Abstract
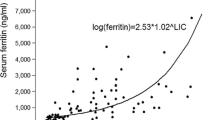
We evaluated pattern and clinical correlates of renal T2* measurements in adult β-thalassemia major (β-TM) patients. Ninety β-TM patients (48 females, 38.15 ± 7.94 years), consecutively enrolled in the Extension-Myocardial Iron Overload in Thalassemia network, underwent T2* magnetic resonance imaging (MRI) for quantification of iron overload (IO) in kidneys, liver, pancreas, and heart. Ten (11.1%) patients showed renal IO (T2* < 31 ms). Global kidney T2* values did not show a correlation with gender, age, splenectomy, regular transfusions or chelation starting age, pre-transfusion hemoglobin, and serum ferritin levels. Global kidney T2* values showed an inverse correlation with MRI liver iron concentration (LIC) values (R = − 0.349; p = 0.001) and a positive correlation with global pancreas T2* values (R = 0.212; p = 0.045). Frequency of renal IO was significantly higher in patients with cardiac IO than in patients without cardiac IO (50.0% vs. 6.3%; p = 0.001). A significant inverse association was detected between global kidneys T2* values and lactate dehydrogenase (LDH) (R = − 0.529; p < 0.0001). In multivariate regression analysis, MRI LIC and LDH were the strongest predictors of global kidney T2* values. A MRI LIC > 4.83 mg/g dw predicted the presence of renal IO (sensitivity = 90.0%; specificity = 61.2%). Global kidney T2* values were inversely correlated with uric acid (R = − 0.269; p = 0.025). In conclusion, in adult β-TM patients, renal iron deposition is not common and is linked to both hemolysis and total body iron overload.

Similar content being viewed by others
References
Cao A, Galanello R. Beta-thalassemia. Genet Med. 2010;12(2):61–76.
Olivieri NF. The beta-thalassemias. N Engl J Med. 1999;341(2):99–109.
Andrews PA. Disorders of iron metabolism. N Engl J Med. 2000;342(17):1293.
Ozment CP, Turi JL. Iron overload following red blood cell transfusion and its impact on disease severity. Biochim Biophys Acta. 2009;1790(7):694–701.
Hentze MW, Muckenthaler MU, Andrews NC. Balancing acts: molecular control of mammalian iron metabolism. Cell. 2004;117(3):285–97.
Borgna-Pignatti C, Rugolotto S, De Stefano P, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89(10):1187–93.
Modell B, Khan M, Darlison M, Westwood MA, Ingram D, Pennell DJ. Improved survival of thalassaemia major in the UK and relation to T2* cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2008;10(1):42.
Pepe A, Pistoia L, Gamberini MR, et al. National networking in rare diseases and reduction of cardiac burden in thalassemia major. Eur Heart J. 2022;43(26):2482–92.
Demosthenous C, Vlachaki E, Apostolou C, et al. Beta-thalassemia: renal complications and mechanisms: a narrative review. Hematology. 2019;24(1):426–38.
Sumboonnanonda A, Malasit P, Tanphaichitr VS, et al. Renal tubular function in beta-thalassemia. Pediatr Nephrol. 1998;12(4):280–3.
Sadeghi-Bojd S, Hashemi M, Karimi M. Renal tubular function in patients with beta-thalassaemia major in Zahedan, southeast Iran. Singapore Med J. 2008;49(5):410–2.
Koliakos G, Papachristou F, Koussi A, et al. Urine biochemical markers of early renal dysfunction are associated with iron overload in beta-thalassaemia. Clin Lab Haematol. 2003;25(2):105–9.
Zhou XJ, Laszik Z, Wang XQ, Silva FG, Vaziri ND. Association of renal injury with increased oxygen free radical activity and altered nitric oxide metabolism in chronic experimental hemosiderosis. Lab Invest. 2000;80(12):1905–14.
