Abstract
Pulmonary embolism is a major cause of maternal morbidity during pregnancy. Beside the frequently encountered thromboembolism, trophoblastic cell embolism has also been reported in a few case reports. This phenomenon may be symptomless in physiological gestational process but is more pronounced in contexts of preeclampsia or gestational trophoblastic disease. It was exceptionally reported to be associated with death. Here, we report the case of a 15-year-old girl, who experienced dyspnea followed by cardiac arrests and disseminated intravascular coagulation. Echocardiography showed a massive proximal pulmonary embolism. Abdominal sonography revealed that she was 11 weeks pregnant. Autopsy confirmed the presence of multiple clot emboli in the proximal pulmonary arteries. Additionally, the histopathological examination showed a massive syncytiotrophoblastic embolism in the lung microcirculation. Microscopic examination of the uterus revealed an exaggerated placental site reaction. In conclusion, this exhaustive post-mortem study describes a previously unreported association between exaggerated placental site reaction and pulmonary trophoblastic embolism, with fatal issue. Forensic pathologists should be aware that a large sampling of the lungs and uterus and examination of both placenta and fetus are needed to achieve this diagnosis. This case study emphasizes the need for further work elucidating pathways of trophoblast deportation.
Similar content being viewed by others
Introduction
Venous thromboembolism, composed of pulmonary embolism and deep venous thrombosis, is a significant cause of maternal mortality in the developed world. Pregnant women are 4 to 5 times more likely to develop venous thromboembolism than women who are not. This predisposition to develop venous thromboembolism results from the hypercoagulable state of pregnancy which may have various origins [1].
Non-thrombotic pulmonary embolism may be caused by embolization of different types of cells (adipocytes, hematopoietic, amniotic, or tumor cells), bacteria, fungi, foreign material, or gas [2] and is related in most of cases to amniotic fluid emboli. The latter during first trimester of pregnancy is exceedingly rare [3, 4]. Trophoblastic cell embolism is a rare condition, which is mainly associated with preeclampsia or gestational trophoblastic disease. An association of cerebral trophoblastic cell embolism and massive pulmonary embolization leading a sudden death following artificial abortion during the first trimester has been previously reported in a 42-year-old woman [5].
In the present case study, we describe a previously unreported association of blood clots and trophoblastic pulmonary embolism and exaggerated placental site reaction, with fatal issue.
Case study
A 15-year-old girl with history of anxiety attacks experienced severe dyspnea and polypnea at home. Upon the arrival of the mobile medical team, the patient was in non-shockable cardiac arrest with an undetermined no flow period. The patient recovered a stable heart rhythm after 55 min of advanced life support including 6 boli of 1 mg of epinephrine. At admission in the intensive care unit, echocardiography findings were a typical acute cor pulmonale with a thrombus in the pulmonary artery trunk. A stage E (A modifier) cardiogenic shock was diagnosed considering a near pulselessness state with deep arterial hypotension, a cardiac output at 1.3 L/min under high doses of epinephrine, and a lactatemia at 11.8 mmol/l. Decision was to place a veno-arterial extracorporeal membrane oxygenation (VA-ECMO).
After VA-ECMO placement, physical examination showed bilateral non-reactive mydriasis with a Glasgow Coma Scale (GCS) score of 3/15. Laboratory assays revealed prolonged activated partial thromboplastin time (aPTT) (> 5), 28% prothrombin time (PT), thrombocytopenia (134 G/L), low fibrinogen (1,1 g/L), and high fibrin monomer (> 150 µg/mL), all suggestive of a disseminated intravascular coagulation state (DIC). An abdominal ultrasound scan found an intrauterine pregnancy with no cardiac activity. Gestational age was estimated at around 11 weeks of amenorrhea. SARS-CoV-2 RT-PCR performed on a naso-pharyngeal swab was negative. Soon after VA-ECMO placement, a refractory post cardiac arrest syndrome occurred, requiring massive fluid challenge, high doses of norepinephrine and vasopressin. A hemorrhagic shock at cannulation site also led to massive packed red blood cells, platelet, plasma, and fibrinogen transfusions. Considering this clinical pattern, a discontinuation of life-sustaining therapies was collegially decided, and death occurred few hours later.
