Abstract
Purpose
Veterans have a suicide rate 1.5 times higher than the non-veteran population. The Department of Veterans Affairs (VA) implemented suicide risk screening recommendations in 2018. This project assessed the impact of mental health (MH) prescribers on these recommendations and identified areas of improvement.
Methods
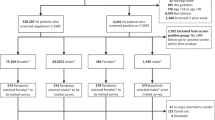
Seventy MH Clinical Pharmacy Specialists (CPS) and 52 other MH prescribers were included. Patients with a positive question nine (from the Patient Health Questionnaire-9) and a same-day Columbia Suicide Severity Rating Scale (C-SSRS) between 11/01/18 and 11/01/19 at a VA system were reviewed. Completion of same-day Comprehensive Suicide Risk Evaluation (CSRE), same-day Suicide Prevention Safety Plan (SPSP), number of patients who were not offered naloxone despite access to opioids, and number of patients who were not offered a gunlock despite access to firearms were compared between groups. Time from C-SSRS to suicidal behavior was compared between those who did and did not receive a same-day CSRE.
Results
MH CPS were significantly more likely to complete a same-day CSRE (p = 0.0201) and SPSP (p < 0.001) when recommended. Naloxone outcomes were not assessed due to availability of only one data point. Rates of gunlock offers did not differ significantly between groups (Fisher’s exact test, p = 0.3189) however there was no documentation stating why they were not offered when appropriate 40% of the time. Time to suicidal behavior did not vary across patients based on CSRE completion (p = 0.16).
Conclusion
MH CPS play an important role in suicide risk screening for veterans. There is a need for improvement regarding the offering and documentation of firearm risk mitigation strategies.


Similar content being viewed by others
References
Carpenter, D. M., Lavigne, J. E., Roberts, C. A., Zacher, J., & Colmenares, E. W. (2018). A review of suicide prevention programs and training policies for pharmacists. Journal of the American Pharmacists Association, 58(5), 522–529. https://doi.org/10.1016/j.japh.2018.05.004.
Cdc.gov. (2019). Preventing suicide. https://www.cdc.gov/violenceprevention/suicide/fastfact.html
Clay, P. G., Burns, A. L., Isetts, B. J., Hirsch, J. D., Kliethermes, M. A., & Planas, L. G. (2019). PaCIR: A tool to enhance pharmacist patient care intervention reporting. Journal of the American Pharmacists Association, 59(5), 615–623. https://doi.org/10.1016/j.japh.2019.07.008.
Elbogen, E. B., Wagner, H. R., Kimbrel, N. A., Brancu, M., Naylor, J., Graziano, R., Crawford, E., & VA Mid-Atlantic MIRECC Workgroup. (2018). Risk factors for concurrent suicidal ideation and violent impulses in military veterans. Psychological Assessment, 30(4), 425–435. https://doi.org/10.1037/pas0000490.
Gallup.com. (2019). Honesty/ethics in professions. https://news.gallup.com/poll/1654/honesty-ethics-professions.aspx
Green, J. D., Kearns, J. C., Rosen, R. C., Keane, T. M., & Marx, B. P. (2018). Evaluating the effectiveness of safety plans for military veterans: Do safety plans tailored to veteran characteristics decrease suicide risk? Behavior Therapy, 49(6), 931–938. https://doi.org/10.1016/j.beth.2017.11.005.
Kessler, R. C., Bauer, M. S., Bishop, T. M., Demler, O. V., Dobscha, S. K., Gildea, S. M., Goulet, J. L., Karras, E., Kreyenbuhl, J., Landes, S. J., Liu, H., Luedtke, A. R., Mair, P., McAuliffe, W. H. B., Nock, M., Petukhova, M., Pigeon, W. R., Sampson, N. A., Smoller, J. W., et al. (2020). Using administrative data to predict suicide after psychiatric hospitalization in the veterans health administration system. Frontiers in Psychiatry, 11. https://doi.org/10.3389/fpsyt.2020.00390.
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x.
Military The Columbia Lighthouse Project. (n.d.). The Columbia lighthouse project. Retrieved May 28, 2020, from https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/military/
Murphy, A. L., Hillier, K., Ataya, R., Thabet, P., Whelan, A. M., O’Reilly, C., & Gardner, D. (2017). A scoping review of community pharmacists and patients at risk of suicide. Canadian Pharmacists Journal, 150(6), 366–379. https://doi.org/10.1177/1715163517733482.
Office of Mental Health and Suicide Prevention. (n.d.). 2019 national veteran suicide prevention annual report. U.S. Department of Veterans Affairs. Retrieved September 23, 2019, from https://www.mentalhealth.va.gov/docs/data-sheets/2019/2019_National_Veteran_Suicide_Prevention_Annual_Report_508.pdf
Painter, N. A., Kuo, G. M., Collins, S. P., Palomino, Y. L., & Lee, K. C. (2018). Pharmacist training in suicide prevention. Journal of the American Pharmacists Association, 58(2), 199–204.e2. https://doi.org/10.1016/j.japh.2017.12.007.
Roaten, K., Johnson, C., Genzel, R., Khan, F., & North, C. S. (2018). Development and implementation of a universal suicide risk screening program in a safety-net hospital system. The Joint Commission Journal on Quality and Patient Safety, 44(1), 4–11. https://doi.org/10.1016/j.jcjq.2017.07.006.
SQUIRE | SQUIRE 2.0 Guidelines. (n.d.). Retrieved June 22, 2020, from http://squire-statement.org/index.cfm?fuseaction=Page.ViewPage&PageID=471
Stanley, B., & Brown, G. (2012). Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive Behavioral Practice, 19(2), 256–264.
Watkins, K. E., Smith, B., Akincigil, A., Sorbero, M. E., Paddock, S., Woodroffe, A., Huang, C., Crystal, S., & Pincus, H. A. (2016). The quality of medication treatment for mental disorders in the Department of Veterans Affairs and in private-sector plans. Psychiatric Services, 67(4), 391–396. https://doi.org/10.1176/appi.ps.201400537.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical Approval
This project was conducted retrospectively from data obtained for clinical purposes. Authors consulted extensively with the IRB of the South Texas Veterans Health Care System and that of UT Health San Antonio who determined that this project did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of both entities.
Informed Consent
This project was conducted retrospectively from data obtained for clinical purposes. Authors consulted extensively with the IRB of the South Texas Veterans Health Care System and of UT Health San Antonio who determined that this project did not need informed consent since it utilized existing data and no identifiable data objects were recorded. An IRB official waiver of ethical approval was granted from the IRB of both entities.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
PaCIR and SQUIRE 2.0 guidelines for pharmacist interventions and quality improvement projects were used in developing this manuscript.
Rights and permissions
About this article
Cite this article
Laguado, S.A., Steavenson, R. & Mehvar, M. Areas of Improvement in Suicide Risk Identification, Assessment, and Risk Mitigation Documentation by Mental Health Prescribers at a Veterans Affairs Health Care System. Adm Policy Ment Health 48, 633–638 (2021). https://doi.org/10.1007/s10488-020-01097-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-020-01097-0