Abstract
Background
Point of Care Ultrasound (PoCUS) is a safe, non-invasive tool for identifying distal radius fractures and can potentially be utilised to assist clinicians to reduce displaced fractures. We aim to test whether PoCUS is accurate to identify distal radius fractures and to determine how PoCUS performs as a tool to confirm a successful fracture reduction.
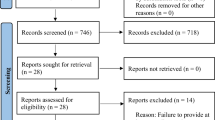
Methods
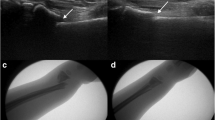
A pragmatic prospective observational study was done in adult patients presenting with forearm injuries resulting in Colle’s type distal radius fractures. Adults who presented to the emergency department (ED) with a suspected distal forearm fracture from August 2018 to July 2019 were conveniently sampled for inclusion into the study when a trained ED ultra-sonographer was available. PoCUS scans over the point of maximal tenderness were done using a high frequency linear transducer (7.5–10 mHz) prior to X-ray. Patients who required a manipulation of the fracture had a second ultrasound scan immediately after the procedure before the second X-ray was ordered. PoCUS scans were compared to X-rays for accuracy in both groups.
Results
Fractures were identified in 44 out of 47 included patients using both PoCUS and X-ray modalities. This showed a sensitivity of 100% (95% CI: 90–100%) and specificity of 100% (95% CI: 31–100%). Fracture manipulation was required in 35 out of 44 patients. The sensitivity and specificity of PoCUS in determining alignment accuracy when compared to X-ray were 100% (95% CI: 83–100%) and 64% (95% CI: 32–88%) respectively. The PPV and NPV were 86% (95% CI: 66–95%) and 100% (95% CI: 56–100%) respectively. Ten out of 44 (23%) patients with distal radius fractures ultimately required an Open Reduction and Internal Fixation (ORIF).
Conclusion
Our study supports the use of PoCUS for identifying distal radius forearm fractures and may have some value in assisting clinicians to determine post reduction success. We still advocate using standard X-ray radiographs to confirm successful or adequate cortical alignment following a manipulation.



Similar content being viewed by others
Change history
21 July 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10140-021-01970-x
References
Nijs S, Broos PL (2004) Fractures of the distal radius: a contemporary approach. Acta Chir Belg 104(4):401–412
Kozaci N, Ay MO, Akcimen M, Turhan G, Sasmaz I, Turhan S et al (2015) Evaluation of the effectiveness of bedside point-of-care ultrasound in the diagnosis and management of distal radius fractures. Am J Emerg Med 33(1):67–71
Kodama N, Takemura Y, Ueba H, Imai S, Matsusue Y (2014) Ultrasound-assisted closed reduction of distal radius fractures. J Hand Surg Am 39(7):1287–1294
Bong MR, Egol KA, Leibman M, Koval KJ (2006) A comparison of immediate postreduction splinting constructs for controlling initial displacement of fractures of the distal radius: a prospective randomized study of long-arm versus short-arm splinting. J Hand Surg Am 31(5):766–770
Földhazy Z, Törnkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L (2007) Long-term outcome of nonsurgically treated distal radius fractures. J Hand Surg Am 32(9):1374–1384
Earnshaw SA, Aladin A, Surendran S, Moran CG (2002) Closed reduction of colles fractures: comparison of manual manipulation and finger-trap traction: a prospective, randomized study. J Bone Joint Surg Am 84-A(3):354–8
Puchalski P, Zyluk A (2005) Complex regional pain syndrome type 1 after fractures of the distal radius: a prospective study of the role of psychological factors. J Hand Surg Br 30(6):574–580
Chartier LB, Bosco L, Lapointe-Shaw L, Chenkin J (2017) Use of point-of-care ultrasound in long bone fractures: a systematic review and meta-analysis. CJEM 19(2):131–142
Rowlands R, Rippey J, Tie S, Flynn J (2017) Bedside ultrasound vs X-ray for the diagnosis of forearm fractures in children. J Emerg Med 52(2):208–215
Douma-den Hamer D, Blanker M, Edens M, Buijteweg L, Boomsma M, Van Helden S, Mauritz G (2016) Ultrasound for distal forearm fracture: a systematic review and diagnostic meta-analysis. PLOS One 1–16 https://doi.org/10.1371/journal.pone.0155659
Champagne N, Eadie L, Regan L, Wilson P (2019) The effectiveness of ultrasound in the detection of fractures in adults with suspected upper or lower limb injury: a systematic review and subgroup meta-analysis. BMC Emerg Med 19(17):1–15. https://doi.org/10.1186/s12873-019-0226-5
Chinnock B, Khaletskiy A, Kuo K, Hendey GW (2011) Ultrasound-guided reduction of distal radius fractures. J Emerg Med 40(3):308–312
Sivrikaya S, Aksay E, Bayram B, Oray NC, Karakasli A, Altintas E (2016) Emergency physicians performed Point-of-Care-Ultrasonography for detecting distal forearm fracture. Turk J Emerg Med 16(3):98–101
Dubrovsky AS, Kempinska A, Bank I (2015) Accuracy of ultrasonography for determining successful realignment of paediatric forearm fractures. Ann Emerge Med 65(3):260–265
Socransky S, Skinner A, Bromley M et al (2016) Ultrasound-assisted distal radius fracture reduction. Cureus 8(7):e674. https://doi.org/10.7759/cureus.674
Sengab A, Krijnen P, Schipper IB (2019) Risk factors for fracture redisplacement after reduction and cast immobilization of displaced distal radius fractures in children: a meta-analysis [published online ahead of print, 2019 Sep 9]. Eur J Trauma Emerg Surg https://doi.org/10.1007/s00068-019-01227-w
Jordan RW, Jaddon S, Srinivas K, Shyamalan G (2016) The Value of maniopulation of displaced distal radius fractures in the emergency department. Acta Orthop Belg 82(2):203–209
Cobb AG, Houghton GR (1985) Local anaesthetic infiltration versus Bier’s block for Colles’ fractures. Br Med J (Clin Res Ed) 291:1683–1684
Siebelt M, Hartholt KA, van Winden DFM et al (2019) Ultrasound-guided nerve blocks as analgesia for nonoperative management of distal radius fractures-two consecutive randomized controlled trials. J Orthop Trauma 33:e124–e130. https://doi.org/10.1097/BOT.0000000000001388
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original article contains a spelling error in Author name. Instead of “Wickremarachchi” it should be “Wickramarachchi”.
Rights and permissions
About this article
Cite this article
Wood, D., Reddy, M., Postma, I. et al. Ultrasound in forearm fractures: a pragmatic study assessing the utility of Point of Care Ultrasound (PoCUS) in identifying and managing distal radius fractures. Emerg Radiol 28, 1107–1112 (2021). https://doi.org/10.1007/s10140-021-01957-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-021-01957-8