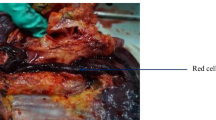
A medical autopsy was conducted 2 days after death. It revealed multiple clot emboli of pulmonary arteries and arterioles. No vein thrombosis was found in the lower limb or pelvis. Mild hemorrhagic infiltration was observed around the right auricula, the tongue, the thyroid, and the esophagus. There was a mild right subarachnoid hemorrhage. Macroscopic examination of the uterus showed no mass lesion, and a grossly normal placental implantation. Fetal autopsy did not show any malformations, and no maceration. Biometric data of the fetus were consistent with a gestational age of 11 weeks.
Organs were sampled and fixed in 4% neutral buffered formalin, and 4 μm thickness tissue sections were performed and stained with hematoxylin, eosin, and saffron (HES). Microscopic study of lung vessels showed arteriolar and arterial thrombi appearing as platelet–fibrin structures or, focally, partially organized older lesions containing few fibroblasts. Additionally, abundant multinucleated syncytial-like structures supposed to be syncytiotrophoblast cells were found in small arterioles and capillaries of the interalveolar septa (Fig. 1), in almost all low power fields. Multifocal presence of megakaryocytes was also noticed in the pulmonary microcirculation.
Examination of the uterus revealed poorly defined infiltration of the myometrium by mononucleated dissociated cells to a depth of 4 mm at the implantation site, in the uterine corpus. They contained a slightly irregular hyperchromatic nucleus and an abundant eosinophilic or clarified cytoplasm. This aspect was compatible with intermediate trophoblastic cells. Some cells were multinucleated. Neither atypia, mitoses, necrosis, nor solid zones were observed. There was no destructive growth. An exuberant infiltration of myometrial vessels by syncytiotrophoblastic cells clusters was noticed (Fig. 2). Microscopic examination of the placenta showed a hyperplasia of the syncytiotrophoblast consistent with the gestational age. Placental villi presented a normal size, regular contours and were not hydropic. Immunohistochemical assay with PDL1 (QR1), CK7, and GATA3 revealed a staining of the intermediate trophoblastic cells that infiltrated the myometrium. There was no expression of inhibin and p63. Syncytiotrophoblast cells in the myometrial and pulmonary vessels were stained with anti-beta-HCG and anti-cytokeratin AE1/AE3 antibodies. These latter did not show any squamous cell in the lung or uterine vessels. Alcian blue staining was negative, thus excluding the diagnosis of amniotic emboli. An in situ hybridization assay (HER2, DDISH, Roche) confirmed the diploidy of the villous stromal cells, thus excluding the diagnosis of partial hydatidiform mole. Anti-CD61 antibody highlighted the presence of megakaryocytes in the lung microcirculation.
Heart analysis revealed an edematous myocardium with mild inflammatory infiltration composed of polymorphonuclear neutrophils. A few contraction bands were present. Acute tubular necrosis and microthrombi of the microcirculation were observed in the kidney. Lesions of ischemic necrosis were found in the liver parenchyma, the colon, and the small intestine. A hemorrhagic infiltration, without significant inflammation, was observed around the periaortic adipose tissue, in the wall of the right atrium, in the tongue muscular tissue, in the adrenal gland parenchyma, in the perirenal adipose tissue, in the esophageal wall, and in the psoas. Histopathological examination of the thyroid, spleen, stomach, thymus, and pancreas revealed no specific abnormality. No embolism was found in other organs.
Discussion
In this original post-mortem case study, we describe a case of exaggerated placental site and concomitant trophoblastic embolism (TE), which led to pulmonary thromboembolism and death.
