Abstract
Objectives
Systemic lupus erythematosus (SLE) and the Epstein-Barr virus (EBV) are very closely related. This study estimated the impact of EBV infection status on clinical manifestations and disease remission in patients with SLE.
Method
A retrospective study was performed using electronic health records of patients with SLE. The SLE disease activity index (SLEDAI-2 K) was used to assess disease activity. VCAIgM or EAIgM positive or EBVDNA copies ≥ 50 IU/mL were defined as lytic infection group, EBNA-IgG or VCAIgG-positive and who were negative for both VCAIgM and EAIgM with EBVDNA copies < 50 IU/mL were defined as the latent infection group. The endpoint (disease remission) was defined as a decrease in SLEDAI-2 K score of ≥ 1 grade or ≥ 4 points from baseline. The association between EBV infection status and disease remission was assessed using propensity score weighting and multivariable Cox regression models.
Results
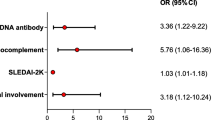
There were 75 patients with SLE in the EBV lytic infection group and 142 patients in the latent infection group. The SLEDAI-2 K score was higher in the lytic infection group (10.00 (6.25, 16.00) vs. 8.00 (5.00, 10.00), Z = 3.96, P < 0.001). There was a significant difference in the effect of EBV lytic infection on disease remission compared to latent infection (HR 0.30, 95% CI 0.19–0.49, P < 0.001).
Conclusions
Patients with SLE with lytic EBV infection have higher disease activity and take longer to achieve remission. Our study furthers our understanding of the relationship between SLE and EBV infection and may inform better treatment practices in the future.


Similar content being viewed by others
References
Lazar S, Kahlenberg JM (2023) Systemic lupus erythematosus: new diagnostic and therapeutic approaches. Annu Rev Med 74:339–352. https://doi.org/10.1146/annurev-med-043021-032611
Rees F, Doherty M, Grainge MJ, Lanyon P, Davenport G, Zhang W (2016) Mortality in systemic lupus erythematosus in the United Kingdom 1999–2012. Rheumatology 55:854–860. https://doi.org/10.1093/rheumatology/kev424
Iwata S, Tanaka Y (2022) Association of viral infection with the development and pathogenesis of systemic lupus erythematosus. Front Med (Lausanne) 25(9):849120. https://doi.org/10.3389/fmed.2022.849120
Jog NR, James JA (2021Feb) Epstein Barr virus and autoimmune responses in systemic lupus erythematosus. Front Immunol 3(11):623944. https://doi.org/10.3389/fimmu.2020.623944
Epstein MA, Achong BG, Barr YM (1964) Virus particles in cultured lymphoblasts from Burkitt’s lymphoma. Lancet 7335:702. https://doi.org/10.1016/s0140-6736(64)91524-7
Damania B, Kenney SC, Raab-Traub N (2022Sep 29) Epstein-Barr virus: biology and clinical disease. Cell 185(20):3652–3670. https://doi.org/10.1016/j.cell.2022.08.026
James JA, Kaufman KM, Farris AD, Taylor-Albert E, Lehman TJ, Harley JB (1997Dec 15) An increased prevalence of Epstein-Barr virus infection in young patients suggests a possible etiology for systemic lupus erythematosus. J Clin Invest 100(12):3019–3026. https://doi.org/10.1172/JCI119856
Han L, Zhang Y, Wang Q, Xin M, Yang K, Lei K et al (2018) Epstein-Barr virus infection and type I interferon signature in patients with systemic lupus erythematosus. Lupus 27(6):947–54. https://doi.org/10.1177/0961203317753069
Li ZX, Zeng S, Wu HX, Zhou Y (2019) The risk of systemic lupus erythematosus associated with Epstein-Barr virus infection: a systematic review and meta-analysis. Clin Exp Med 19(1):23–36. https://doi.org/10.1007/s10238-018-0535-0
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R et al (2019) 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann Rheum Dis 78(9):1151–1159. https://doi.org/10.1136/annrheumdis-2018-214819
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29(2):288–291
