Abstract
Therapy-related myelodysplastic syndrome (t-MDS) is defined as a complication in patients with cancer following exposure to chemotherapy and/or radiotherapy and has an inferior outcome compared with de novo myelodysplastic syndrome (de novo MDS). This study aimed to estimate and compare the clinical outcomes of haploidentical stem cell transplantation (haplo-HSCT) for t-MDS and de novo MDS. We retrospectively analyzed 96 patients with MDS who received haplo-HSCT between January 2015 and December 2021. Eleven patients with t-MDS and 85 patients with de novo MDS were matched using the case-pair method in a 1:8 ratio with the following pairing criteria: (1) sex, (2) age (± 5 years), (3) year of haplo-HSCT (± 2 years), and (4) blast cell counts (≥ 5% or not). The 3-year overall survival and disease-free survival after haplo-HSCT for t-MDS versus de novo MDS patients were 72.7% versus 75.1% (P = 0.99) and 54.5% versus 67.0% (P = 0.50), respectively. The 3-year cumulative incidence of relapse was 36.4% versus 15.5% (P = 0.08), respectively. In multivariate analysis, there was no difference in relapse between t-MDS and de novo MDS. The 3-year cumulative non-relapse mortality rates were 9.1% versus 17.6% (P = 0.45), respectively. This study confirmed the comparable clinical outcomes of haplo-HSCT on the prognosis of t-MDS and de novo MDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myelodysplastic syndromes (MDS) are a group of myeloid neoplasms characterized by bone marrow dysplasia, ineffective hematopoiesis, peripheral blood cytopenia, and a high-risk transformation to acute myeloid leukemia (AML) [1,2,3]. De novo MDS and t-MDS are subtypes of MDS with different biology and prognosis. t-MDS is defined as a complication of patients with cancer following exposure to chemotherapy and/or radiotherapy and has an inferior outcome compared with de novo MDS, with a median survival of one year or less [4,5,6,7,8]. According to the 2022 WHO classification [9], myeloid neoplasms post-cytotoxic tumor (MN-pCT) replace the previous diagnosis called therapy-related myeloid neoplasms (t-MN), including both t-AML and t-MDS [10]. According to the 2022 European LeukemiaNet recommendations for AML, therapy-related factors, including radiotherapy, chemotherapy, and immune interventions and secondary AML that progressed from MDS and MDS/MPN (specify type), are adverse prognostic factors [11]. At present, MDS is merely classified and diagnosed according to morphological, flow cytometry, cytogenetic and molecular factors. Although t-MDS has not been regarded as a poor prognostic factor in various MDS classifications, it should also be taken into consideration.
Allogeneic hematopoietic cell transplantation (allo-HSCT) remains the only curative therapy strategy for t-MDS to date [5, 8, 12, 13]. Haploidentical stem cell transplantation (haplo-HSCT) provides an attractive treatment option for patients lacking an available identical sibling donor (ISD) who need urgent transplantation [14, 15]. There have been considerable advances in the field of haplo-HSCT, such as donor selection, conditioning regimens, and graft-versus-host disease prophylaxis, which have successfully improved the clinical outcomes of patients receiving haplo-HSCT. Our previous studies demonstrated comparable efficacy between haploidentical hematopoietic cell transplantation (haplo-HSCT) and identical sibling transplant for MDS [16]. However, prior studies on t-MDS did not separate haplo-HSCT from other types of allo-HSCT [4, 6, 17, 18]. Therefore, in this study, we compared and analyzed the clinical outcomes of haplo-HSCT for t-MDS with those of de novo MDS.
Materials and methods
Patients
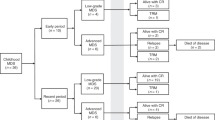
We retrospectively reviewed the data of MDS patients who received haplo-HSCT at the Institute of Hematology, Peking University, Beijing, China, between January 2015 and December 31, 2021. We identified 11 t-MDS patients who received haplo-HSCT and used the case-pair method to match the control subjects in a 1:8 ratio with the following pairing criteria: (1) sex, (2) age (± 5 years), (3) year of haplo-HSCT (± 2 years), and (4) blast cell counts (≥ 5% or not). This matching method strictly controlled the confounding effect of time in the analysis process. Eighty-five patients with de novo MDS who received haplo-HSCT were finally matched as a set of control cases owing to the fact that 2 patients in t-MDS group did not achieve a 1:8 pairing. Eventually, 96 patients were eligible as subjects for this study. Informed consent was obtained from all patients for being included in the study. All methods were carried out in accordance with the Declaration of Helsinki, and the protocol was approved by the ethics committee of Peking University People's Hospital. Cytogenetic risk was defined based on the revised International Prognostic Scoring System (IPSS-R) criteria [19].
