Abstract
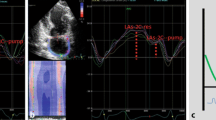
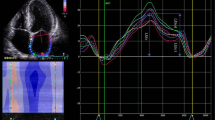
Previous studies using conventional echocardiographic measurements have reported subclinical left ventricular (LV) diastolic abnormalities in patients with Marfan syndrome (MFS). Left atrial (LA) strain allows an accurate categorization of LV diastolic dysfunction. We aimed to characterize LV myocardial performance in a cohort of MFS patients using STE-derived measurements (LV and LA strain) along with conventional echocardiographic parameters. We studied 127 adult patients with MFS (no prior cardiac surgery or significant valvular regurgitation) and 38 healthy controls. We performed detailed echocardiograms and selected left atrial reservoir strain (LASr) as a surrogate of impaired relaxation. Additionally, we searched for possible determinants of LASr in patients with MFS, with a special focus on the elastic properties of the aorta. In spite of lower E-wave, septal and lateral e’ velocities and average E/e’ ratio in MFS patients, all participants had normal diastolic function according to current guidelines. MFS patients exhibited reduced LV global longitudinal strain (19.3 ± 2.6 vs 21.6 ± 2.1%, p < 0.001) and reduced LASr (32.9 ± 8.5 vs 43.3 ± 7.8%, p < 0.001) compared to controls. In the MFS cohort, we found weak significant (p < 0.05) correlations between LASr and certain parameters: E/A ratio (R = 0.258), E wave (R = 0.226), aortic distensibility (R = 0.222), stiffness index (R = – 0.216), LV ejection fraction (R = 0.214), lateral e’ (R = 0.210), LV end-systolic volume index (R = − 0.210), LV global longitudinal strain (R = 0.201), septal e’ (R = 0.185). After multivariate analysis, only LV end-systolic volume index and E/A ratio maintained a weak independent association with LASr (R = − 0.220; p = 0.017 and R = 0.199; p = 0.046, respectively). In conclusion, LASr is reduced in patients with MFS, which may represent an early stage of LV diastolic dysfunction. LASr is not determined by the elastic properties of the aorta, suggesting that impaired myocardial relaxation is a primary condition in MFS.




Similar content being viewed by others
References
Robinson PN, Arteaga-Solis E, Baldock C, Collod-Béroud G, Booms P, De Paepe A, Dietz HC, Guo G, Handford PA, Judge DP et al (2006) The molecular genetics of Marfan syndrome and related disorders. J Med Genet 43:769–787. https://doi.org/10.1136/jmg.2005.039669
Judge DP, Dietz HC (2005) Marfan’s syndrome. Lancet 366:1965–1976. https://doi.org/10.1016/S0140-6736(05)67789-6
Whitfield AGW, Arnott WM, Stafford JL (1951) ‘Myocarditis’ and aortic hypoplasia in arachnodactyly: report of a case. Lancet 257:1387–1391. https://doi.org/10.1016/s0140-6736(51)92841-3
Chatrath R, Beauchesne LM, Connolly HM, Michels VV, Driscoll DJ (2003) Left ventricular function in the Marfan syndrome without significant valvular regurgitation. Am J Cardiol 91:914–916. https://doi.org/10.1016/s0002-9149(03)00039-0
Meijboom LJ, Timmermans J, van Tintelen JP, Nollen GJ, De Backer J, van den Berg MP, Boers GH, Mulder BJM (2005) Evaluation of left ventricular dimensions and function in Marfan’s syndrome without significant valvular regurgitation. Am J Cardiol 95:795–797. https://doi.org/10.1016/j.amjcard.2004.11.042
Alpendurada F, Wong J, Kiotsekoglou A, Banya W, Child A, Prasad SK, Pennell DJ, Mohiaddin RH (2010) Evidence for Marfan cardiomyopathy. Eur J Heart Fail 12:1085–1091. https://doi.org/10.1093/eurjhf/hfq127