Anderson LJ, Holden S, Davis B, et al. Cardiovascular T2-star (T2*) magnetic resonance for the early diagnosis of myocardial iron overload. Eur Heart J. 2001;22(23):2171–9.
Meloni A, Positano V, Pepe A, et al. Preferential patterns of myocardial iron overload by multislice multiecho T*2 CMR in thalassemia major patients. Magn Reson Med. 2010;64(1):211–9.
Wood JC. Magnetic resonance imaging measurement of iron overload. Curr Opin Hematol. 2007;14(3):183–90.
Pepe A, Pistoia L, Gamberini MR, et al. The close link of pancreatic iron with glucose metabolism and with cardiac complications in thalassemia major: a large. Multicenter Observat Study Diabetes Care. 2020;43(11):2830–9.
Schein A, Enriquez C, Coates TD, Wood JC. Magnetic resonance detection of kidney iron deposition in sickle cell disease: a marker of chronic hemolysis. J Magn Reson Imaging. 2008;28(3):698–704.
Hashemieh M, Azarkeivan A, Akhlaghpoor S, Shirkavand A, Sheibani K. T2-star (T2*) magnetic resonance imaging for assessment of kidney iron overload in thalassemic patients. Arch Iran Med. 2012;15(2):91–4.
ElAlfy MS, Khalil Elsherif NH, Ebeid FSE, et al. Renal iron deposition by magnetic resonance imaging in pediatric beta-thalassemia major patients: relation to renal biomarkers, total body iron and chelation therapy. Eur J Radiol. 2018;103:65–70.
Pepe A, Positano V, Santarelli F, et al. Multislice multiecho T2* cardiovascular magnetic resonance for detection of the heterogeneous distribution of myocardial iron overload. J Magn Reson Imaging. 2006;23(5):662–8.
Ramazzotti A, Pepe A, Positano V, et al. Multicenter validation of the magnetic resonance t2* technique for segmental and global quantification of myocardial iron. J Magn Reson Imaging. 2009;30(1):62–8.
Meloni A, De Marchi D, Pistoia L, et al. Multicenter validation of the magnetic resonance T2* technique for quantification of pancreatic iron. Eur Radiol. 2019;29(5):2246–52.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med. 1999;130(6):461–70.
Grassedonio E, Meloni A, Positano V, et al. Quantitative T2* magnetic resonance imaging for renal iron overload assessment: normal values by age and sex. Abdom Imaging. 2015;40:1700–4.
Restaino G, Meloni A, Positano V, et al. Regional and global pancreatic T*(2) MRI for iron overload assessment in a large cohort of healthy subjects: normal values and correlation with age and gender. Magn Reson Med. 2011;65(3):764–9.
Positano V, Salani B, Pepe A, et al. Improved T2* assessment in liver iron overload by magnetic resonance imaging. Magn Reson Imaging. 2009;27(2):188–97.
Positano V, Pepe A, Santarelli MF, et al. Standardized T2* map of normal human heart in vivo to correct T2* segmental artefacts. NMR Biomed. 2007;20(6):578–90.
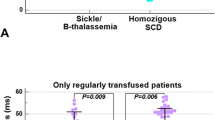
Meloni A, Barbuto L, Pistoia L, et al. Frequency, pattern, and associations of renal iron accumulation in sickle/beta-thalassemia patients. Ann Hematol. 2022;101(9):1941–50.
Meloni A, Luciani A, Positano V, et al. Single region of interest versus multislice T2* MRI approach for the quantification of hepatic iron overload. J Magn Reson Imaging. 2011;33(2):348–55.
Wood JC, Enriquez C, Ghugre N, et al. MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood. 2005;106(4):1460–5.
Meloni A, Rienhoff HY Jr, Jones A, Pepe A, Lombardi M, Wood JC. The use of appropriate calibration curves corrects for systematic differences in liver R2* values measured using different software packages. Br J Haematol. 2013;161(6):888–91.
Angelucci E, Brittenham GM, McLaren CE, et al. Hepatic iron concentration and total body iron stores in thalassemia major. N Engl J Med. 2000;343(5):327–31.
