Abstract
Purpose
Beta-blocker is a frequently used medication in cardiovascular diseases. However, long-term benefit of beta-blocker in patients with preserved left ventricular ejection function (LVEF) on major adverse cardiovascular events (MACEs) is uncertain.
Methods
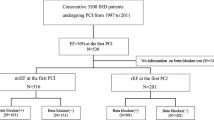
The Cohort Of patients with high Risk for cardiovascular Events (CORE-Thailand) was a prospective study that enrolled Thai patients with high atherosclerotic risk including multiple atherosclerotic risk factors and established atherosclerotic cardiovascular diseases. Baseline demographic data, co-morbidities and medication were recorded. Patients were followed for 5 years. Patients with LVEF<50% were excluded. Primary outcome was the effect of beta-blocker on the occurrence of MACEs including all-cause death, non-fatal myocardial infarction and non-fatal stroke (3P-MACEs). Propensity score matching was used to control confounding factors.
Results
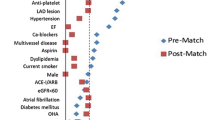
There was a total of 8513 patients in the pre-matched cohort, 4418 were taking beta-blocker and 4095 were not. After adjustment of confounders, beta-blocker was an independent predictor of 3P-MACEs (adjusted HR 1.29;95% CI 1.12-1.49;p<0.001). After propensity score matching, 4686 patients remained in the post-matched cohort. Propensity score analysis showed consistent results in which patient taking beta-blocker had higher risk of 3P-MACEs (adjusted HR 1.29;95% CI 1.10-1.53;p=0.002). Subgroup analysis in patients with coronary artery disease (CAD) indicated that taking beta-blocker did not increase the incidence of 3P-MACEs (adjusted HR 0.99;95% CI 0.76-1.29) while those without CAD did (adjusted HR 1.51; 95% CI, 1.22-1.86;p-interaction=0.015).
Conclusion
In patients with high atherosclerotic cardiovascular risk, taking beta-blockers had a higher risk of 3P-MACEs. Care should be taken when prescribing beta-blockers to patients without a clear indication.
Trial registration
TCTR20130520001 registered in Thai Clinical Trials Registry (TCTR) https://www.thaiclinicaltrials.org/, date of registration 20 May 2013.



Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Heidenreich PA, Bozkurt B, Aguilar D, et al. AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032.
McDonagh TA, Metra M, Adamo M, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
O'Gara PT, Kushner FG, Ascheim DD, et al. ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362–425.
Amsterdam EA, Wenger NK, Brindis RG, et al. AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130(25):e344–426.
Freemantle N, Cleland J, Young P, Mason J, Harrison J. beta Blockade after myocardial infarction: systematic review and meta regression analysis. Bmj. 1999;318(7200):1730–7.
Bangalore S, Steg G, Deedwania P, et al. beta-Blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. JAMA. 2012;308(13):1340–9.
Puymirat E, Riant E, Aissaoui N, et al. beta blockers and mortality after myocardial infarction in patients without heart failure: multicentre prospective cohort study. BMJ. 2016;354:i4801.
Fukase T, Dohi T, Koike T, et al. Long-term impact of beta-blocker in elderly patients without myocardial infarction after percutaneous coronary intervention. ESC Heart Fail. 2022;9(1):545–54.
Motivala AA, Parikh V, Roe M, et al. Predictors, Trends, and Outcomes (Among Older Patients >/=65 Years of Age) Associated With Beta-Blocker Use in Patients With Stable Angina Undergoing Elective Percutaneous Coronary Intervention: Insights From the NCDR Registry. JACC Cardiovasc Interv. 2016;9(16):1639–48.
Tsujimoto T, Kajio H, Shapiro MF, Sugiyama T. Risk of All-Cause Mortality in Diabetic Patients Taking beta-Blockers. Mayo Clin Proc. 2018;93(4):409–18.