Scherptong RWC, Vliegen HW, van der Wall EE, Hilhorst-Hofstee Y, Bax JJ, Scholte AJ, Delgado V (2011) Biventricular performance in patients with marfan syndrome without significant valvular disease: comparison to normal subjects and longitudinal follow-up. J Am Soc Echocardiogr 24(1392–1399):e1. https://doi.org/10.1016/j.echo.2011.09.004
de Witte P, Aalberts JJJ, Radonic T, Timmermans J, Scholte AJ, Zwinderman AH, Mulder BJM, Groenink M, van den Berg MP (2011) Intrinsic biventricular dysfunction in Marfan syndrome. Heart 97:2063–2068. https://doi.org/10.1136/heartjnl-2011-300169
Winther S, Williams LK, Keir M, Connelly KA, Bradley TJ, Rakowski H, Crean AM (2019) Cardiovascular magnetic resonance provides evidence of abnormal myocardial strain and primary cardiomyopathy in Marfan syndrome. J Comput Assist Tomogr 43(3):410–415. https://doi.org/10.1097/RCT.0000000000000863
Kiotsekoglou A, Moggridge JC, Bijnens BH, Kapetanakis V, Alpendurada F, Mullen MJ, Saha S, Nassiri DK, Camm J, Sutherland GR, Child AH (2009) Biventricular and atrial diastolic function assessment using conventional echocardiography and tissue-Doppler imaging in adults with Marfan syndrome. Eur J Echocardiogr 10:947–955. https://doi.org/10.1093/ejechocard/jep110
De Backer JF, Devos D, Segers P, Matthys D, François K, Gillebert TC, De Paepe AM, De Sutter J (2006) Primary impairment of left ventricular function in Marfan syndrome. Int J Cardiol 112:353–358. https://doi.org/10.1016/j.ijcard.2005.10.010
Rybczynski M, Koschyk DH, Aydin MA, Robinson PN, Brinken T, Franzen O, Berger J, Hofmann T, Meinertz T, von Kodolitsch Y (2007) Tissue Doppler imaging identifies myocardial dysfunction in adults with Marfan syndrome. Clin Cardiol 30:19–24. https://doi.org/10.1002/clc.3
Cameli M, Mandoli GE, Loiacono F, Dini FL, Henein M, Mondillo S (2016) Left atrial strain: a new parameter for assessment of left ventricular filling pressure. Heart Fail Rev 21:65–76. https://doi.org/10.1007/s10741-015-9520-9
Buggey J, Hoit BD (2018) Left atrial strain: measurement and clinical application. Curr Opin Cardiol 33:479–485. https://doi.org/10.1097/HCO.0000000000000537
Salvi P, Grillo A, Marelli S, Gao L, Salvi L, Viecca M, Di Blasio AM, Carretta R, Pini A, Parati G (2018) Aortic dilatation in Marfan syndrome: role of arterial stiffness and fibrillin-1 variants. J Hypertens 36:77–84. https://doi.org/10.1097/HJH.0000000000001512
Loeys B, Dietz HC, Braverman AC, Callewaert B, De Backer J, Devereux RB, Hilhorst-Hofstee Y, Jondeau G, Faivre L, Milewicz DM et al (2010) The revised Ghent nosology for the Marfan syndrome. J Med Genet 47:476–485. https://doi.org/10.1136/jmg.2009.072785
Homan TD, Bordes S, Cichowski E (2020) Physiology, pulse pressure. In: StatPearls. StatPearls Publishing, Treasure Island, FL. https://www.ncbi.nlm.nih.gov/books/NBK482408/. Accessed 4 Mar 2021
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1–39):e14. https://doi.org/10.1016/j.echo.2014.10.003
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314. https://doi.org/10.1016/j.echo.2016.01.011
Zoghbi WA, Adams D, Bonow RO, Enriquez-Sarano M, Foster E, Grayburn PA, Hahn RT, Han Y, Hung J, Lang RM et al (2017) Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the American Society of Echocardiography Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 30:303–371. https://doi.org/10.1016/j.echo.2017.01.007
