Abstract
Introduction
Survival following lung transplant is low. With limited donor lung availability, predicting post-transplant survival is key. We investigated the predictive value of pre-transplant CT biomarkers on survival.
Methods
In this single-center retrospective cohort study of adults in a diverse, underserved, urban lung transplant program (11/8/2017–5/20/2022), chest CTs were analyzed using TeraRecon to assess musculature, fat, and bone. Erector spinae and pectoralis muscle area and attenuation were analyzed. Sarcopenia thresholds were 34.3 (women) and 38.5 (men) Hounsfield Units (HU). Visceral and subcutaneous fat area and HU, and vertebral body HU were measured. Demographics and pre-transplant metrics were recorded. Survival analyses included Kaplan–Meier and Cox proportional hazard.
Results
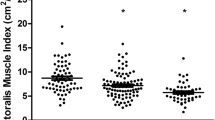
The study cohort comprised 131 patients, 50 women, mean age 60.82 (SD 10.15) years, and mean follow-up 1.78 (SD 1.23) years. Twenty-nine percent were White. Mortality was 32.1%. Kaplan–Meier curves did not follow the proportional hazard assumption for sex, so analysis was stratified. Pre-transplant EMR metrics did not predict survival. Women without sarcopenia at erector spinae or pectoralis had 100% survival (p = 0.007). Sarcopenia did not predict survival in men and muscle area did not predict survival in either sex. Men with higher visceral fat area and HU had decreased survival (p = 0.02). Higher vertebral body density predicted improved survival in men (p = 0.026) and women (p = 0.045).
Conclusion
Pre-transplantation CT biomarkers had predictive value in lung transplant survival and varied by sex. The absence of sarcopenia in women, lower visceral fat attenuation and area in men, and higher vertebral body density in both sexes predicted survival in our diverse, urban population.





Similar content being viewed by others
References
Valapour M, Lehr CJ, Skeans MA et al (2022) OPTN/SRTR 2020 annual data report: lung. Am J Transplant 22(S2):438–518. https://doi.org/10.1111/ajt.16991
Kobashigawa J, Dadhania D, Bhorade S et al (2019) Report from the American Society of Transplantation on frailty in solid organ transplantation. Am J Transplant 19(4):984–994. https://doi.org/10.1111/ajt.15198
Hook JL, Lederer DJ (2012) Selecting lung transplant candidates: where do current guidelines fall short? Expert Rev Respir Med 6(1):51. https://doi.org/10.1586/ers.11.83
Kelm DJ, Bonnes SL, Jensen MD et al (2016) Pre-transplant wasting (as measured by muscle index) is a novel prognostic indicator in lung transplantation. Clin Transplant 30(3):247–255. https://doi.org/10.1111/ctr.12683
Hsu J, Krishnan A, Lin CT et al (2019) Sarcopenia of the psoas muscles is associated with poor outcomes following lung transplantation. Ann Thorac Surg 107(4):1082–1088. https://doi.org/10.1016/j.athoracsur.2018.10.006
Gani F, Cerullo M, Amini N et al (2017) Frailty as a risk predictor of morbidity and mortality following liver surgery. J Gastrointest Surg 21(5):822–830. https://doi.org/10.1007/s11605-017-3373-6
Awano N, Inomata M, Kuse N et al (2020) Quantitative computed tomography measures of skeletal muscle mass in patients with idiopathic pulmonary fibrosis according to a multidisciplinary discussion diagnosis: a retrospective nationwide study in Japan. Respir Investig 58(2):91–101. https://doi.org/10.1016/j.resinv.2019.11.002
Pienta MJ, Zhang P, Derstine BA et al (2018) Analytic morphomics predict outcomes after lung transplantation. Ann Thorac Surg 105(2):399–405. https://doi.org/10.1016/j.athoracsur.2017.08.049
Sella N, Boscolo A, Lovison D et al (2022) The impact of nutritional status and sarcopenia on the outcomes of lung transplantation. J Heart Lung Transplant 41(4):S165. https://doi.org/10.1016/j.healun.2022.01.388
Kashani K, Sarvottam K, Pereira NL, Barreto EF, Kennedy CC (2018) The sarcopenia index: a novel measure of muscle mass in lung transplant candidates. Clin Transplant 32(3):e13182. https://doi.org/10.1111/ctr.13182
Singer JP, Diamond JM, Anderson MR et al (2018) Frailty phenotypes and mortality after lung transplantation: a prospective cohort study. Am J Transplant 18(8):1995–2004. https://doi.org/10.1111/ajt.14873
