Abstract
Background and aims
Sarcopenia is an important prognostic factor for cancer patients. The aim of this study was to assess the ability of sarcopenia to predict recurrent biliary obstruction (RBO) in patients with unresectable cancer after EUS-guided biliary drainage (EUS-BD).
Methods
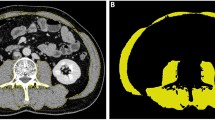
The study enrolled 113 patients who underwent EUS-BD using the self-expandable metal stent (SEMS) for unresectable malignant biliary obstruction (MBO) between April 2016 and December 2021 at Wakayama Medical University Hospital. The skeletal muscle index at the third lumbar spine level (L3) was calculated from computed tomography images. We analyzed the cumulative incidence of RBO at 180 days after stent insertion. Univariate and multivariate analyses were performed to identify variables significantly associated with RBO.
Results
Seventy-six patients were assigned to the sarcopenia group, and 37 were assigned to the non-sarcopenia group. The 180-day cumulative incidence of RBO was 11% in the non-sarcopenia group and 29% in the sarcopenia group (p = 0.034). The time to RBO was significantly shorter for the sarcopenia group (p = 0.028; Gray’s test). Multivariate analyses identified sarcopenia as an independent prognostic factor for RBO (present vs absent; HR 4.61; 95% CI 1.76–12.10, p = 0.001). The rates of biliary sludge/food impaction were significantly higher in the sarcopenia group for the causes of RBO (p = 0.048). There were no significant differences between the sarcopenia and the non-sarcopenia groups with respect to related EUS-BD adverse events.
Conclusion
Sarcopenia is an independent indicator of RBO in patients with MBO who receive EUS-BD with SEMS.



Similar content being viewed by others
References
Rosenberg IH (1997) Sarcopenia: origins and clinical relevance. J Nutr 127:990s–991s
Delmonico MJ, Harris TB, Lee JS et al (2007) Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 55:769–774
Goodpaster BH, Park SW, Harris TB et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:601
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing 39:412–423
Rollins KE, Tewari N, Ackner A et al (2016) The impact of sarcopenia and myosteatosis on outcomes of unresectable pancreatic cancer or distal cholangiocarcinoma. Clin Nutr 35:1103–1109
Henderson SE, Makhijani N, Mace TA (2018) Pancreatic cancer-induced cachexia and relevant mouse models. Pancreas 47:937–945
Tan BH, Birdsell LA, Martin L et al (2009) Sarcopenia in an overweight or obese patient is an adverse prognostic factor in pancreatic cancer. Clin Cancer Res 15:6973–6979
Okumura S, Kaido T, Hamaguchi Y et al (2016) Impact of the preoperative quantity and quality of skeletal muscle on outcomes after resection of extrahepatic biliary malignancies. Surgery 159:821–833
Choi Y, Oh DY, Kim TY et al (2015) Skeletal muscle depletion predicts the prognosis of patients with advanced pancreatic cancer undergoing palliative chemotherapy, independent of body mass index. PLoS ONE 10:e0139749
Emori T, Itonaga M, Ashida R et al (2022) Impact of sarcopenia on prediction of progression-free survival and overall survival of patients with pancreatic ductal adenocarcinoma receiving first-line gemcitabine and nab-paclitaxel chemotherapy. Pancreatology 22:277–285
Rizvi S, Gores GJ (2013) Pathogenesis, diagnosis, and management of cholangiocarcinoma. Gastroenterology 145:1215–1229
Almadi MA, Barkun A, Martel M (2017) Plastic vs. self-expandable metal stents for palliation in malignant biliary obstruction: a series of meta-analyses. Am J Gastroenterol 112:260–273
Nakai Y, Isayama H, Wang HP et al (2020) International consensus statements for endoscopic management of distal biliary stricture. J Gastroenterol Hepatol 35:967–979
Isayama H, Nakai Y, Itoi T et al (2019) Clinical practice guidelines for safe performance of endoscopic ultrasound/ultrasonography-guided biliary drainage: 2018. J Hepatobiliary Pancreat Sci 26:249–269
Kawakubo K, Isayama H, Kato H et al (2014) Multicenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in Japan. J Hepatobiliary Pancreat Sci 21:328–334
Paik WH, Lee TH, Park DH et al (2018) EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: a multicenter randomized clinical trial. Am J Gastroenterol 113:987–997
Nakai Y, Isayama H, Kawakami H et al (2019) Prospective multicenter study of primary EUS-guided choledochoduodenostomy using a covered metal stent. Endosc Ultrasound 8:111–117
Park JK, Woo YS, Noh DH et al (2018) Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: prospective randomized controlled study. Gastrointest Endosc 88:277–282
Von Hoff DD, Ervin T, Arena FP et al (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369:1691–1703
Valle J, Wasan H, Palmer DH et al (2010) Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med 362:1273–1281
Mitsiopoulos N, Baumgartner RN, Heymsfield SB et al (1985) Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol 1998(85):115–122
Heymsfield SB, Wang Z, Baumgartner RN et al (1997) Human body composition: advances in models and methods. Annu Rev Nutr 17:527–558