Goldstein SA, Evangelista A, Abbara S, Arai A, Asch FM, Badano LP, Bolen MA, Connolly HM, Cuéllar-Calàbria H, Czerny M et al (2015) Multimodality imaging of diseases of the thoracic aorta in adults: from the American Society of Echocardiography and the European Association of Cardiovascular Imaging: endorsed by the Society of Cardiovascular Computed Tomography and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 28:119–182. https://doi.org/10.1016/j.echo.2014.11.015
Devereux RB, de Simone G, Arnett DK, Best LG, Boerwinkle E, Howard BV, Kitzman D, Lee ET, Mosley TH, Weder A, Roman MJ (2012) Normal limits in relation to age, body size and gender of two-dimensional echocardiographic aortic root dimensions in persons ≥15 years of age. Am J Cardiol 110:1189–1194. https://doi.org/10.1016/j.amjcard.2012.05.063
Badano LP, Kolias TJ, Muraru D, Abraham TP, Aurigemma G, Edvardsen T, D’Hooge J, Donal E, Fraser AG, Marwick T et al (2018) Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 19:591–600. https://doi.org/10.1093/ehjci/jey042
Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, Pedri S, Ito Y, Abe Y, Metz S et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16(1):1–11. https://doi.org/10.1093/ehjci/jeu184
Demolder A, von Kodolitsch Y, Muiño-Mosquera L, De Backer J (2020) Myocardial function, heart failure and arrhythmia in Marfan syndrome: a systematic literature review. Diagnostics (Basel) 10:751. https://doi.org/10.3390/diagnostics10100751
Kiotsekoglou A, Saha S, Moggridge JC, Kapetanakis V, Govindan M, Alpendurada F, Mullen MJ, Nassiri DK, Camm J, Sutherland GR et al (2011) Impaired biventricular deformation in Marfan syndrome: a strain and strain rate study in adult unoperated patients. Echocardiography 28:416–430. https://doi.org/10.1111/j.1540-8175.2010.01359.x
Thomas L, Muraru D, Popescu BA, Sitges M, Rosca M, Pedrizzetti G, Henein MY, Donal E, Badano LP (2020) Evaluation of left atrial size and function: relevance for clinical practice. J Am Soc Echocardiogr 33:934–952. https://doi.org/10.1016/j.echo.2020.03.021
Morris DA, Takeuchi M, Krisper M, Köhncke C, Bekfani T, Carstensen T, Hassfeld S, Dorenkamp M, Otani K, Takigiku K et al (2015) Normal values and clinical relevance of left atrial myocardial function analysed by speckle-tracking echocardiography: multicentre study. Eur Heart J Cardiovasc Imaging 16:364–372. https://doi.org/10.1093/ehjci/jeu219
Singh A, Medvedofsky D, Mediratta A, Balaney B, Kruse E, Ciszek B, Shah AP, Blair JE, Maffessanti F, Addetia K et al (2019) Peak left atrial strain as a single measure for the non-invasive assessment of left ventricular filling pressures. Int J Cardiovasc Imaging 35:23–32. https://doi.org/10.1007/s10554-018-1425-y
Singh A, Addetia K, Maffessanti F, Mor-Avi V, Lang RM (2017) LA strain for categorization of LV diastolic dysfunction. JACC Cardiovasc Imaging 10:735–743. https://doi.org/10.1016/j.jcmg.2016.08.014
Cameli M, Lisi M, Focardi M, Reccia R, Natali BM, Sparla S, Mondillo S (2012) Left atrial deformation analysis by speckle tracking echocardiography for prediction of cardiovascular outcomes. Am J Cardiol 110:264–269. https://doi.org/10.1016/j.amjcard.2012.03.022
Ersbøll M, Andersen MJ, Valeur N, Mogensen UM, Waziri H, Møller JE, Hassager C, Søgaard P, Køber L (2013) The prognostic value of left atrial peak reservoir strain in acute myocardial infarction is dependent on left ventricular longitudinal function and left atrial size. Circ Cardiovasc Imaging 6:26–33. https://doi.org/10.1161/CIRCIMAGING.112.978296