Transplant procedure
All patients received myeloablative conditioning (MAC) regimen. The uniform conditioning regimen for haploidentical donors (HID) was cytarabine (4 g/m2 per day, intravenous infusion, days − 10 to − 9), busulfan (3.2 mg/kg per day, intravenous infusion, days − 8 to − 6), cyclophosphamide (1.8 g/m2 per day, intravenous infusion, days − 5 to − 4), semustine (250 mg/m2 per day, oral administration, day − 3), and rabbit antithymocyte globulin (ATG) (2.5 mg/kg per day, intravenous infusion, days − 5 to − 2) [20]. Granulocyte colony stimulating factor (G-CSF) (5 μg/kg) mobilizing bone marrow and/or peripheral blood grafts were infused on the day of collection for HSCT. GVHD prophylaxis consisted of cyclosporine (2.5 mg/kg, intravenous infusion, since day − 9), mycophenolate mofetil (1.0 g, oral administration, since day − 9), and short-term methotrexate (15 mg/m2, intravenous infusion, on day 1 and 10 mg/m2 on days 3, 5, and 11) for all patients. Bone marrow samples were evaluated at 1, 2, 3, 4.5, 6, 9, and 12 months after haplo-HSCT, and at every 6 months after thereafter, to monitor minimum residual disease (MRD) after haplo-HSCT [21].
Definitions
The endpoints of our study were overall survival (OS) and disease-free survival (DFS), while the secondary observation targets included non-relapse mortality (NRM), the incidence of relapse and the incidences of acute GVHD (aGVHD), chronic GVHD (cGVHD) and influencing factors for clinical outcomes. OS time was defined as the time from transplantation to death from any cause or the last follow-up in surviving patients. DFS was defined as the time from transplantation to relapse or death from any cause. Relapse was defined as morphological evidence of the disease discovered in texting samples from the peripheral blood, bone marrow, or extramedullary sites or else by the recurrence and sustained presence of pre-transplantation chromosomal abnormalities [14]. NRM was defined as the time from transplantation to death from any cause without relapse. All data were calculated from the day of graft infusion. Neutrophil engraftment was defined as an absolute neutrophil count ≥ 0.5 × 109/L on three consecutive days. Platelet engraftment was defined as no transfusion for 7 consecutive days and platelet count ≥ 20 × 109/L. aGVHD and cGVHD were defined according to published criteria [22, 23].
Statistical analysis
The endpoint of the last follow-up for all survivors was April 30, 2023. The median follow-up time of survivors was 34.9 months (range, 17.8–100.1 months). Baseline patient, disease, and transplant-related characteristics were analyzed between patients with de novo MDS and those with t-MDS by using the χ2 test and Fisher’s exact test for categorical variables and the Mann–Whitney U test for continuous variables. OS and DFS were calculated by using the Kaplan–Meier estimator with the log-rank test. The cumulative incidence of GVHD, relapse and NRM were calculated by using competing risk analysis. For GVHD, death from any cause was a competing event. For NRM, relapse was a competing event, and for relapse, NRM was a competing event. Multivariable analyses were performed using Cox proportional hazards regression to identify independent risk factors for NRM, relapse, DFS, and OS. The variables in the Cox proportional hazards regression model were as follows: patient age (< 35 years vs. ≥ 35 years), interval between MDS diagnosis and haplo-HSCT (interval < 30 months vs. interval ≥ 30 months), cytogenetic risk (high cytogenetic risk vs. non-high cytogenetic risk), graft type (BM + PB vs. PB), platelet engraftment (yes vs. no), treatment for t-MDS/de novo MDS prior to haplo-HSCT (chemotherapy vs. supportive care only) and MDS subtype (de novo MDS vs. t-MDS). All variables with P < 0.1 in the univariate analysis were allowed to be analyzed in the multivariate regression. The MDS subtype (de novo MDS vs. t-MDS) was forced into the Cox proportional hazards model regardless of the P value. Two-sided P values < 0.05 were considered statistically significant. Data analyses were calculated by using the Statistical Package for the Social Sciences (SPSS) software (SPSS Inc., Chicago, IL, USA), whereas competing risk analysis was performed using R software (version 3.2.1; http://www.r-project.org).
