Abstract
Background
The effects of the type of anesthesia (spinal (SA) vs. general (GA)) used for transurethral resection of bladder tumor (TURBT) on non-muscle invasive bladder cancer (NMIBC) recurrence and progression are controversial and our aim is to investigate their associations.
Methods
We identified 300 NMIBC patients who underwent initial TURBT with SA or GA. Cox’s regression analysis was performed to examine the effects of anesthesia on tumor recurrence.
Results
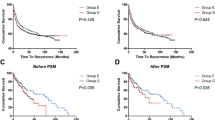
Among 300 patients, 153 (51.0%) received GA and 147 (49.0%) SA. The 5-year recurrence-free survival (RFS) rate was 59.9% in the GA group, which was significantly lower than that in the SA group (74.4%, p = 0.029). GA (HR 1.57, p = 0.048), male sex (HR 2.72, p = 0.012), and tumor multiplicity (HR 1.96, p = 0.006) were independently associated with tumor recurrence. In a subgroup of 137 patients with high-risk NMIBC, the 5-year RFS rate was 50.3% in the GA group, which was significantly lower than that in the SA group (77.6%, p = 0.020), and GA remained an independent indicator of tumor recurrence (HR 2.35, p = 0.016). However, no significant differences were observed in the RFS rates of low- to intermediate-risk NMIBC patients between the GA and SA groups.
Conclusions
The RFS rate was lower in NMIBC patients who received GA during TURBT than in those who received SA. Volatile anesthesia may increase tumor recurrence, particularly in high-risk NMIBC patients, which may be due to the inhibition of the immune response system during surgery.


Similar content being viewed by others
References
Dobruch J, Daneshmand S, Fisch M et al (2016) Gender and bladder cancer: a collaborative review of etiology, biology, and outcomes. Eur Urol 69(2):300–310. https://doi.org/10.1016/j.eururo.2015.08.037
Kamat AM, Hahn NM, Efstathiou JA et al (2016) Bladder cancer. Lancet 388(10061):2796–2810. https://doi.org/10.1016/S0140-6736(16)30512-8
Sylvester RJ, van der Adrian Meijden PM , Lamm DL (2002) Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol 168(5):1964–1970. https://doi.org/10.1097/01.ju.0000034450.80198.1c
Sun Y, Li T, Gan TJ (2015) The effects of perioperative regional anesthesia and analgesia on cancer recurrence and survival after oncology surgery: a systematic review and meta-analysis. Reg Anesth Pain Med 40(5):589–598. https://doi.org/10.1097/AAP.0000000000000273
Iwasaki M, Zhao H, Jaffer T et al (2016) Volatile anaesthetics enhance the metastasis related cellular signalling including CXCR2 of ovarian cancer cells. Oncotarget 7(18):26042–26056. https://doi.org/10.18632/oncotarget.8304
Tai LH, de Souza CT, Belanger S et al (2013) Preventing postoperative metastatic disease by inhibiting surgery-induced dysfunction in natural killer cells. Cancer Res 73(1):97–107. https://doi.org/10.1158/0008-5472.CAN-12-1993
Koumpan Y, Jaeger M, Mizubuti GB et al (2018) Spinal anesthesia is associated with lower recurrence rates after resection of non-muscle invasive bladder cancer. J Urol 199(4):940–946. https://doi.org/10.1016/j.juro.2017.11.064
Soukup V, Capoun O, Cohen D et al (2017) Prognostic performance and reproducibility of the 1973 and 2004/2016 world health organization grading classification systems in non-muscle-invasive bladder cancer: a European Association of Urology non-muscle invasive bladder cancer guidelines panel systematic review. Eur Urol 72(5):801–813. https://doi.org/10.1016/j.eururo.2017.04.015
Babjuk M, Bohle A, Burger M et al (2017) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol 71(3):447–461. https://doi.org/10.1016/j.eururo.2016.05.041
Abdallah FW, Wijeysundera DN (2019) Anaesthetic interventions and long-term tumour recurrence. Lancet 394(10211):1781–1782. https://doi.org/10.1016/s0140-6736(19)32314-1
Scavonetto F, Yeoh TY, Umbreit EC et al (2014) Association between neuraxial analgesia, cancer progression, and mortality after radical prostatectomy: a large, retrospective matched cohort study. Br J Anaesth 113(Suppl 1):i95-102. https://doi.org/10.1093/bja/aet467
Christopherson R, James KE, Tableman M et al (2008) Long-term survival after colon cancer surgery: a variation associated with choice of anesthesia. Anesth Analg 107(1):325–332. https://doi.org/10.1213/ane.0b013e3181770f55
Sessler DI, Pei L, Huang Y et al (2019) Recurrence of breast cancer after regional or general anaesthesia: a randomised controlled trial. Lancet 394(10211):1807–1815. https://doi.org/10.1016/s0140-6736(19)32313-x
Kim R (2018) Effects of surgery and anesthetic choice on immunosuppression and cancer recurrence. J Transl Med 16(1):8. https://doi.org/10.1186/s12967-018-1389-7
Zhao H, Iwasaki M, Yang J et al (2014) Hypoxia-inducible factor-1: a possible link between inhalational anesthetics and tumor progression? Acta Anaesthesiol Taiwan 52(2):70–76. https://doi.org/10.1016/j.aat.2014.05.008
Surhonne N, Hebri C, Kannan S et al (2019) The effect of anesthetic techniques on neutrophil to lymphocyte ratio in patients undergoing infraumbilical surgeries. Korean J Anesthesiol 72(5):458–465. https://doi.org/10.4097/kja.d.19.00022
Ni Eochagain A, Burns D, Riedel B et al (2018) The effect of anaesthetic technique during primary breast cancer surgery on neutrophil-lymphocyte ratio, platelet-lymphocyte ratio and return to intended oncological therapy. Anaesthesia 73(5):603–611. https://doi.org/10.1111/anae.14207
Bar-Yosef S, Melamed R, Page GG et al (2001) Attenuation of the tumor-promoting effect of surgery by spinal blockade in rats. Anesthesiology 94(6):1066–1073. https://doi.org/10.1097/00000542-200106000-00022
Tonnesen E, Wahlgreen C (1988) Influence of extradural and general anaesthesia on natural killer cell activity and lymphocyte subpopulations in patients undergoing hysterectomy. Br J Anaesth 60(5):500–507. https://doi.org/10.1093/bja/60.5.500
Kweon TD, Lee KY (2018) Spinal anesthesia is associated with lower recurrence rates after resection of non-muscle invasive bladder cancer. Transl Androl Urol 7(2):283–286. https://doi.org/10.21037/tau.2018.03.13
Miyake M, Iida K, Nishimura N, Japanese Urological Oncology G et al (2021) Non-maintenance intravesical Bacillus Calmette-Guerin induction therapy with eight doses in patients with high- or highest-risk non-muscle invasive bladder cancer: a retrospective non-randomized comparative study. BMC Cancer 21(1):266. https://doi.org/10.1186/s12885-021-07966-7
Acknowledgements
We are grateful to Medical English Service (https://www.med-english.com/) for the English language review.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology YB, EK, KS. Formal analysis and investigation, original draft preparation YB, YN, YM. Review and editing EK, KS. Resources KO, MM, YN, YM. Supervision HA, MO, RM, MO.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The institutional review board in each facility regarding this study has approved the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Baba, Y., Kikuchi, E., Shigeta, K. et al. Effects of transurethral resection under general anesthesia on tumor recurrence in non-muscle invasive bladder cancer. Int J Clin Oncol 26, 2094–2103 (2021). https://doi.org/10.1007/s10147-021-02000-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-021-02000-z