Fanouriakis A, Kostopoulou M, Alunno A, Aringer M, Bajema I, Boletis JN et al (2019) 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 78(6):736–745. https://doi.org/10.1136/annrheumdis-2019-215089
Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M et al (1996) The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 39(3):363–369. https://doi.org/10.1002/art.1780390303
Houen G, Trier NH (2021) Epstein-Barr virus and systemic autoimmune diseases. Front Immunol 7(11):587380. https://doi.org/10.3389/fimmu.2020.587380
Danza A, Ruiz-Irastorza G (2013) Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus 22(12):1286–1294. https://doi.org/10.1177/0961203313493032
França SAS, Viana JBGO, Góes HCA, Fonseca RRS, Laurentino RV, Costa IB et al (2022) Epidemiology of the Epstein-Barr virus in autoimmune inflammatory rheumatic diseases in Northern Brazil. Viruses 14(4):694. https://doi.org/10.3390/v14040694
Aygun D, Kuskucu MA, Sahin S, Adrovic A, Barut K, Yıldız M et al (2020) Epstein-Barr virus, cytomegalovirus and BK polyomavirus burden in juvenile systemic lupus erythematosus: correlation with clinical and laboratory indices of disease activity. Lupus 29(10):1263–1269. https://doi.org/10.1177/0961203320940029
Piroozmand A, Haddad Kashani H, Zamani B (2017) Correlation between Epstein-Barr virus infection and disease activity of systemic lupus erythematosus: a cross-sectional study. Asian Pac J Cancer Prev 18(2):523–527. https://doi.org/10.22034/APJCP.2017.18.2.523
Jog NR, Young KA, Munroe ME, Harmon MT, Guthridge JM, Kelly JA et al (2019) Association of Epstein-Barr virus serological reactivation with transitioning to systemic lupus erythematosus in at-risk individuals. Ann Rheum Dis 78(9):1235–1241. https://doi.org/10.1136/annrheumdis-2019-215361
Harley JB, Chen X, Pujato M, Miller D, Maddox A, Forney C et al (2018) Transcription factors operate across disease loci, with EBNA2 implicated in autoimmunity. Nat Genet 50(5):699–707. https://doi.org/10.1038/s41588-018-0102-3
Lu X, Chen X, Forney C, Donmez O, Miller D, Parameswaran S et al (2021) Global discovery of lupus genetic risk variant allelic enhancer activity. Nat Commun 12(1):1611. https://doi.org/10.1038/s41467-021-21854-5
Karrar S, Graham DS (2018) Abnormal B cell development in systemic lupus erythematosus: what the genetics tell us. Arthritis Rheumatol 70:496–507. https://doi.org/10.1002/art.40396
Laurynenka V, Ding L, Kaufman KM, James JA, Harley JB (2022Feb) A high prevalence of anti-EBNA1 heteroantibodies in systemic lupus erythematosus (SLE) supports anti-EBNA1 as an origin for SLE autoantibodies. Front Immunol 17(13):830993. https://doi.org/10.3389/fimmu.2022.830993
Kanduc D, Shoenfeld Y (2020) From anti-EBV immune responses to the EBV diseasome via cross-reactivity. Glob Med Genet 7(2):51–63. https://doi.org/10.1055/s-0040-1715641
Zucchi D, Silvagni E, Elefante E, Signorini V, Cardelli C, Trentin F et al (2023) Systemic lupus erythematosus: one year in review 2023. Clin Exp Rheumatol 41(5):997–1008. https://doi.org/10.55563/clinexprheumatol/4uc7e8
Freitas EC, de Oliveira MS, Monticielo OA (2017) Pristane-induced lupus: considerations on this experimental model. Clin Rheumatol 36(11):2403–2414. https://doi.org/10.1007/s10067-017-3811-6
Jarrett AF, Armstrong AA, Alexander E (1996) Epidemiology of EBV and Hodgkin’s lymphoma. Ann Oncol 7(Suppl 4):5–10. https://doi.org/10.1093/annonc/7.suppl_4.s5
de Melo SJ, Pinheiro-Silva R, Dhyani A, Pontes GS (2020Oct) Cytomegalovirus and Epstein-Barr infections: prevalence and impact on patients with hematological diseases. Biomed Res Int 2020:1627824. https://doi.org/10.1155/2020/1627824
Miao Y, Zhang J, Chen Q, Xing L, Qiu T, Zhu H et al (2022Aug) Spectrum and trigger identification of hemophagocytic lymphohistiocytosis in adults: a single-center analysis of 555 cases. Front Immunol 12(13):970183. https://doi.org/10.3389/fimmu.2022.970183
