.2023.03.013.
Eccles J, Marin D, Duffy L, et al (2021) Rate of patients electing for polygenic risk scores in preimplantation genetic testing. In: Fertility and sterility. Elsevier BV, pp e267–e268.
Gleicher N, Patrizio P, Brivanlou A. Preimplantation genetic testing for aneuploidy – a castle built on sand. Trends Mol Med. 2021;27:731–42. https://doi.org/10.1016/j.molmed.2020.11.009.
Mastenbroek S, De Wert G, Adashi EY. The imperative of responsible innovation in reproductive medicine. N Engl J Med. 2021;22:385.
Beauchamp TL, Childress JF. Principles of biomedical ethics. 7th ed. New York: Oxford University Press; 2013.
Ethics Committee of the American Society for Reproductive Medicine. Transferring embryos with genetic anomalies detected in preimplantation testing: an ethics committee opinion. Fertil Steril. 2017;107:1130–5. https://doi.org/10.1016/j.fertnstert.2017.02.121.
Hughes T, Bracewell-Milnes T, Saso S, et al. A review on the motivations, decision-making factors, attitudes and experiences of couples using pre-implantation genetic testing for inherited conditions. Hum Reprod Update. 2021;27:944–66. https://doi.org/10.1093/humupd/dmab013.
Michie M. Is preparation a good reason for prenatal genetic testing? Ethical and critical questions. Birth Defects Res. 2020;112:332–8.
Ethics Committee of the American Society for Reproductive Medicine. Disclosure of sex when incidentally revealed as part of preimplantation genetic testing (PGT): an ethics committee opinion. Fertil Steril. 2018;110:625–7. https://doi.org/10.1016/j.fertnstert.2018.06.019.
Ethics Committee of the American Society for Reproductive Medicine. Use of reproductive technology for sex selection for nonmedical reasons: an ethics committee opinion. Fertil Steril. 2022;117:720–6. https://doi.org/10.1016/j.fertnstert.2021.12.024.
Bowman-Smart H, Savulescu J, Mand C, et al. “Is it better not to know certain things?”: views of women who have undergone non-invasive prenatal testing on its possible future applications. J Med Ethics. 2019;45:231–8. https://doi.org/10.1136/medethics-2018-105167.
Sullivan HK, Bayefsky M, Wakim PG, et al. Noninvasive prenatal whole genome sequencing: pregnant women’s views and preferences. Obstet Gynecol. 2019;133:525–32. https://doi.org/10.1097/AOG.0000000000003121.
Zhang J, Pastore LM, Sarwana M, et al. Ethical and moral perspectives of individuals who considered/used preimplantation (embryo) genetic testing. J Genet Couns. 2022;31:176–87. https://doi.org/10.1002/jgc4.1471.
Wertz DC, Knoppers BM. Serious genetic disorders: can or should they be defined? Am J Med Genet. 2002;108:29–35.
Wasserman D, Asch A, Blustein J, Putnam D. "Disability: health, well-being, and personal relationships". In: Zalta EN, editor. The stanford encyclopedia of philosophy (summer 2022 edition). 2016. https://plato.stanford.edu/archives/sum2022/entries/disability-health/.
Murphy D. "Concepts of disease and health". In: Zalta EN, Nodelman U, editors. The stanford encyclopedia of philosophy (fall 2023 edition). 2020. https://plato.stanford.edu/archives/fall2023/entries/health-disease/.
Huber M, Knottnerus JA, Green L, et al. Health: how should we define it? Br Med J. 2011;343:235–7.
Chen SC, Wasserman DT. A framework for unrestricted prenatal whole-genome sequencing: respecting and enhancing the autonomy of prospective parents. Am J Bioeth. 2017;17:3–18. https://doi.org/10.1080/15265161.2016.1251632.
Kleiderman E, Rahimzadeh V, Knoppers B, et al. The serious factor in expanded prenatal genetic testing. Am J Bioeth. 2022;22:23–5. https://doi.org/10.1080/15265161.2021.2013991.
Acknowledgements
The authors thank the REIs and IVF patients that participated in this study, as well as Jason Bach, Arturo Balaguer, Jonathan Frumovitz, and Page Trotter for their assistance with data analysis and Ana Battaglino for her feedback on the manuscript.
Funding
This work was supported by National Human Genome Research Institute, R01HG011711, Todd Lencz.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SC is a paid consultant at MyHeritage. All other co-authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barlevy, D., Cenolli, I., Campbell, T. et al. Patient interest in and clinician reservations on polygenic embryo screening: a qualitative study of stakeholder perspectives. J Assist Reprod Genet 41, 1221–1231 (2024). https://doi.org/10.1007/s10815-024-03074-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-024-03074-0