Hu A, Prosper A, Ruchaslski K et al (2021) Sarcopenia is distinct from physical frailty and significantly associated with length of stay after transplantation. J Heart Lung Transplant 40(4):S318–S319. https://doi.org/10.1016/j.healun.2021.01.902
Clausen ES, Frankel C, Palmer SM, Snyder LD, Smith PJ (2018) Pre-transplant weight loss and clinical outcomes after lung transplantation. J Heart Lung Transplant 37(12):1443–1447. https://doi.org/10.1016/j.healun.2018.07.015
Singer JP, Peterson ER, Golden J et al (2014) Lung Transplant body composition. J Heart Lung Transplant 33(4):S79. https://doi.org/10.1016/j.healun.2014.01.246
McClellan T, Allen BC, Kappus M et al (2017) Repeatability of computerized tomography-based anthropomorphic measurements of frailty in patients with pulmonary fibrosis undergoing lung transplantation. Curr Probl Diagn Radiol 46(4):300–304. https://doi.org/10.1067/j.cpradiol.2016.12.009
Tanimura K, Sato S, Fuseya Y et al (2016) Quantitative assessment of erector spinae muscles in patients with chronic obstructive pulmonary disease. Novel chest computed tomography–derived index for prognosis. Annals ATS 13(3):334–341. https://doi.org/10.1513/AnnalsATS.201507-446OC
Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J (2015) Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc 74(4):355–366. https://doi.org/10.1017/S0029665115000129
Oshima Y, Sato S, Chen-Yoshikawa TF et al (2022) Erector spinae muscle radiographic density is associated with survival after lung transplantation. J Thorac Cardiovasc Surg 164(1):300-311.e3. https://doi.org/10.1016/j.jtcvs.2021.07.039
Weig T, Milger K, Langhans B et al (2016) Core muscle size predicts postoperative outcome in lung transplant candidates. Ann Thorac Surg 101(4):1318–1325. https://doi.org/10.1016/j.athoracsur.2015.10.041
Rozenberg D, Wickerson L, Singer LG, Mathur S (2014) Sarcopenia in lung transplantation: a systematic review. J Heart Lung Transplant 33(12):1203–1212. https://doi.org/10.1016/j.healun.2014.06.003
Rozenberg D, Orsso CE, Chohan K et al (2020) Clinical outcomes associated with computed tomography-based body composition measures in lung transplantation: a systematic review. Transpl Int 33(12):1610–1625. https://doi.org/10.1111/tri.13749
Anderson MR, Easthausen I, Gallagher G et al (2020) Skeletal muscle adiposity and outcomes in candidates for lung transplantation: a lung transplant body composition cohort study. Thorax 75(9):801–804. https://doi.org/10.1136/thoraxjnl-2019-214461
Hu A, Prosper A, Ruchalski K et al (2023) Sarcopenia predicts outcomes after lung transplantation in older lung transplant candidates. Ann Thorac Surg Short Rep 1(1):174–178. https://doi.org/10.1016/j.atssr.2022.11.005
Derstine BA, Holcombe SA, Ross BE, Wang NC, Su GL, Wang SC (2018) Skeletal muscle cutoff values for sarcopenia diagnosis using T10 to L5 measurements in a healthy US population. Sci Rep 8(1):11369. https://doi.org/10.1038/s41598-018-29825-5
McNabb-Baltar J, Manickavasagan HR, Conwell DL et al (2022) A pilot study to assess opportunistic use of CT-scan for osteoporosis screening in chronic pancreatitis. Front Physiol 13:866945. https://doi.org/10.3389/fphys.2022.866945
Parulekar AD, Wang T, Li GW, Hoang V, Kao CC (2020) Pectoralis muscle area is associated with bone mineral density and lung function in lung transplant candidates. Osteoporos Int 31(7):1361–1367. https://doi.org/10.1007/s00198-020-05373-5
Grambsch PM, Therneau TM (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81(3):515–526. https://doi.org/10.1093/biomet/81.3.515
Alawi M, Begum A, Harraz M et al (2021) Dual-energy X-ray absorptiometry (DEXA) scan versus computed tomography for bone density assessment. Cureus 13(2):e13261. https://doi.org/10.7759/cureus.13261
Buckens CF, Dijkhuis G, de Keizer B, Verhaar HJ, de Jong PA (2015) Opportunistic screening for osteoporosis on routine computed tomography? An external validation study Eur Radiol 25(7):2074–2079. https://doi.org/10.1007/s00330-014-3584-0
Hendrickson NR, Pickhardt PJ, del Rio AM, Rosas HG, Anderson PA (2018) Bone mineral density T-scores derived from CT attenuation numbers (Hounsfield Units): clinical utility and correlation with dual-energy X-ray absorptiometry. Iowa Orthop J 38:25–31
Lee SY, Kwon SS, Kim HS et al (2015) Reliability and validity of lower extremity computed tomography as a screening tool for osteoporosis. Osteoporos Int 26(4):1387–1394. https://doi.org/10.1007/s00198-014-3013-x
