Abstract
Purpose
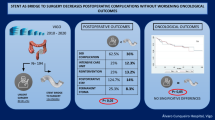
Intestinal decompression using self-expandable metallic colonic stents (SEMSs) as a bridge to surgery is now considered an attractive alternative to emergency surgery. However, data regarding the optimal timing of surgery after stenting are limited.
Methods
We investigated the impact of the interval between stenting and surgery on short- and long-term outcomes in 92 obstructive colorectal cancer (OCRC) patients who had a SEMS inserted and subsequently received curative surgery.
Results
The median age of the patients was 70.5 years, and the median interval between SEMS insertion and the surgery was 17 (range 5–47) days. There were 35 postoperative complications, including seven major postoperative complications. An interval of more than 16 days was an independent predictor of a poor relapse-free survival (hazard ratio [HR] = 3.12, 95% confidence interval [CI] 1.24–7.81, p = 0.015). An interval of more than 35 days was independently associated with major postoperative complications (HR = 16.6, 95% CI 2.21–125, p = 0.006).
Conclusion
A longer interval between stenting and surgery significantly compromised the short- and long-term outcomes. Surgery within 16 days after stenting might help maximize the benefit of SEMS without interfering with short- and long-term outcomes.


Similar content being viewed by others
References
The Global Cancer Observatory. 2020. https://gco.iarc.fr/ Accessed 6 June 2021.
McCullough JA, Engledow AH. Treatment options in obstructed left-sided colonic cancer. Clin Oncol. 2010;22:764–70.
Matsuda A, Miyashita M, Matsumoto S, et al. Comparison of long-term outcomes of colonic stent as “bridge to surgery” and emergency surgery for malignant large-bowel obstruction: a meta-analysis. Ann Surg Oncol. 2015;22:497–504.
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—update 2020. Endoscopy. 2020;52:389–407.
Arezzo A, Passera R, Lo Secco G, Verra M, Bonino MA, Targarona E, et al. Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials. Gastrointest Endosc. 2017;86:416–26.
Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L. Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol. 2017;2017:2863272.
Dohomoto M. New method-endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Dig. 1991;3:1507–12.
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, European Society of Gastrointestinal Endoscopy, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;46:990–1053.
Matsuzawa T, Ishida H, Yoshida S, Isayama H, Kuwai T, Maetani I, et al. A Japanese prospective multicenter study of self-expandable metal stent placement for malignant colorectal obstruction: short-term safety and efficacy within 7 days of stent procedure in 513 cases. Gastrointest Endosc. 2015;82:697–707.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, et al. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Frago R, Ramirez E, Millan M, Kreisler E, del Valle E, Biondo S. Current management of acute malignant large bowel obstruction: a systematic review. Am J Surg. 2014;207:127–38.
Gainant A. Emergency management of acute colonic cancer obstruction. J Visc Surg. 2012;149:e3-10.
Kye BH, Kim JH, Kim HJ, Lee YS, Lee IK, Kang WK, et al. The optimal time interval between the placement of self-expandable metallic stent and elective surgery in patients with obstructive colon cancer. Sci Rep. 2020;10:9502.
Broholm M, Kobborg M, Frostberg E, Jeppesen M, Gögenür I. Delay of surgery after stent placement for resectable malignant colorectal obstruction is associated with higher risk of recurrence. Int J Colorectal Dis. 2017;32:513–6.
Veld JV, Kumcu A, Amelung FJ, Borstlap WAA, Consten ECJ, Dekker JWT, et al. Time interval between self-expandable metal stent placement or creation of a decompressing stoma and elective resection of left-sided obstructive colon cancer. Endoscopy. 2020. https://doi.org/10.1055/a-1308-1487.
Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, et al. Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett. 2018;15:400–6.
Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94:1151–4.
Takahashi G, Yamada T, Iwai T, Takeda K, Koizumi M, Shinji S, et al. Oncological assessment of stent placement for obstructive colorectal cancer from circulating cell-free DNA and circulating tumor DNA dynamics. Ann Surg Oncol. 2018;25:737–44.
Haraguchi N, Ikeda M, Miyake M, Yamada T, Sakakibara Y, Mita E, et al. Colonic stenting as a bridge to surgery for obstructive colorectal cancer: advantages and disadvantages. Surg Today. 2016;46:1310–7.
Kim HJ, Choi GS, Park JS, Park SY, Jun SH. Higher rate of perineural invasion in stent-laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Colorectal Dis. 2013;28:407–14.
Foo CC, Poon SHT, Chiu RHY, Lam WY, Cheung LC, Law WL. Is bridge to surgery stenting a safe alternative to emergency surgery in malignant colonic obstruction: a meta-analysis of randomized control trials. Surg Endosc. 2019;33:293–302.
Ribeiro IB, Bernardo WM, Martins BDC, de Moura DTH, Baba ER, Josino IR, et al. Colonic stent versus emergency surgery as treatment of malignant colonic obstruction in the palliative setting: a systematic review and meta-analysis. Endosc Int Open. 2018;6:E558–67.
Sato R, Oikawa M, Kakita T, Okada T, Oyama A, Abe T, et al. Comparison of the long-term outcomes of the self-expandable metallic stent and transanal decompression tube for obstructive colorectal cancer. Ann Gastroenterol Surg. 2019;3:209–16.
Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Kawano Y, Yamada T, et al. Optimal interval from placement of a self-expandable metallic stent to surgery in patients with malignant large bowel obstruction: a preliminary study. Surg Laparosc Endosc Percutan Tech. 2018;28:239–44.
Lee GJ, Kim HJ, Baek JH, Lee WS, Kwon KA. Comparison of short-term outcomes after elective surgery following endoscopic stent insertion and emergency surgery for obstructive colorectal cancer. Int J Surg. 2013;11:442–6.
Saito S, Yoshida S, Isayama H, Matsuzawa T, Kuwai T, Maetani I, et al. A prospective multicenter study on self-expandable metallic stents as a bridge to surgery for malignant colorectal obstruction in Japan: efficacy and safety in 312 patients. Surg Endosc. 2016;30:3976–86.
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sato, R., Oikawa, M., Kakita, T. et al. A longer interval after stenting compromises the short- and long-term outcomes after curative surgery for obstructive colorectal cancer. Surg Today 52, 681–689 (2022). https://doi.org/10.1007/s00595-021-02385-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-021-02385-4