Abstract
Purpose
Delirium after transcatheter aortic valve implantation (TAVI) should be prevented because it is associated with worse patient outcomes. Perioperative administration of benzodiazepines is a risk factor for postoperative delirium; however, the association between remimazolam, a newer ultrashort-acting benzodiazepine for general anesthesia, and postoperative delirium remains unclear. This study aimed to evaluate whether remimazolam administration during TAVI under general anesthesia affected the incidence of postoperative delirium.
Methods
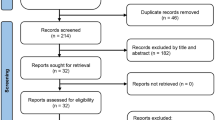
This single-center retrospective study recruited all adult patients who underwent transfemoral TAVI (TF-TAVI) under general anesthesia between March 2020 and May 2022. Patients were divided into the remimazolam (R) and propofol (P) groups according to the sedative used for anesthesia. In the R group, all patients received flumazenil after surgery. The primary endpoint was the incidence of delirium within 3 days after surgery. Factors associated with delirium after TF-TAVI were examined by multiple logistic regression analysis.
Results
Ninety-eight patients were included in the final analysis (R group, n = 40; P group, n = 58). The incidence of postoperative delirium was significantly lower in the R group than in the P group (8% vs. 26%, p = 0.032). Multiple logistic regression analysis revealed that remimazolam (odds ratio 0.17, 95% CI 0.04–0.80, p = 0.024) was independently associated with the incidence of postoperative delirium, even after adjustment for age, sex, preoperative cognitive function, history of stroke, and TF-TAVI approach.
Conclusion
Remimazolam may benefit TF-TAVI in terms of postoperative delirium; however, its usefulness must be further evaluated in extensive prospective studies.

Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Tse L, Bowering JB, Schwarz SK, Moore RL, Burns KD, Barr AM. Postoperative delirium following transcatheter aortic valve implantation: a historical cohort study. Can J Anaesth. 2015;62:22–30.
Eide LS, Ranhoff AH, Fridlund B, Haaverstad R, Hufthammer KO, Kuiper KK, Nordrehaug JE, Norekvål TM, CARDELIR Investigators. Comparison of frequency, risk factors, and time course of postoperative delirium in octogenarians after transcatheter aortic valve implantation versus surgical aortic valve replacement. Am J Cardiol. 2015;115:802–9.
Maniar HS, Lindman BR, Escallier K, Avidan M, Novak E, Melby SJ, Damiano MS, Lasala J, Quader N, Rao RS, Lawton J, Moon MR, Helsten D, Pasque MK, Damiano RJ Jr, Zajarias A. Delirium after surgical and transcatheter aortic valve replacement is associated with increased mortality. J Thorac Cardiovasc Surg. 2016;151:81-23.e2.
Goins AE, Smeltz A, Ramm C, Strassle PD, Teeter EG, Vavalle JP, Kolarczyk L. General anesthesia for transcatheter aortic valve replacement: total intravenous anesthesia is associated with less delirium as compared to volatile agent technique. J Cardiothorac Vasc Anesth. 2018;32:1570–7.
van der Wulp K, van Wely M, van Heijningen L, van Bakel B, Schoon Y, Verkroost M, Gehlmann H, Van Garsse L, Vart P, Kievit P, Rikkert MO, Morshuis W, van Royen N. Delirium after transcatheter aortic valve implantation under general anesthesia: incidence, predictors, and relation to long-term survival. J Am Geriatr Soc. 2019;67:2325–30.
Maldonado JR. Acute brain failure: pathophysiology, diagnosis, management, and sequelae of delirium. Crit Care Clin. 2017;33:461–519.
Pisano A, Torella M, Yavorovskiy A, Landoni G. The impact of anesthetic regimen on outcomes in adult cardiac surgery: a narrative review. J Cardiothorac Vasc Anesth. 2021;35:711–29.
Weinstein SM, Poultsides L, Baaklini LR, Mörwald EE, Cozowicz C, Saleh JN, Arrington MB, Poeran J, Zubizarreta N, Memtsoudis SG. Postoperative delirium in total knee and hip arthroplasty patients: a study of perioperative modifiable risk factors. Br J Anaesth. 2018;120:999–1008.
Memtsoudis S, Cozowicz C, Zubizarreta N, Weinstein SM, Liu J, Kim DH, Poultsides L, Berger MM, Mazumdar M, Poeran J. Risk factors for postoperative delirium in patients undergoing lower extremity joint arthroplasty: a retrospective population-based cohort study. Reg Anesth Pain Med. 2019. https://doi.org/10.1136/rapm-2019-100700 (published online ahead of print, 2019 Jul 12).
Chaiwat O, Chanidnuan M, Pancharoen W, Vijitmala K, Danpornprasert P, Toadithep P, Thanakiattiwibun C. Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol. 2019;19:39.
Marcantonio ER, Juarez G, Goldman L, Mangione CM, Ludwig LE, Lind L, Katz N, Cook EF, Orav EJ, Lee TH. The relationship of postoperative delirium with psychoactive medications. JAMA. 1994;272:1518–22.
Zaal IJ, Devlin JW, Hazelbag M, Klein Klouwenberg PM, van der Kooi AW, Ong DS, Cremer OL, Groenwold RH, Slooter AJ. Benzodiazepine-associated delirium in critically ill adults. Intensive Care Med. 2015;41:2130–7.
Masui K. Remimazolam besilate, a benzodiazepine, has been approved for general anesthesia!! J Anesth. 2020;34:479–82.