Meloni A, De Marchi D, Positano V, et al. Accurate estimate of pancreatic T2* values: how to deal with fat infiltration. Abdom Imaging. 2015;40(8):3129–36.
Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002;105(4):539–42.
Meloni A, Maggio A, Positano V, et al. CMR for myocardial iron overload quantification: calibration curve from the MIOT network. Eur Radiol. 2020;29(5):2246–52.
Taher A, Elalfy MS, Al Zir K, et al. Importance of optimal dosing >/= 30 mg/kg/d during deferasirox treatment: 2.7-yr follow-up from the ESCALATOR study in patients with beta-thalassaemia. Eur J Haematol. 2011;87(4):355–65.
Casale M, Marsella M, Ammirabile M, et al. Predicting factors for liver iron overload at the first magnetic resonance in children with thalassaemia major. Blood Transfus. 2018;2018:1–6.
Noetzli LJ, Papudesi J, Coates TD, Wood JC. Pancreatic iron loading predicts cardiac iron loading in thalassemia major. Blood. 2009;114(19):4021–6.
Gladwin MT, Kanias T, Kim-Shapiro DB. Hemolysis and cell-free hemoglobin drive an intrinsic mechanism for human disease. J Clin Investig. 2012;122(4):1205–8.
Kristiansen M, Graversen JH, Jacobsen C, et al. Identification of the haemoglobin scavenger receptor. Nature. 2001;409(6817):198–201.
Gburek J, Verroust PJ, Willnow TE, et al. Megalin and cubilin are endocytic receptors involved in renal clearance of hemoglobin. J Am Soc Nephrol. 2002;13(2):423–30.
Kovtunovych G, Eckhaus MA, Ghosh MC, Ollivierre-Wilson H, Rouault TA. Dysfunction of the heme recycling system in heme oxygenase 1-deficient mice: effects on macrophage viability and tissue iron distribution. Blood. 2010;116(26):6054–62.
Waikar SS, Betensky RA, Emerson SC, Bonventre JV. Imperfect gold standards for kidney injury biomarker evaluation. J Am Soc Nephrol. 2012;23(1):13–21.
Grangé S, Bertrand DM, Guerrot D, Eas F, Godin M. Acute renal failure and Fanconi syndrome due to deferasirox. Nephrol Dial Transpl. 2010;25(7):2376–8.
Behairy OG, Abd Almonaem ER, Abed NT, et al. Role of serum cystatin-C and beta-2 microglobulin as early markers of renal dysfunction in children with beta thalassemia major. Int J Nephrol Renovasc Dis. 2017;10:261–8.
Giordano C, Karasik O, King-Morris K, Asmar A. Uric acid as a marker of kidney disease: review of the current literature. Dis Markers. 2015;2015: 382918.
Acknowledgements
We would like to thank all the colleagues involved in the E-MIOT project (https://emiot.ftgm.it/) and all patients for their cooperation. This work is generated within the European Reference Network on Rare Hematological Diseases (ERN-EuroBloodNet).
Funding
The E-MIOT project received “no-profit support” from industrial sponsorships (Chiesi Farmaceutici S.p.A. and Bayer). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
AM conceived the study, analyzed the data, interpreted the results, and wrote the paper. LB analyzed the renal T2* images. VP developed the software for image analysis. LP was responsible for data collection. AS, TC, FM, CA, PG, and AB collected the data. LR contributed to the interpretation of the results. FC supervised the study. All authors contributed to critical revision of the manuscript and read and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Ethics Committee of Area Vasta Nord Ovest (protocol code 56664, date of approval October 8, 2015).
Consent to participate
Informed consent was obtained from all patients included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meloni, A., Barbuto, L., Positano, V. et al. Pattern and clinical correlates of renal iron deposition in adult beta-thalassemia major patients. Clin Exp Med 23, 3573–3579 (2023). https://doi.org/10.1007/s10238-023-01133-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01133-x