Results
Patient characteristics
Table 1 summarizes the characteristics of the 96 patients enrolled in this study. Among them, 11 (11.5%) were diagnosed with t-MDS, and 85 (88.5%) had de novo MDS. Two patients in t-MDS group did not achieve a 1:8 pairing. The median age of all patients was 48 years (range, 2–62 years) and the median age in t-MDS group and de novo MDS group was 51 years (range, 6–58 years) and 48 years (range, 2–62 years), respectively (P = 0.83). The median interval from MDS diagnosis to haplo-HSCT was 6 months (1–192 months). A higher proportion of t-MDS patients was found with the high-risk cytogenetic abnormalities compared to de novo MDS (45.5% vs. 18.8%, P = 0.04). Treatment for t-MDS prior to haplo-HSCT included supportive treatment (n = 5, 45.5%) and chemotherapy (n = 6, 54.5%).
Among the 11 patients with t-MDS, 6 (54.5%) patients had prior hematological malignancy, including AML (n = 3), chronic myeloid leukemia (n = 1), acute lymphoblastic leukemia (n = 1), and non-Hodgkin lymphoma (n = 1), and 5 (45.5%) patients had a history of solid malignancy, including 2 (18.2%) with lung cancer, 2 (18.2%) with genital system carcinoma, and 1 (9.1%) with thyroid carcinoma. The median latency time from the diagnosis of primary cancer and t-MDS was 57 months (22.7–120 months). None of the patients received radiotherapy. The median cycle of chemotherapy was 7 (range, 5–28 cycles). The chemotherapy drugs principally included alkylating agents, topoisomerase, and antimetabolic drugs. All t-MDS patients with solid malignancy underwent surgical resection. The primary cancer of all patients with t-MDS was cured at the time of haplo-HSCT. The median interval from t-MDS diagnosis to haplo-HSCT was 5 months (2–24 months).
Engraftment and GVHD
All patients showed complete donor chimerism after transplantation. Incomplete neutrophil recovery was observed in 2 patients with de novo MDS. The median neutrophil engraftment times in the t-MDS and control cohort were 13 days (range, 11–20 days) and 12 days (range, 9–26 days), respectively (P = 0.35). Eight patients with de novo MDS failed to achieve platelet engraftment. The median platelet engraftment times of patients in the t-MDS and control cohort were 14 days (range, 9–102 days) and 15 days (range, 9–119 days), respectively (P = 0.84).
On 100 days after transplantation, the cumulative incidences of grade II–IV aGVHD in the t-MDS and control cohort were 27.3% and 32.9%, respectively (P = 0.69; Fig. 1a). The cumulative incidence of all-grade cGVHD in the t-MDS and control cohort were 27.3% and 31.2%, respectively (P = 0.74; Fig. 1b).
Relapse
Four patients (36.4%) in the t-MDS group and 13 (15.3%) in control cohort experienced relapse at a median of 7.3 months (range, 3.0–18.2 months) after haplo-HSCT. The relapse times of patients with t-MDS were 3.1, 3.6, 7.9, and 10.3 months after haplo-HSCT. The median times of relapse in the t-MDS and de novo MDS were 5.8 months (range, 3.1–10.3 months) and 7.3 months (range, 3–18.2 months), respectively. None of t-MDS patients experienced the recurrence of primary cancer. The 3-year cumulative incidence of relapse in the t-MDS group and control cohort was 36.4% and 15.5%, respectively (P = 0.08; Fig. 2a). In multivariable analysis, the incidence of relapse seemed to be comparable between patients with t-MDS and de novo MDS (Table 2). In univariate and multivariable analysis, high-risk cytogenetics was significantly correlated with a higher relapse rate [HR 2.758 (95% CI: 1.049–7.253), P = 0.040].
NRM
One patient (9.1%) in the t-MDS group and 15 patients (17.7%) in the de novo MDS group died of NRM. The median time of NRM after haplo-HSCT was 2.4 months (range, 0.4–17 months). The NRM time of the patient in the t-MDS group was 11.5 months, and she died of infection. No t-MDS patients died of the recurrence of primary cancer. Patients in the control group died of infection (66.7%) and GVHD (13.3%). The cumulative incidences of NRM in the t-MDS group and control cohort were 9.1% and 17.6%, respectively (P = 0.45; Fig. 2b). In multivariable analysis for NRM, platelet engraftment was an independent significant factor [HR 0.012 (95% CI: 0.002–0.066), P = 0.000] (Table 2).