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158(8):588–595. https://doi.org/10.7326/0003-4819-158-8-201304160-00003
Schreiber JJ, Anderson PA, Hsu WK (2014) Use of computed tomography for assessing bone mineral density. Neurosurg Focus 37(1):E4. https://doi.org/10.3171/2014.5.FOCUS1483
Zaidi Q, Danisa OA, Cheng W (2019) Measurement techniques and utility of Hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine 44(4):E239–E244. https://doi.org/10.1097/BRS.0000000000002813
Choi MK, Kim SM, Lim JK (2016) Diagnostic efficacy of Hounsfield units in spine CT for the assessment of real bone mineral density of degenerative spine: correlation study between T-scores determined by DEXA scan and Hounsfield units from CT. Acta Neurochir 158(7):1421–1427. https://doi.org/10.1007/s00701-016-2821-5
Gausden EB, Nwachukwu BU, Schreiber JJ, Lorich DG, Lane JM (2017) Opportunistic use of CT imaging for osteoporosis screening and bone density assessment: a qualitative systematic review. J Bone Joint Surg 99(18):1580–1590. https://doi.org/10.2106/JBJS.16.00749
Cho YH, Do KH, Chae EJ et al (2019) Association of chest CT-based quantitative measures of muscle and fat with post-lung transplant survival and morbidity: a single institutional retrospective cohort study in Korean population. Korean J Radiol 20(3):522–530. https://doi.org/10.3348/kjr.2018.0241
Nachit M, Horsmans Y, Summers RM, Leclercq IA, Pickhardt PJ (2023) AI-based CT body composition identifies myosteatosis as key mortality predictor in asymptomatic adults. Radiology. https://doi.org/10.1148/radiol.222008
Halpern AL, Boshier PR, White AM et al (2020) A comparison of frailty measures at listing to predict outcomes after lung transplantation. Ann Thorac Surg 109(1):233–240. https://doi.org/10.1016/j.athoracsur.2019.07.040
Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R (2006) Visceral fat is an independent predictor of all-cause mortality in men. Obesity 14(2):336–341. https://doi.org/10.1038/oby.2006.43
Ibrahim MM (2010) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev 11(1):11–18. https://doi.org/10.1111/j.1467-789X.2009.00623.x
Lee JH, Choi SH, Jung KJ, Goo JM, Yoon SH (2023) High visceral fat attenuation and long-term mortality in a health check-up population. J Cachexia Sarcopenia Muscle 14(3):1495–1507. https://doi.org/10.1002/jcsm.13226
Loor G, Brown R, Kelly RF et al (2017) Gender differences in long-term survival posttransplant: a single-institution analysis in the lung allocation score (LAS) era. Clin Transplant. https://doi.org/10.1111/ctr.12889
Roberts DH, Wain JC, Chang Y, Ginns LC (2004) Donor—recipient gender mismatch in lung transplantation: impact on obliterative bronchiolitis and survival. J Heart Lung Transplant 23(11):1252–1259. https://doi.org/10.1016/j.healun.2003.09.014
Suh JW, Paik HC, Yu WS et al (2019) Effect of sarcopenic overweight on lung transplant based in three-dimensional reconstructed psoas muscle mass. Ann Thorac Surg 107(6):1626–1631. https://doi.org/10.1016/j.athoracsur.2019.01.007
Nikkuni E, Hirama T, Hayasaka K et al (2021) Recovery of physical function in lung transplant recipients with sarcopenia. BMC Pulm Med 21(1):124. https://doi.org/10.1186/s12890-021-01442-5
Acknowledgements
We would like to acknowledge the Einstein Office of Medical Student Research for its support with this project.
Funding
The authors did not receive external support for this submitted work.
Author information
Authors and Affiliations
Contributions
RSF: study design, data collection, data analysis, writing of manuscript, reviewing of manuscript. AT: study design, data collection, reviewing of manuscript. VRJ: study design, data analysis, reviewing of manuscript. KY: data analysis, reviewing of manuscript. AM: study design, reviewing of manuscript. LBH: study design, data analysis, reviewing of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Friedman, R.S., Tarasova, A., Jain, V.R. et al. Predictive Value of CT Biomarkers in Lung Transplantation Survival: Preliminary Investigation in a Diverse, Underserved, Urban Population. Lung 201, 581–590 (2023). https://doi.org/10.1007/s00408-023-00650-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-023-00650-6