Trophoblastic pulmonary embolism was first described by Schmorl et al. [6] in deceased pregnant women affected with eclampsia. He described knots of multinucleated syncytiotrophoblast in the myometrial vessels and in the lung microcirculation. TE was then described in gestational trophoblastic diseases, after elective abortion [7] and conservative treatment of placenta accreta [8]. Garner et al. [9] reported on trophoblastic pulmonary embolization in a 27-year-old woman following abdominal hysterectomy for invasive gestational trophoblastic disease (Mola destruens), with complete recovery after 72 h without long-term sequelae. TE was also described in a fatal case of amniotic fluid embolism, in association with components of amniotic fluid [10]. Death following TE is rare and has been reported in cases of molar pregnancies [11], as a side effect of chemotherapy of choriocarcinoma [12], and in a normal pregnancy [13]. An association of cerebral trophoblastic cells embolism and massive pulmonary embolization leading a sudden death following artificial abortion has been previously reported in a 42-year-old woman [5]. Ikarashi found TE in three of eight maternal autopsy cases [14]. Additionally, asymptomatic deportation of fewer trophoblastic debris may be frequent in normal pregnancies [15, 16]. Mononuclear cytotrophoblast cells were also extracted from peripheral blood [16, 17]. Trophoblastic debris were reported to be associated with inflammation, endothelial dysfunction [18], and hypercoagulability [19]. This could probably explain the development of pulmonary thromboembolism and disseminated intravascular coagulation that occurred in the present case.
This young patient did not present molar pregnancy or preeclampsia. However, an exaggerated placental site (EPS) reaction was found in the uterus. This EPS represents the extreme end of a physiological process rather than a true lesion, consisting of an exuberant infiltration of the decidua and myometrium by implantation site intermediate trophoblast cells (ISITs) and syncytiotrophoblast at the implantation site [20, 21]. ISITs differentiate from the cytotrophoblast during the process of placenta formation. They anchor the placenta to the maternal tissue, invade spiral arteries, and are considered to maintain pregnancy [20]. Distinction with physiological process may be somewhat arbitrary because there are no reliable data quantifying the amount and extent of trophoblast infiltration at different stages of normal gestation. The pathological significance of EPS has not been clearly determined. This nonneoplastic lesion can develop from early to term pregnancy and may be found with abortion or molar pregnancy or diagnosed several days or weeks after delivery. Patients may present bleeding, elevated beta-HCG, or rarely an intrauterine mass. Others are asymptomatic [22,23,24]. It resolves spontaneously after curettage but is difficult to diagnose without histopathological examination of a hysterectomy specimen. Histologically, the cells resemble usual ISITs. Villi and decidua may be present. The cells are diffusely positive for GATA3 [25], CK7, PDL-1, Mel-CAM, and hPL. The most important differential diagnosis of EPS is placental site trophoblastic tumor (PSTT), which usually forms a confluent mass of trophoblastic cells with unequivocal mitosis and a Ki-67 labeling index higher than 10%. Chorionic villi are absent in PSTT. Other diagnostics include other neoplastic trophoblastic lesions such as epithelioid trophoblastic tumor and placental site nodule.
The mechanisms by which trophoblasts are deported from the placenta to the maternal circulation are not fully understood [15, 26]. Trophoblast deportation has never been described in association with EPS. Possible mechanisms could involve migration of the syncytiotrophoblastic component of EPS, or differentiation of intermediate trophoblast into syncytiotrophoblast and following embolization. Another hypothesis is that EPS may induce ischemia as seen in preeclampsia, favoring the shedding of syncytiotrophoblast. Additionally, the occurrence of TE was reported to be associated with amniotic fluid emboli. The higher frequency of EPS in molar pregnancies may partly explain the association of molar pregnancies with TE.