DFS and OS
The 3-year DFS for the t-MDS group and the de novo MDS group were 54.5% and 67.0%, respectively, P = 0.50 (Fig. 3a). The 3-year OS were 72.7% and 75.1%, respectively, P = 0.99 (Fig. 3b). In univariate analysis, the absence of platelet engraftment was significantly associated with higher DFS and OS [DFS: HR 0.096 (95% CI: 0.040–0.228), P = 0.000; OS: HR 0.069 (95% CI: 0.028–0.174), P = 0.000]. In multivariable analysis for DFS and OS, platelet engraftment remained a significant predictive variable [DFS: HR 0.096 (95% CI: 0.040–0.228), P = 0.000; OS: HR 0.085 (95% CI: 0.034–0.216), P = 0.000]. However, OS and DFS were not influenced by MDS type (t-MDS vs. de novo MDS) (Table 2).
Discussion
To the best of our knowledge, this study is the first to systematically compare the clinical outcomes of haplo-HSCT on t-MDS and de novo MDS. Our study shows that the OS, DFS, relapse, and NRM of t-MDS after haplo-HSCT are comparable to those of de novo MDS.
In this study, we systematically analyzed the original case data of 11 t-MDS. Hematological malignancies were the most common primary cancer (54.5%). Kuendgen A et al. found that hematological malignancies (43%) were the most common primary tumor of t-MDS [4]. Our results are consistent with those of previous studies. In our study, the 3-year OS, DFS, relapse, and NRM rates in t-MDS patients were 72.7%, 54.5%, 36.4%, and 9.1%, respectively. In 2021, the CIBMTR reported that the OS, DFS, relapse, and NRM incidences in t-MDS after allo-HSCT were 26.9%, 19.4%, 46.2%, and 33.7%, respectively [17]. Compared with the results of the CIBMTR, our clinical outcomes of t-MDS after haplo-HSCT are encouraging. Several possible explanations might account for these findings. First, the median age of our group was younger than that of the CIBMTR (48 years vs. 58.6 years). In previous studies of t‐MNs from CIBMTR and EBMT, older age was identified as an independent risk factor for post‐transplant survival [8, 18]. Second, the data of CIBMTR of allo-HSCT were between 2000 and 2014, during an early era of transplantation, while the median year of our data was 2019 (range, 2015–2021). Third, patients in our study merely received haplo-HSCT, whereas the CIBMTR study concentrated on HLA identical sibling and unrelated donor settings. Survival was promising owing to the stronger graft-versus-leukemia effects of haploidentical HSCT [24]. Fourth, our patients all received MAC, in contrast to the study of CIBMTR in which 51% of patients received reduced-intensity conditioning (RIC). A previous study of patients with MDS eligible for either the MAC or RIC regimens and long-term follow-up demonstrated a survival advantage for patients who received MAC [25]. Fifth, our center has uniform treatment schemes including conditioning regimens and GVHD prophylaxis, whereas the CIBMTR study analyzed data from multiple centers with heterogeneous patient groups and treatment methods.
In this study, the clinical outcomes including the rates of relapse, OS, DFS, and NRM after haplo-HSCT for patients with t-MDS were comparable to those with de novo MDS. However, relapse seems to be a major challenge of haplo-HSCT for patients with t-MDS, although the P value in univariate and multivariate analyses did not indicate a significant difference. The trend of a high relapse rate may be related to the overall small number of patients in our retrospective study, so it needs to be further confirmed by prospective large samples of studies. It is might associated with high-risk cytogenetics [5, 18], because that the proportion of patients with high-risk cytogenetic abnormalities was higher in t-MDS (45.5%) than in de novo MDS (18.8%) (P = 0.04). Ibrahim Aldoss et al. found comparable outcomes between t-MDS and de novo MDS after HLA identical sibling and unrelated donor transplants (OS, 49.9% vs. 53.9%, P = 0.61; relapse-free survival, 47.2% vs. 49.5%, P = 0.68) [5]. However, we found that the OS (72.7% vs. 75.1%; P = 0.99) and DFS (54.5% vs. 67.0%; P = 0.50) of t-MDS and de novo MDS in our study seem more encouraging than that in previous studies, which might because of that the age of patients were young and all received haplo-HSCT with a myeloablative conditioning regimen in our study. Therefore, haplo-HSCT is an optimum and curative therapeutic option for patients with t-MDS. In our study, platelet engraftment was an independent significant factor for OS, DFS and NRM. Our previous study indicated that primary prolonged isolated thrombocytopenia was significantly associated with inferior overall survival and higher TRM, which is consistent with this study [26].