Kilpatrick GJ, McIntyre MS, Cox RF, Stafford JA, Pacofsky GJ, Lovell GG, Wiard RP, Feldman PL, Collins H, Waszczak BL, Tilbrook GS. CNS 7056: a novel ultra-short-acting benzodiazepine. Anesthesiology. 2007;107:60–6.
Chen X, Sang N, Song K, Zhong W, Wang H, Jiang J, Huang Y, Hu P. Psychomotor recovery following remimazolam-induced sedation and the effectiveness of flumazenil as an antidote. Clin Ther. 2020;42:614–24.
Sneyd JR, Gambus PL, Rigby-Jones AE. Current status of perioperative hypnotics, role of benzodiazepines, and the case for remimazolam: a narrative review. Br J Anaesth. 2021;127:41–55.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
National Collaborating Centre for Mental Health (UK). Dementia: a NICE-SCIE guideline on supporting people with dementia and their carers in health and social care. Leicester (UK): British Psychological Society; 2007.
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautam S, Bernard GR, Inouye SK. Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med. 2001;29:1370–9.
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–8.
Vasilevskis EE, Han JH, Hughes CG, Ely EW. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012;26:277–87.
Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol. 2009;5:210–20.
Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125:492–504.
Antonik LJ, Goldwater DR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): Part I. Safety, efficacy, and basic pharmacokinetics. Anesth Analg. 2012;115:274–83.
Wiltshire HR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): Part II. Population pharmacokinetic and pharmacodynamic modeling and simulation. Anesth Analg. 2012;115:284–96.
Eisenried A, Schüttler J, Lerch M, Ihmsen H, Jeleazcov C. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers: Part II. Pharmacodynamics of electroencephalogram effects. Anesthesiology. 2020;132:652–66.
Tieges Z, McGrath A, Hall RJ, Maclullich AM. Abnormal level of arousal as a predictor of delirium and inattention: an exploratory study. Am J Geriatr Psychiatry. 2013;21:1244–53.
Jhuang BJ, Yeh BH, Huang YT, Lai PC. Efficacy and safety of remimazolam for procedural sedation: a meta-analysis of randomized controlled trials with trial sequential analysis. Front Med (Lausanne). 2021;8: 641866.
Zhang J, Wang X, Zhang Q, Wang Z, Zhu S. Application effects of remimazolam and propofol on elderly patients undergoing hip replacement. BMC Anesthesiol. 2022;22:118.
Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34:543–53.
Tan Y, Ouyang W, Tang Y, Fang N, Fang C, Quan C. Effect of remimazolam tosilate on early cognitive function in elderly patients undergoing upper gastrointestinal endoscopy. J Gastroenterol Hepatol. 2022;37:576–83.
Mao Y, Guo J, Yuan J, Zhao E, Yang J. Quality of recovery after general anesthesia with remimazolam in patients’ undergoing urologic surgery: a randomized controlled trial comparing remimazolam with propofol. Drug Des Devel Ther. 2022;16:1199–209.
Hirata N, Hayamizu K, Yamakage M. How to administer remimazolam for anesthesia induction. J Anesth. 2020;34:962.
Yamamoto T, Kurabe M, Kamiya Y. Re-sleeping after reversal of remimazolam by flumazenil. J Anesth. 2021;35:322.
Yamamoto T, Kurabe M, Kamiya Y. A mechanism of re-sedation caused by remimazolam. J Anesth. 2021;35:467–8.
Arbel Y, Zivkovic N, Mehta D, Radhakrishnan S, Fremes SE, Rezaei E, Cheema AN, Al-Nasser S, Finkelstein A, Wijeysundera HC. Factors associated with length of stay following trans-catheter aortic valve replacement—a multicenter study. BMC Cardiovasc Disord. 2017;17:137.
Carli F, Mayo N. Measuring the outcome of surgical procedures: what are the challenges? Br J Anaesth. 2001;87:531–3.
Maessen JM, Dejong CH, Kessels AG, von Meyenfeldt MF, Enhanced Recovery After Surgery (ERAS) Group. Length of stay: an inappropriate readout of the success of enhanced recovery programs. World J Surg. 2008;32:971–5.
Fiore JF Jr, Faragher IG, Bialocerkowski A, Browning L, Denehy L. Time to readiness for discharge is a valid and reliable measure of short-term recovery after colorectal surgery. World J Surg. 2013;37:2927–34.
Balvardi S, Pecorelli N, Castelino T, Niculiseanu P, Liberman AS, Charlebois P, Stein B, Carli F, Mayo NE, Feldman LS, Fiore JF Jr. Measuring in-hospital recovery after colorectal surgery within a well-established enhanced recovery pathway: a comparison between hospital length of stay and time to readiness for discharge. Dis Colon Rectum. 2018;61:854–60.
Pretto M, Spirig R, Milisen K, Degeest S, Regazzoni P, Hasemann W. Effects of an interdisciplinary nurse-led Delirium prevention and management program (DPMP) on nursing workload: a pilot study. Int J Nurs Stud. 2009;46:804–12.
Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168:27–32.
Wang ML, Min J, Sands LP, Leung JM, Perioperative Medicine Research Group. Midazolam premedication immediately before surgery is not associated with early postoperative delirium. Anesth Analg. 2021;133:765–71.
Acknowledgements
We would like to thank www.editage.jp for English language editing.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by SK, TM, and TI. Data collection, analysis, visualization, and project administration were performed by SK. The first draft of the manuscript was written by SK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kaneko, S., Morimoto, T., Ichinomiya, T. et al. Effect of remimazolam on the incidence of delirium after transcatheter aortic valve implantation under general anesthesia: a retrospective exploratory study. J Anesth 37, 210–218 (2023). https://doi.org/10.1007/s00540-022-03148-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-022-03148-2