Abstract
Purpose
This study is aimed at investigating gender differences in the medical management of patients with coronary heart disease (CHD).
Methods
Analyses were based on the ESC EORP EUROASPIRE V (European Survey Of Cardiovascular Disease Prevention And Diabetes) survey. Consecutive patients between 18 and 80 years, hospitalized for a coronary event, were included in the study. Information on cardiovascular medication intake at hospital discharge and at follow-up (≥ 6 months to < 2 years after hospitalization) was collected.
Results
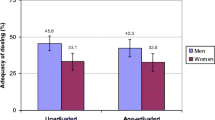
Data was available for 8261 patients (25.8% women). Overall, no gender differences were observed in the prescription and use of cardioprotective medication like aspirin, beta-blockers, and ACE-I/ARBs (P > 0.01) at discharge and follow-up respectively. However, a statistically significant difference was found in the use of statins at follow-up, in disfavor of women (82.8% vs. 77.7%; P < 0.001). In contrast, at follow-up, women were more likely to use diuretics (31.5% vs. 39.5%; P < 0.001) and calcium channel blockers (21.2% vs. 28.8%; P < 0.001), whereas men were more likely to use anticoagulants (8.8% vs. 7.0%; P < 0.001). Overall, no gender differences were found in total daily dose intake (P > 0.01). Furthermore, women were less likely than men to have received a CABG (20.4% vs. 13.2%; P < 0.001) or PCI (82.1% vs. 74.9%; P < 0.001) at follow-up. No gender differences were observed in prescribed (P = 0.10) and attended (P = 0.63) cardiac rehabilitation programs.
Conclusion
The EUROASPIRE V results show only limited gender differences in the medical management of CHD patients. Current findings suggest growing awareness about risk in female CHD patients.

Similar content being viewed by others
Data Availability
No availability of data and material.
References
Piepoli MF, Abreu A, Albus C, Ambrosetti M, Brotons C, Catapano AL, et al. Update on cardiovascular prevention in clinical practice: a position paper of the European Association of Preventive Cardiology of the European Society of Cardiology. Eur J Prev Cardiol. 2020;27(2):181–205.
Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18(12):598–603.
Maas AH, Van Der Schouw YT, Regitz-Zagrosek V, et al. Red alert for women's heart: the urgent need for more research and knowledge on cardiovascular disease in women: proceedings of the workshop held in Brussels on gender differences in cardiovascular disease, 29 September 2010. Eur Heart J. 2011;32(11):1362–8.
Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, et al. European Society of Cardiology: cardiovascular disease statistics 2019. Eur Heart J. 2020;41(1):12–85.
Dallongevillle J, De Bacquer D, Heidrich J, et al. Gender differences in the implementation of cardiovascular prevention measures after an acute coronary event. Heart. 2010;96(21):1744–9.
Haider A, Bengs S, Luu J, et al. Sex and gender in cardiovascular medicine: presentation and outcomes of acute coronary syndrome. Eur Heart J. 2019.
Maffei S, Guiducci L, Cugusi L, Cadeddu C, Deidda M, Gallina S, et al. Women-specific predictors of cardiovascular disease risknew paradigms. Int J Cardiol. 2019;286:190–7.
Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non–ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the American College of Cardiology/American Heart Association guidelines) national quality improvement initiative. J Am Coll Cardiol. 2005;45(6):832–7.
Koopman C, Vaartjes I, Heintjes EM, Spiering W, van Dis I, Herings RMC, et al. Persisting gender differences and attenuating age differences in cardiovascular drug use for prevention and treatment of coronary heart disease, 1998–2010. Eur Heart J. 2013;34(41):3198–205.
Wilkinson C, Bebb O, Dondo TB, Munyombwe T, Casadei B, Clarke S, et al. Sex differences in quality indicator attainment for myocardial infarction: a nationwide cohort study. Heart. 2019;105(7):516–23.
Lichtman JH, Leifheit EC, Safdar B, Bao H, Krumholz HM, Lorenze NP, et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO study (variation in recovery: role of gender on outcomes of young AMI patients). Circulation. 2018;137(8):781–90.
Patel H, Rosengren A, Ekman I. Symptoms in acute coronary syndromes: does sex make a difference? Am Heart J. 2004;148(1):27–33.