Limitations still exist in our study. First, our study is a single-center and retrospective study, which might lead to selection bias. Second, the number of t-MDS cases in our center was relatively small, which might lead to statistical bias. Third, because the primary cancer of some t-MDS patients was not diagnosed and treated in our center, we lack some data on the details of the initial therapy of the primary cancer. Fourth, our data began in 2015, while next-generation sequencing (NGS) was carried out in our center in 2018, so part of the data lacked the results of NGS. Therefore, we expect more multicenter and prospective studies to confirm our conclusions, and we also hope that research will further prove the biological characteristics of t-MDS in future.
In conclusion, our study first demonstrated that t-MDS has comparable outcomes to de novo MDS after haplo-HSCT. Therefore, haplo-HSCT is one of the feasible options for t-MDS patients if there is no HLA-matched sibling. Additionally, large, well-designed, prospective randomized trials are needed to further confirm these conclusions.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Malcovati L, Hellström-Lindberg E, Bowen D, et al. Diagnosis and treatment of primary myelodysplastic syndromes in adults: Recommendations from the european leukemianet. Blood. 2013;122(17):2943–64. https://doi.org/10.1182/blood-2013-03-492884.
Cazzola M. Myelodysplastic syndromes. N Engl J Med. 2020;383(14):1358–74. https://doi.org/10.1056/NEJMra1904794.
Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the world health organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. https://doi.org/10.1182/blood-2016-03-643544.
Kuendgen A, Nomdedeu M, Tuechler H, et al. Therapy-related myelodysplastic syndromes deserve specific diagnostic sub-classification and risk-stratification-an approach to classification of patients with t-mds. Leukemia. 2021;35(3):835–49. https://doi.org/10.1038/s41375-020-0917-7.
Aldoss I, Pham A, Li SM, et al. Favorable impact of allogeneic stem cell transplantation in patients with therapy-related myelodysplasia regardless of tp53 mutational status. Haematologica. 2017;102(12):2030–8. https://doi.org/10.3324/haematol.2017.172544.
Itonaga H, Kida M, Hamamura A, et al. Outcome of therapy-related myelodysplastic syndrome and oligoblastic acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation: a propensity score matched analysis. Hematol Oncol. 2022. https://doi.org/10.1002/hon.2991.
Borthakur G, Estey AE. Therapy-related acute myelogenous leukemia and myelodysplastic syndrome. Curr Oncol Rep. 2007;9(5):373–7. https://doi.org/10.1007/s11912-007-0050-z.
Litzow MR, Tarima S, Pérez WS, et al. Allogeneic transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia. Blood. 2010;115(9):1850–7. https://doi.org/10.1182/blood-2009-10-249128.
Khoury JD, Solary E, Abla O, et al. The 5th edition of the world health organization classification of haematolymphoid tumours: Myeloid and histiocytic/dendritic neoplasms. Leukemia. 2022;36(7):1703–19. https://doi.org/10.1038/s41375-022-01613-1.
Candelaria M, Dueñas-Gonzalez A. Therapy-related myelodysplastic syndrome. Expert Opin Drug Saf. 2015;14(5):655–65. https://doi.org/10.1517/14740338.2015.1014340.
Döhner H, Wei AH, Appelbaum FR, et al. Diagnosis and management of aml in adults: 2022 recommendations from an international expert panel on behalf of the eln. Blood. 2022;140(12):1345–77. https://doi.org/10.1182/blood.2022016867.
Fianchi L, Pagano L, Piciocchi A, et al. Characteristics and outcome of therapy-related myeloid neoplasms: report from the italian network on secondary leukemias. Am J Hematol. 2015;90(5):E80–5. https://doi.org/10.1002/ajh.23966.
Abou Zahr A, Kavi AM, Mukherjee S, et al. Therapy-related myelodysplastic syndromes, or are they? Blood Rev. 2017;31(3):119–28. https://doi.org/10.1016/j.blre.2016.11.002.
Mo XD, Zhang XH, Xu LP, et al. Haploidentical hematopoietic stem cell transplantation for myelodysplastic syndrome. Biol Blood Marrow Transplant. 2017;23(12):2143–50. https://doi.org/10.1016/j.bbmt.2017.08.026.