Gavriilaki E, de Latour RP, Risitano AM (2022) Advancing therapeutic complement inhibition in hematologic diseases: PNH and beyond. Blood 139(25):3571–3582. https://doi.org/10.1182/blood.2021012860
Wang Z, Bo L, Xu Y, Liu H, Zhao Y (2021) Features of serum complement C3 and C4 levels in autoimmune hemolytic anemia patients. Int J Lab Hematol 43(5):1154–1158. https://doi.org/10.1111/ijlh.13469
Ba H, Xu L, Peng H, Lin Y, Li X, Wang H et al (2019) Chronic active Epstein-Barr virus infection with systemic vasculitis and pulmonary arterial hypertension in a child. Front Pediatr 7:219. https://doi.org/10.3389/fped.2019.00219
Kano K, Katayama T, Takeguchi S, Asanome A, Takahashi K, Saito T et al (2017) Biopsy-proven case of Epstein-Barr virus (EBV)-associated vasculitis of the central nervous system. Neuropathology 37(3):259–264. https://doi.org/10.1111/neup.12356
Dong X, Liu L, Wang Y, Yang X, Wang W, Lin L et al (2019) Novel heterogeneous mutation of TNFAIP3 in a Chinese patient with Behçet-like phenotype and persistent EBV viremia. J Clin Immunol 39(2):188–194. https://doi.org/10.1007/s10875-019-00604-9
Tao L, Zhang T, Zhou Y, Liu X, Ding C, Yu J et al (2023) Epstein-Barr virus downregulates the α7 nicotinic acetylcholine receptor of CD8+ T lymphocytes might associate with coronary artery lesions in Kawasaki disease patients. Microbes Infect 25(7):105168. https://doi.org/10.1016/j.micinf.2023.105168
Al Sawah S, Zhang X, Zhu B, Magder LS, Foster SA, Iikuni N et al (2015) Effect of corticosteroid use by dose on the risk of developing organ damage over time in systemic lupus erythematosus-the Hopkins Lupus Cohort. Lupus Sci Med 2(1):e000066. https://doi.org/10.1136/lupus-2014-000066
Urowitz MB, Aranow C, Asukai Y, Bass DL, Bruce IN, Chauhan D et al (2022) Impact of belimumab on organ damage in systemic lupus erythematosus. Arthritis Care Res (Hoboken) 74(11):1822–1828. https://doi.org/10.1002/acr.24901
Lu JJ, Chen DY, Hsieh CW, Lan JL, Lin FJ, Lin SH (2007) Association of Epstein-Barr virus infection with systemic lupus erythematosus in Taiwan. Lupus 16(3):168–175. https://doi.org/10.1177/0961203306075800
Ming B, Bai M, Cai S, Wang B, Zhong J, Dong L (2023Jan) Clinical characteristics of SLE patients infected with Epstein-Barr virus and potential associated risk factors. Clin Rheumatol 42(1):101–109. https://doi.org/10.1007/s10067-022-06369-8
Liu J, Gao H, Xu LP, Mo XD, Liu R, Liang S et al (2020Mar) Immunosuppressant indulges EBV reactivation and related lympholytic disease by inhibiting Vδ2+ T cells activities after hematopoietic transplantation for blood malignancies. J Immunother Cancer 8(1):e000208. https://doi.org/10.1136/jitc-2019-000208
Funding
Wenling Social Development Science and Technology Program (No. 2023S00052).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• The proportion of vasculitis, serositis, and hematological involvement was higher in patients with SLE and lytic EBV infection.
• A higher proportion of patients with SLE and lytic EBV infection required methylprednisolone pulse therapy than those with latent infection.
• Patients with SLE and lytic EBV infection were more likely to be treated with more than two immunosuppressive agents or agents combined with multitarget biologic therapy.
• Patients with SLE and latent EBV infection reached disease remission significantly sooner than those with lytic infection group.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, M., Tu, J., Huang, M. et al. A retrospective cohort study of Epstein-Barr virus infection status and systemic lupus erythematosus. Clin Rheumatol 43, 1521–1530 (2024). https://doi.org/10.1007/s10067-024-06917-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-024-06917-4