Hiteshi AK, Li D, Gao Y, Chen A, Flores F, Mao SS, et al. Gender differences in coronary artery diameter are not related to body habitus or left ventricular mass. Clin Cardiol. 2014;37(10):605–9.
Kotseva K, De Backer G, De Bacquer D, et al. Lifestyle and impact on cardiovascular risk factor control in coronary patients across 27 countries: results from the European Society of Cardiology ESCEORP EUROASPIRE V registry. Eur J Prev Cardiol. 2019;26(8):824–35.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and Other Societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81.
Arnold SV, Spertus JA, Masoudi FA, Daugherty SL, Maddox TM, Li Y, et al. Beyond medication prescription as performance measures: optimal secondary prevention medication dosing after acute myocardial infarction. J Am Coll Cardiol. 2013;62(19):1791–801.
Asenjo RM, Bueno H, Mcintosh M. Angiotensin converting enzyme inhibitors (ACE inhibitors) and angiotensin II receptor blockers (ARBs) - ACE inhibitors and ARBs, a cornerstone in the prevention and treatment of cardiovascular disease. 2017. https://www.escardio.org/Education/ESC-Prevention-of-CVD-Programme/Treatment-goals/Cardio-Protective-drugs/angiotensin-converting-enzyme-inhibitors-ace-inhibitors-and-angiotensin-ii-rec. Accessed 15 June 2020.
Frederix I, Mcintosh M. Beta-blockers - modes of action & cardiovascular effects, indications, contraindications & side effects. 2017. https://www.escardio.org/Education/ESC-Prevention-of-CVD-Programme/Treatment-goals/Cardio-Protective-drugs/beta-blockers. Accessed 15 June 2020.
Krychtiuk KA, Speidl WS. Statins & more - overview of common lipid-lowering drugs used in secondary prevention to reach LDL treatment goals. 2017. https://www.escardio.org/Education/ESC-Prevention-of-CVD-Programme/Treatment-goals/Cardio-Protective-drugs/statins-more. Accessed 15 June 2020.
Vranckx P, Huber K. Antiplatelets therapy - antiplatelet therapy in ischemic heart disease. 2017. https://www.escardio.org/Education/ESC-Prevention-of-CVD-Programme/Treatment-goals/Cardio-Protective-drugs/antiplatelets-therapy. Accessed 15 June 2020.
Hilleary RS, Jabusch SM, Zheng B, et al. Gender disparities in patient education provided during patient visits with a diagnosis of coronary heart disease. Women’s Health. 2019;15:1745506519845591.
Hambraeus K, Tydén P, Lindahl B. Time trends and gender differences in prevention guideline adherence and outcome after myocardial infarction: data from the SWEDEHEART registry. Eur J Prev Cardiol. 2016;23(4):340–8.
De Smedt D, De Bacquer D, De Sutter J, et al. The gender gap in risk factor control: effects of age and education on the control of cardiovascular risk factors in male and female coronary patients. The EUROASPIRE IV study by the European Society of Cardiology. Int J Cardiol. 2016;209:284–90.
Lahoz C, Mantilla T, Taboada M, Soler B, Tranche S, López-Rodriguez I, et al. Gender differences in evidence-based pharmacological therapy for patients with stable coronary heart disease. Int J Cardiol. 2009;133(3):336–40.
Goldstein KM, Zullig LL, Bastian LA, Bosworth HB. Statin adherence: does gender matter? Curr Atheroscler Rep. 2016;18(11):63.
De Smedt D, De Backer T, Petrovic M, et al. Chronic medication intake in patients with stable coronary heart disease across Europe: evidence from the daily clinical practice. Results from the ESC EORP European Survey of Cardiovascular Disease Prevention and Diabetes (EUROASPIRE IV) Registry. Int J Cardiol. 2020;300:7–13.
Zhao M, Vaartjes I, Graham I, Grobbee D, Spiering W, Klipstein-Grobusch K, et al. Sex differences in risk factor management of coronary heart disease across three regions. Heart. 2017;103(20):1587–94.
Brugts J, Arima H, Remme W, et al. The incidence and clinical predictors of ACE-inhibitor induced dry cough by perindopril in 27,492 patients with vascular disease. Int J Cardiol. 2014;176(3):718–23.