Tsujimoto T, Sugiyama T, Kajio H. Effects of beta-blockers on all-cause mortality in patients with type 2 diabetes and coronary heart disease. Diabetes Obes Metab. 2017;19(6):800–8.
Kjeldsen SE, Lyle PA, Kizer JR, et al. The effects of losartan compared to atenolol on stroke in patients with isolated systolic hypertension and left ventricular hypertrophy. The LIFE study. J Clin Hypertens (Greenwich). 2005;7(3):152–8.
Park J, Han JK, Kang J, et al. The Clinical Impact of β-Blocker Therapy on Patients With Chronic Coronary Artery Disease After Percutaneous Coronary Intervention. Korean Circ J. 2022;52(7):544–55.
Silverman DN, de Lavallaz JDF, Plante TB, et al. Beta-Blocker Use in Hypertension and Heart Failure (A Secondary Analysis of the Systolic Blood Pressure Intervention Trial). Am J Cardiol. 2022;165:58–64.
Williams B, Lacy PS, Thom SM, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–25.
Messerli FH, Rimoldi SF, Bangalore S, Bavishi C, Laurent S. When an Increase in Central Systolic Pressure Overrides the Benefits of Heart Rate Lowering. J Am Coll Cardiol. 2016;68(7):754–62.
Whelton PK, Carey RM, Aronow WS, et al. 2017ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–324.
Ishak D, Aktaa S, Lindhagen L, et al. Association of beta-blockers beyond 1 year after myocardial infarction and cardiovascular outcomes. Heart. 2023;109(15):1159–65.
Arnold SV, Silverman DN, Gosch K, et al. Beta-Blocker Use and Heart Failure Outcomes in Mildly Reduced and Preserved Ejection Fraction. JACC Heart Fail. 2023.
Bangalore S, Parkar S, Grossman E, Messerli FH. A meta-analysis of 94,492 patients with hypertension treated with beta blockers to determine the risk of new-onset diabetes mellitus. Am J Cardiol. 2007;100(8):1254–62.
Sharma AM, Pischon T, Hardt S, Kunz I, Luft FC. Hypothesis: Beta-adrenergic receptor blockers and weight gain: A systematic analysis. Hypertension. 2001;37(2):250–4.
Elliott WJ, Meyer PM. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet. 2007;369(9557):201–7.
Weir MR, Moser M. Diuretics and beta-blockers: is there a risk for dyslipidemia? Am Heart J. 2000;139(1 Pt 1):174–83.
Psaty BM, Koepsell TD, Wagner EH, LoGerfo JP, Inui TS. The relative risk of incident coronary heart disease associated with recently stopping the use of beta-blockers. JAMA. 1990;263(12):1653–7.
Acknowledgments
We would like to express our appreciation for all the efforts and contributions to the study support from the investigators of CORE registry, Thailand. This study was supported by The Heart Association of Thailand, National Research Council of Thailand (NRCT) and Health Systems Research Institute (HSRI).
Funding
This study was supported by The Heart Association of Thailand, National Research Council of Thailand (NRCT) and Health Systems Research Institute (HSRI). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
NO performed statistical analysis, wrote the manuscript, tables, and figures. KU, KS, BS revising it critically for important intellectual content. SG collected and re-checked the data prior to the analysis. WS performed statistical analysis and figures. WW, AP substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of the data for the work. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding authors
Ethics declarations
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Joint Research Ethics Committee and Ministry of Public Health, Thailand (Approval Number COA-JREC 004/2011, date of approval 21 May 2011).
Consent to Participate
Informed consent was obtained from all patients prior to the commencement of the study.
Consent for Publication
Not applicable.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Osataphan, N., Udol, K., Siriwattana, K. et al. Effect of Beta-Blocker on Long-Term Major Cardiovascular Events in High Atherosclerotic Risk Population. Cardiovasc Drugs Ther (2023). https://doi.org/10.1007/s10557-023-07502-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-023-07502-8