Chang YJ, Luznik L, Fuchs EJ, et al. How do we choose the best donor for t-cell-replete, hla-haploidentical transplantation? J Hematol Oncol. 2016;9:35. https://doi.org/10.1186/s13045-016-0265-2.
Wang Y, Wang HX, Lai YR, et al. Haploidentical transplant for myelodysplastic syndrome: registry-based comparison with identical sibling transplant. Leukemia. 2016;30(10):2055–63. https://doi.org/10.1038/leu.2016.110.
Metheny L, Callander NS, Hall AC, et al. Allogeneic transplantation to treat therapy-related myelodysplastic syndrome and acute myelogenous leukemia in adults. Transplant Cell Ther. 2021;27(11):923.e1-.e12. https://doi.org/10.1016/j.jtct.2021.08.010.
Kröger N, Brand R, van Biezen A, et al. Risk factors for therapy-related myelodysplastic syndrome and acute myeloid leukemia treated with allogeneic stem cell transplantation. Haematologica. 2009;94(4):542–9. https://doi.org/10.3324/haematol.2008.000927.
Greenberg PL, Tuechler H, Schanz J, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. https://doi.org/10.1182/blood-2012-03-420489.
Tang F, Mo X, Zhang X, et al. Influence of the degree of donor bone marrow hyperplasia on patient clinical outcomes after allogeneic hematopoietic stem cell transplantation. Sci China Life Sci. 2020;63(1):138–47. https://doi.org/10.1007/s11427-018-9509-y.
Zhao XS, Jin S, Zhu HH, et al. Wilms’ tumor gene 1 expression: an independent acute leukemia prognostic indicator following allogeneic hematopoietic sct. Bone Marrow Transplant. 2012;47(4):499–507. https://doi.org/10.1038/bmt.2011.121.
Thomas ED, Storb R, Clift RA, et al. Bone-marrow transplantation (second of two parts). N Engl J Med. 1975;292(17):895–902. https://doi.org/10.1056/nejm197504242921706.
Shulman HM, Sullivan KM, Weiden PL, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 seattle patients. Am J Med. 1980;69(2):204–17. https://doi.org/10.1016/0002-9343(80)90380-0.
Wang Y, Liu DH, Xu LP, et al. Superior graft-versus-leukemia effect associated with transplantation of haploidentical compared with hla-identical sibling donor grafts for high-risk acute leukemia: An historic comparison. Biol Blood Marrow Transplant. 2011;17(6):821–30. https://doi.org/10.1016/j.bbmt.2010.08.023.
Scott BL, Pasquini MC, Fei M, et al. Myeloablative versus reduced-intensity conditioning for hematopoietic cell transplantation in acute myelogenous leukemia and myelodysplastic syndromes-long-term follow-up of the bmt ctn 0901 clinical trial. Transplant Cell Ther. 2021;27(6):483.e1-.e6. https://doi.org/10.1016/j.jtct.2021.02.031.
Tang FF, Sun YQ, Mo XD, et al. Incidence, risk factors, and outcomes of primary prolonged isolated thrombocytopenia after haploidentical hematopoietic stem cell transplant. Biol Blood Marrow Transplant. 2020;26(8):1452–8. https://doi.org/10.1016/j.bbmt.2020.03.024.
Funding
This study was supported by the National Key Research and Development Program of China (No. 2022YFA1103300), Major Program of the National Natural Science Foundation of China (No. 82293630), the Key Program of the National Natural Science Foundation of China (No. 81930004), and the National Key Research and Development Program of China (No. 2021YFC2500302).
Author information
Authors and Affiliations
Contributions
XH and FT contributed to the study conception and design; YW, JJ, WH, YC, CY, LX, and XZ provided the clinical data; FT and YW performed the data analysis and interpretation; manuscript was written by FT and YW, and XH supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This study was performed in accordance with the Declaration of Helsinki, and the protocol was approved by the ethics committee of Peking University People's Hospital.
Consent to participate
Informed consent was obtained from all patients for being included in the study.
Consent for publication
The authors affirm that human study participants provided informed consent to publish.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, F., Wang, Y., Wang, Y. et al. The clinical outcomes of haploidentical stem cell transplantation (haplo-HSCT) for patients with therapy-related myelodysplastic syndrome: comparable to de novo myelodysplastic syndrome. Clin Exp Med 24, 33 (2024). https://doi.org/10.1007/s10238-023-01287-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10238-023-01287-8