Anand SS, Islam S, Rosengren A, Franzosi MG, Steyn K, Yusufali AH, et al. Risk factors for myocardial infarction in women and men: insights from the INTERHEART study. Eur Heart J. 2008;29(7):932–40.
De Smedt D, Clays E, Annemans L, Pardaens S, Kotseva K, De Bacquer D. Self-reported health status in coronary heart disease patients: a comparison with the general population. Eur J Cardiovasc Nurs. 2015;14(2):117–25.
Pogosova N, Kotseva K, De Bacquer D, et al. Psychosocial risk factors in relation to other cardiovascular risk factors in coronary heart disease: results from the EUROASPIRE IV survey. A registry from the European Society of Cardiology. Eur J Prev Cardiol. 2017;24(13):1371–80.
Lewer D, O'Reilly C, Mojtabai R, Evans-Lacko S. Antidepressant use in 27 European countries: associations with sociodemographic, cultural and economic factors. Br J Psychiatry. 2015;207(3):221–6.
Doyle F, Harpe DDL, McGee H, Shelley E, Conroy R. Gender differences in the presentation and management of acute coronary syndromes: a national sample of 1365 admissions. Eur J Cardiovasc Prev Rehabil. 2005;12(4):376–9.
Worrall-Carter L, McEvedy S, Wilson A, Rahman MA. Gender differences in presentation, coronary intervention, and outcomes of 28,985 acute coronary syndrome patients in Victoria, Australia. Women’s Health Issues. 2016;26(1):14–20.
Gulati M, Shaw LJ, Bairey Merz CN. Myocardial ischemia in women: lessons from the NHLBI WISE study. Clin Cardiol. 2012;35(3):141–8.
Yahagi K, Davis HR, Arbustini E, Virmani R. Sex differences in coronary artery disease: pathological observations. Atherosclerosis. 2015;239(1):260–7.
De Bacquer D, De Smedt D, Kotseva K, et al. Incidence of cardiovascular events in patients with stabilized coronary heart disease: the EUROASPIRE IV follow-up study. Eur J Epidemiol. 2019;34(3):247–58.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O'Brien SM, Boden WE, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395–407.
Acknowledgments
The Registry Executive Committee and Steering Committee of the EURObservational Research Programme (EORP) is acknowledged. Data collection was conducted by the EORP department from the ESC by Emanunuelle Fiorucci as Project Officer, Viviane Missiamenou and Florian Larras as Data Manager. All investigators are listed in Supplemental Appendix 1. The EUROASPIRE Study Group is grateful to the administrative staff, physicians, nurses, and other personnel in the hospitals in which the survey was carried out and to all patients who participated in the surveys.
Funding
The EuroAspire V survey was carried out under the auspices of the European Society of Cardiology, EURObservational Research Programme (EORP). Since the start of EORP, the following companies have supported the program: Amgen, Eli Lilly, Pfizer, Sanofi, Ferrer, Daiichi Sankyo and Novo Nordisk. Pieter Vynckier is financially supported by the ‘Fonds voor Hartchirurgie–Fonds pour la Chirurgie Cardiaque’.
Author information
Authors and Affiliations
Consortia
Contributions
PV, DDB, and DDS contributed to the conception and design. PV, GF, LR, LT, JB, KK, DW, TDB, SG, DDB, and DDS contributed to the acquisition, analysis, and interpretation. PV, DDB, and DDS drafted the manuscript. All authors critically revised the manuscript, gave final approval, and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that there is no conflict of interest.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Local Ethics Committee approval was available for each participating country.
Consent to Participate
Written informed consent was obtained from each participant by a signed declaration.
Consent for Publication
Written informed consent was obtained from each participant by a signed declaration.
Code Availability
No code availability.
Disclaimer
The sponsors of the EuroAspire surveys had no role in the design, data collection, data analysis, data interpretation, decision to publish, or writing the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 77 kb)
Rights and permissions
About this article
Cite this article
Vynckier, P., Ferrannini, G., Rydén, L. et al. Medical Treatment in Coronary Patients: Is there Still a Gender Gap? Results from European Society of Cardiology EUROASPIRE V Registry. Cardiovasc Drugs Ther 35, 801–808 (2021). https://doi.org/10.1007/s10557-020-07095-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-020-07095-6