From the forensic pathologist point of view, this case study highlights the importance of an extensive sampling of the lungs and uterine corpus in case of maternal death, even in the first and second trimester of pregnancies, associated with a specialized pathological examination of both fetus and placenta. As TE may be associated with amniotic fluid embolism [10], a meticulous examination of lung and uterus circulation is needed, looking for squams, lanugo hair, meconium, mucin, and sebum (using if necessary anti-CKAE1-AE3 antibody and Alcian blue staining). Additionally, a large sampling of the myometrium, perpendicular to the interface between the endometrium and placenta, is necessary in order to screen for abnormal placental implantation or trophoblastic tumor. Differential diagnoses include neoplastic emboli, most notably choriocarcinoma or diverse type of poorly differentiated carcinoma, and megakaryocytes emboli. In the present case, we also found megakaryocytes in the lung microcirculation, which were easily discernable from syncytiotrophoblasts by using anti-CD61 antibody. Megakaryocyte’s emboli are a nonspecific finding that may be associated with various causes of shock.
In conclusion, this case study outlines that trophoblastic embolism should be considered in cases of respiratory distress in pregnancy. A large sampling of the lungs and uterus and the examination of both placenta and fetus are needed to achieve this diagnosis. This first description of the association between EPS and TE highlights the need for further work explaining mechanisms of trophoblastic deportation.
References
James Andra H (2009) Venous thromboembolism in pregnancy. Arterioscler Thromb Vasc Biol 29:326–331. https://doi.org/10.1161/ATVBAHA.109.184127
Jorens PG, Van Marck E, Snoeckx A, Parizel PM (2009) Nonthrombotic pulmonary embolism. Eur Respir J 34:452–474. https://doi.org/10.1183/09031936.00141708
Wernet A, Luton D, Muller F, Ducarme G (2014) Use of insulin-like growth factor binding protein-1 for retrospective diagnosis of amniotic fluid embolism in first trimester. Arch Gynecol Obstet 289:461–462. https://doi.org/10.1007/s00404-013-2970-1
Guidotti RJ, Grimes DA, Cates W (1981) Fatal amniotic fluid embolism during legally induced abortion, United States, 1972 to 1978. Am J Obstet Gynecol 141:257–261. https://doi.org/10.1016/s0002-9378(16)32629-1
Habek D, Janculjak D, Cerkez Habek J, Jalsovec D (2005) Sudden death because of massive pulmonary thromboembolism and concomitant cerebrovascular trophoblastic embolism following artificial abortion. Fetal Diagn Ther 20:390–392. https://doi.org/10.1159/000086818
Schmorl G (1893) Pathologisch-anatomische untersuchungen über Puerperal-Eklampsie. Verlag FCW Vogel, Leipzig
Kamoi S, Ohaki Y, Mori O et al (2003) Placental villotrophoblastic pulmonary emboli after elective abortion: immunohistochemical diagnosis and comparison with ten control cases. Int J Gynecol Pathol 22:303–309. https://doi.org/10.1097/01.PGP.0000054822.24312.59
Wang Q-M, Liu H-L, Dang Q (2015) Acute trophoblastic pulmonary embolism during conservative treatment of placenta accreta: case report and review of literature. Eur J Med Res 20:91. https://doi.org/10.1186/s40001-015-0185-6
Garner EI, Chang-Lee WY, Lu KH et al (1999) Trophoblastic pulmonary embolization after hysterectomy for invasive complete mole A case report. J Reprod Med 44:908–912
Lunetta P, Penttilä A (1996) Immunohistochemical identification of syncytiotrophoblastic cells and megakaryocytes in pulmonary vessels in a fatal case of amniotic fluid embolism. Int J Legal Med 108:210–214. https://doi.org/10.1007/BF01369794
