Abstract
Background
Lumbar spondylolysis involves a bony defect in the vertebral pars interarticularis, predominantly affecting the lower lumbar spine. This condition is a significant etiological factor in lumbar instability and recurrent lower back pain, particularly in young individuals. While conservative treatments are the primary intervention, they often fail to provide relief, necessitating surgical approaches. Notwithstanding, executing bone grafting and fixation in the pars interarticularis defect simultaneously through minimally invasive surgery remains challenging.
Method
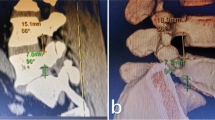
This study elucidates the biportal endoscopic spinal surgery (BESS) technique, innovatively applied for bone graft repair and percutaneous cannulated screw fixation in a patient with lumbar spondylolysis. We offer a detailed walkthrough of the technical procedures supplemented with follow-up radiographic evidence.
Results
The BESS technique facilitated meticulous clearance of the defect site, coupled with bone grafting and cannulated screw fixation, effectively addressing lumbar spondylolysis through a minimally invasive approach. This method holds promise for achieving substantial osseous fusion at the vertebral pars interarticularis defect site.
Conclusion
The BESS procedure for lumbar spondylolysis ensures a clean and prepared defect site for grafting and encourages successful osseous fusion, spotlighting its potential as a viable surgical strategy in managing this condition.









Similar content being viewed by others
Data Availability
The publisher's note above is accepted by all authors.
References
Aoki Y, Takahashi H, Nakajima A (2020) Prevalence of lumbar spondylolysis and spondylolisthesis in patients with degenerative spinal disease. Sci Rep 10(1):6739
Grogan JP, Hemminghytt S, Williams AL (1982) Spondylolysis studied with computed tomography. Radiology 145(3):737–742
Jamshidi AM, Soldozy S, Levi AD (2023) Percutaneous direct pars repair in young athletes. Neurosurgery 92(2):263–270
Jin M, Zhang J, Shao H (2020) Percutaneous endoscopic-assisted direct repair of pars defect without general anesthesia could be a satisfying treatment alternative for young patient with symptomatic lumbar spondylolysis: a technique note with case series. BMC Musculoskelet Disord 21(1):340
Leone A, Cianfoni A, Cerase A (2011) Lumbar spondylolysis: a review. Skeletal Radiol 40(6):683–700
Li DM, Li YC, Jiang W (2022) Application of a new anatomic hook-rod-pedicle screw system in young patients with lumbar spondylolysis: a pilot study. World J Clin Cases 10(17):5680–5689
Linhares D, Rodrigues PC, Silva MR (2019) Minimum of 10-year follow-up of V-rod technique in lumbar spondylolysis. Eur Spine J 28(7):1743–1749
Muthiah N, Ozpinar A, Eubanks J (2022) Direct pars repair with cannulated screws in adults: a case series and systematic literature review. World Neurosurg 163:e263–e274
Rothman SL, Glenn WV (1984) CT multiplanar reconstruction in 253 cases of lumbar spondylolysis. AJNR Am J Neuroradiol 5(1):81–90
Tanveer F, Arslan SA, Darain H (2021) Prevailing treatment methods for lumbar spondylolysis: a systematic review. Medicine (Baltimore) 100(51):e28319
Tawfik S, Phan K, Mobbs RJ (2020) The incidence of pars interarticularis defects in athletes. Global Spine J 10(1):89–101
Funding
This research received funding from the Capital Health Research and Development of Special, grant number SF No. 2022–2-6043.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol adhered to the guidelines of the Declaration of Helsinki and secured approval from the Ethics Committee of Peking University Shougang Hospital, under the reference number 2021ZZCX07. All participants granted informed consent to be included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 46986 KB)
Supplementary file2 (MP4 37087 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, W., Liu, Z., Lyu, P. et al. Biportal endoscopic bone graft repair and percutaneous screw fixation for lumbar spondylolysis—technical note and clinical outcomes. Acta Neurochir 166, 58 (2024). https://doi.org/10.1007/s00701-024-05944-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05944-z