Prado CM, Baracos VE, McCargar LJ et al (2009) Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res 15:2920–2926
Sato H, Goto T, Hayashi A et al (2021) Prognostic significance of skeletal muscle decrease in unresectable pancreatic cancer: survival analysis using the Weibull exponential distribution model. Pancreatology 21:892–902
Kashihara H, Lee JS, Kawakubo K et al (2009) Criteria of waist circumference according to computed tomography-measured visceral fat area and the clustering of cardiovascular risk factors. Circ J 73:1881–1886
Smith RA, Bosonnet L, Raraty M et al (2009) Preoperative platelet–lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg 197:466–472
Bhatti I, Peacock O, Lloyd G et al (2010) Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil–lymphocyte versus platelet–lymphocyte ratio. Am J Surg 200:197–203
Proctor MJ, Morrison DS, Talwar D et al (2011) A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow inflammation outcome study. Eur J Cancer 47:2633–2641
Stotz M, Gerger A, Eisner F et al (2013) Increased neutrophil-lymphocyte ratio is a poor prognostic factor in patients with primary operable and inoperable pancreatic cancer. Br J Cancer 109:416–421
Szkandera J, Stotz M, Absenger G et al (2014) Validation of C-reactive protein levels as a prognostic indicator for survival in a large cohort of pancreatic cancer patients. Br J Cancer 110:183–188
Piciucchi M, Stigliano S, Archibugi L et al (2017) The neutrophil/lymphocyte ratio at diagnosis is significantly associated with survival in metastatic pancreatic cancer patients. Int J Mol Sci 18:730
Ikeguchi M, Goto K, Watanabe J et al (2019) Clinical importance of preoperative and postoperative prognostic nutritional index in patients with pancreatic ductal adenocarcinoma. Ann Hepatobiliary Pancreat Surg 23:372–376
Liu Z, Jin K, Guo M et al (2017) Prognostic value of the CRP/Alb ratio, a novel inflammation-based score in pancreatic cancer. Ann Surg Oncol 24:561–568
Austin PC, Fine JP (2017) Accounting for competing risks in randomized controlled trials: a review and recommendations for improvement. Stat Med 36:1203–1209
Ishiwatari H, Ishikawa K, Niiya F et al (2022) Endoscopic ultrasound-guided hepaticogastrostomy versus hepaticogastrostomy with antegrade stenting for malignant distal biliary obstruction. J Hepatobiliary Pancreat Sci 29:703–712
Ogura T, Chiba Y, Masuda D et al (2016) Comparison of the clinical impact of endoscopic ultrasound-guided choledochoduodenostomy and hepaticogastrostomy for bile duct obstruction with duodenal obstruction. Endoscopy 48:156–163
Koya Y, Shibata M, Oe S et al (2021) Impact of sarcopenia on recurrent biliary obstruction after insertion of self-expandable metallic stent in patients with malignant biliary obstruction. J Hepatobiliary Pancreat Sci 28:572–580
Leitzmann MF, Giovannucci EL, Rimm EB et al (1998) The relation of physical activity to risk for symptomatic gallstone disease in men. Ann Intern Med 128:417–425
Serra-Prat M, Mans E, Palomera E et al (2013) Gastrointestinal peptides, gastrointestinal motility, and anorexia of aging in frail elderly persons. Neurogastroenterol Motil 25:291-e245
Shintakuya R, Sasaki M, Nakamitsu A et al (2019) Sarcopenia is an independent predictor of delayed gastric emptying following pancreaticoduodenectomy: a retrospective study. ANZ J Surg. https://doi.org/10.1111/ans.15379
Tsukagoshi M, Harimoto N, Araki K et al (2021) Impact of preoperative nutritional support and rehabilitation therapy in patients undergoing pancreaticoduodenectomy. Int J Clin Oncol 26(9):1698–1706
Kitahata Y, Hirono S, Kawai M et al (2018) Intensive perioperative rehabilitation improves surgical outcomes after pancreaticoduodenectomy. Langenbecks Arch Surg 403:711–718
Luo H, Galvão DA, Newton RU et al (2021) Exercise medicine in the management of pancreatic cancer: a systematic review. Pancreas 50:280–292
Hamauchi S, Furuse J, Takano T et al (2019) A multicenter, open-label, single-arm study of anamorelin (ONO-7643) in advanced gastrointestinal cancer patients with cancer cachexia. Cancer 125:4294–4302
Funding
This study was supported by Olympus.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.K. has received honoraria from Olympus Corporation for spoken lectures at conferences. The other authors declare that they have no conflict of interest regarding the publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary figure 1.
Cumulative survival probability between groups with and without RBO in each group. (A) Overall survival (calculated using the Kaplan–Meier method) in the sarcopenia group between without RBO (solid line) and with RBO (dotted line). Supplementary file1 (TIF 24930 KB)
About this article
Cite this article
Emori, T., Itonaga, M., Ashida, R. et al. Impact of sarcopenia on recurrent biliary obstruction after EUS-guided biliary drainage in patients with malignant biliary obstruction. Int J Clin Oncol 29, 286–296 (2024). https://doi.org/10.1007/s10147-023-02455-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-023-02455-2