Cohle SD, Petty CS (1985) Sudden death caused by embolization of trophoblast from hydatidiform mole. J Forensic Sci 30:1279–1283
Hoogland HJ, Arends JW, Blijham GH et al (1988) Death from chemotherapy in gestational trophoblastic disease. Eur J Obstet Gynecol Reprod Biol 29:167–172. https://doi.org/10.1016/0028-2243(88)90144-X
Delmis J, Pfeifer D, Ivanisevic M et al (2000) Sudden death from trophoblastic embolism in pregnancy. Eur J Obstet Gynecol Reprod Biol 92:225–227. https://doi.org/10.1016/S0301-2115(99)00281-X
Ikarashi T, Takeuchi S, Ohnishi Y (1988) Trophoblastic embolism in sudden maternal death. Nihon Sanka Fujinka Gakkai Zasshi 40:793–795
Attwood HD, Park WW (1961) Embolism to the lungs by trophoblast. BJOG Int J Obstet Gynaecol 68:611–617. https://doi.org/10.1111/j.1471-0528.1961.tb02778.x
Johansen M, Redman CWG, Wilkins T, Sargent IL (1999) Trophoblast deportation in human pregnancy—its relevance for pre-eclampsia. Placenta 20:531–539. https://doi.org/10.1053/plac.1999.0422
Chua S, Wilkins T, Sargent I, Redman C (1991) Trophoblast deportation in pre-eclamptic pregnancy. Br J Obstet Gynaecol 98:973–979. https://doi.org/10.1111/j.1471-0528.1991.tb15334.x
Pantham P, Askelund KJ, Chamley LW (2011) Trophoblast deportation part II: a review of the maternal consequences of trophoblast deportation. Placenta 32:724–731. https://doi.org/10.1016/j.placenta.2011.06.019
Reverdiau P, Jarousseau AC, Thibault G et al (1995) Tissue factor activity of syncytiotrophoblast plasma membranes and tumoral trophoblast cells in culture. Thromb Haemost 73:49–54
Shih IM, Kurman RJ (2001) The pathology of intermediate trophoblastic tumors and tumor-like lesions. Int J Gynecol Pathol 20:31–47. https://doi.org/10.1097/00004347-200101000-00004
Cheung AN-Y (2003) Pathology of gestational trophoblastic diseases. Best Pract Res Clin Obstet Gynaecol 17:849–868. https://doi.org/10.1016/s1521-6934(03)00094-4
Liu G, Yuan B, Wang Y (2013) Exaggerated placental site leading to postpartum hemorrhage: a case report. J Reprod Med 58:448–450
De Miguel JR, Quintana R, González-Rodilla I et al (2014) Exaggerated placental site/placental site trophoblastic tumor: an underestimated risk factor for emergency peripartum hysterectomy. Clin Exp Obstet Gynecol 41:638–640
Takebayashi A, Kimura F, Yamanaka A et al (2014) Exaggerated placental site, consisting of implantation site intermediate trophoblasts, causes massive postpartum uterine hemorrhage: case report and literature review. Tohoku J Exp Med 234:77–82. https://doi.org/10.1620/tjem.234.77
Banet N, Gown AM, Shih I-M et al (2015) GATA-3 expression in trophoblastic tissues: an immunohistochemical study of 445 cases, including diagnostic utility. Am J Surg Pathol 39:101–108. https://doi.org/10.1097/PAS.0000000000000315
Askelund KJ, Chamley LW (2011) Trophoblast deportation part I: review of the evidence demonstrating trophoblast shedding and deportation during human pregnancy. Placenta 32:716–723. https://doi.org/10.1016/j.placenta.2011.07.081
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was lead in respect of the French law relevant to medical autopsy and bio-medical research.
Informed consent
The family consent was obtained for autopsy and case study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pina, H., Kimmoun, A., Marchand, E. et al. Fatal massive pulmonary thromboembolism and concomitant pulmonary trophoblastic embolism associated with exaggerated placental site reaction: a case study. Int J Legal Med 135, 2357–2361 (2021). https://doi.org/10.1007/s00414-021-02710-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-021-02710-z