Santos ABS, Roca GQ, Claggett B, Sweitzer NK, Shah SJ, Anand IS, Fang JC, Zile MR, Pitt B, Solomon SD, Shah AM (2016) The prognostic relevance of left atrial dysfunction in heart failure with preserved ejection fraction. Circ Heart Fail 9:e002763. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002763
Kim J, Yum B, Palumbo MC, Sultana R, Wright N, Das M, You C, Moskowitz CS, Levine RA, Devereux RB, Weinsaft JW (2020) Left atrial strain impairment precedes geometric remodeling as a marker of post-myocardial infarction diastolic dysfunction. JACC Cardiovasc Imaging 13:2099–2113. https://doi.org/10.1016/j.jcmg.2020.05.041
Delling FN, Vasan RS (2014) Epidemiology and pathophysiology of mitral valve prolapse: new insights into disease progression, genetics, and molecular basis. Circulation 129:2158–2170. https://doi.org/10.1161/CIRCULATIONAHA.113.006702
Gan GCH, Bhat A, Chen HHL, Fernandez F, Byth K, Eshoo S, Thomas L (2020) Determinants of LA reservoir strain: Independent effects of LA volume and LV global longitudinal strain. Echocardiography. https://doi.org/10.1111/echo.14922
Sun BJ, Park J-H, Lee M, Choi J-O, Lee J-H, Shin M-S, Kim M-J, Jung HO, Park JR, Sohn IS et al (2020) Normal reference values for left atrial strain and its determinants from a large Korean Multicenter Registry. J Cardiovasc Imaging 28:186–198. https://doi.org/10.4250/jcvi.2020.0043
Inoue K, Khan FH, Remme EW, Ohte N, García-Izquierdo E, Chetrit M, Moñivas-Palomero V, Mingo-Santos S, Andersen ØS, Gude E et al (2021) Determinants of left atrial reservoir and pump strain and use of atrial strain for evaluation of left ventricular filling pressure. Eur Heart J Cardiovasc Imaging. https://doi.org/10.1093/ehjci/jeaa415
Thomas L, Abhayaratna WP (2017) Left atrial reverse remodeling: mechanisms, evaluation, and clinical significance. JACC Cardiovasc Imaging 10:65–77. https://doi.org/10.1016/j.jcmg.2016.11.003
Loeper F, Oosterhof J, van den Dorpel M, van der Linde D, Lu Y, Robertson E, Hambly B, Jeremy R (2016) Ventricular-vascular coupling in Marfan and Non-Marfan aortopathies. J Am Heart Assoc 5:e003705. https://doi.org/10.1161/JAHA.116.003705
Savolainen A, Nisula L, Keto P, Hekali P, Viitasalo M, Kaitila I, Kupari M (1994) Left ventricular function in children with the Marfan syndrome. Eur Heart J 15:625–630. https://doi.org/10.1093/oxfordjournals.eurheartj.a060558
Das BB, Taylor AL, Yetman AT (2006) Left ventricular diastolic dysfunction in children and young adults with Marfan syndrome. Pediatr Cardiol 27:256–258. https://doi.org/10.1007/s00246-005-1139-5
Funding
This work was supported by a grant from Comunidad de Madrid (AORTASANA-CM; B2017/BMD-3676).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no conflict of interest.
Ethical approval
Ethics approval was obtained from the Research Ethics Committee of Puerta de Hierro University Hospital in Madrid (Spain). Each participant provided written informed consent after receiving a detailed description of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
García-Izquierdo, E., Moñivas-Palomero, V., Forteza, A. et al. Left atrial strain in the assessment of diastolic function: providing new insights into primary myocardial dysfunction in Marfan syndrome. Int J Cardiovasc Imaging 37, 2735–2745 (2021). https://doi.org/10.1007/s10554-021-02247-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02247-7