Abstract
Background
After pulmonary vein isolation (PVI) for atrial fibrillation (AF), it is common as an endpoint to demonstrate an exit block from the pulmonary veins (PVs) in addition to an entrance block into them. By using high-resolution mapping catheters, even very small signals can be detected.
Objectives
We investigated whether additional exit block testing is still necessary when using high-resolution mapping catheters after ablation in high-power short-duration (HPSD) techniques.
Materials and methods
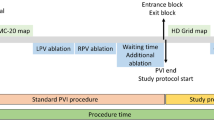
Overall, 114 patients with AF (average age, 65.14 ± 11.3 years; 65.8% male) undergoing radiofrequency PVI were included in the study. Ablation was performed with the HPSD technique using a fixed protocol for energy delivery of 50 W (contact force 3–20 g). Entrance and exit block were tested with a high-resolution mapping catheter. Isolation of the PVs was achieved in all patients.
Results
Capture of local PV tissue was demonstrated in all patients after PVI and exit block was present in all patients after entrance block was detected using a high-resolution mapping catheter.
Conclusion
Exit block testing in addition to the demonstration of an entrance block as an endpoint of PVI seems to have no additional benefit and might no longer be necessary when a high-resolution mapping catheter is used in HPSD ablation for PVI of AF.
Zusammenfassung
Hintergrund
Nach einer Pulmonalvenenisolation (PVI) bei Vorhofflimmern (AF) ist es als Endpunkt üblich, zusätzlich zum Nachweis eines Entrance-Blocks der Erregungsleitung in die Pulmonalvenen (PV) auch einen Exit-Block aus den PV nachzuweisen. Durch den Einsatz hochauflösender Mapping-Katheter können selbst sehr kleine Signale sicher detektiert werden.
Ziel der Arbeit
Es wurde untersucht, ob die zusätzliche Exit-Block-Testung beim Einsatz hochauflösender Mapping-Katheter nach Ablation in High-Power-Short-Duration (HPSD)-Technik noch notwendig ist.
Material und Methoden
Dazu wurden 114 Patienten mit Vorhofflimmern (Durchschnittsalter 65,14 ± 11,3 Jahre; 65,8 % männlich), bei denen eine Hochfrequenz-PVI durchgeführt wurde, in die Studie eingeschlossen. Die Ablation erfolgte in HPSD-Technik unter Verwendung eines festen Protokolls mit Energieabgaben von 50 W (Kontaktkraft 3–20 g). Entrance- und Exit-Block wurden mit einem hochauflösenden Mapping-Katheter getestet. Bei allen Patienten konnten die PV erfolgreich isoliert werden.
Ergebnisse
Durch Stimulation konnte lokales PV-Gewebe bei allen Probanden nach PVI erregt werden, und ein Exit-Block war bei allen Patienten vorhanden, nachdem ein Entrance-Block mittels hochauflösendem Mapping-Katheter nachgewiesen worden war.
Schlussfolgerung
Die Prüfung des Exit-Blocks zusätzlich zum Nachweis eines Entrance-Blocks als Endpunkt einer PVI scheint keinen zusätzlichen Nutzen zu haben und ist möglicherweise nicht mehr erforderlich, wenn ein hochauflösender Mapping-Katheter bei der HPSD-Ablation zur PVI von Vorhofflimmern eingesetzt wird.



Similar content being viewed by others
References
Jaïs P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, Hocini M, Extramiana F, Sacher F, Bordachar P, Klein G, Weerasooriya R, Clémenty J, Haïssaguerre M (2008) Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation 118(24):2498–2505. https://doi.org/10.1161/CIRCULATIONAHA.108.772582
Haïssaguerre M, Jaïs P, Shah DC, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Métayer P, Clémenty J (1998) Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med 339(10):659–666. https://doi.org/10.1056/NEJM199809033391003
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan G‑A, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau J‑P, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, van Gelder IC, van Putte BP, Watkins CL (2021) 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J 42(5):373–498. https://doi.org/10.1093/eurheartj/ehaa612
Sun X, Lu J, Lin J, Feng T, Suo N, Zheng L, Liu Z, Chen G, Fan X, Zhang S, Niu G (2021) Efficiency, safety, and efficacy of high-power short-duration radiofrequency ablation in patients with atrial fibrillation. Cardiol Res Pract 2021:8821467. https://doi.org/10.1155/2021/8821467
Calkins H, Hindricks G, Cappato R, Kim Y‑H, Saad EB, Aguinaga L, Akar JG, Badhwar V, Brugada J, Camm J, Chen P‑S, Chen S‑A, Chung MK, Cosedis Nielsen J, Curtis AB, Davies DW, Day JD, d’Avila A, de Groot NMS, Di Biase L, Duytschaever M, Edgerton JR, Ellenbogen KA, Ellinor PT, Ernst S, Fenelon G, Gerstenfeld EP, Haines DE, Haissaguerre M, Helm RH, Hylek E, Jackman WM, Jalife J, Kalman JM, Kautzner J, Kottkamp H, Kuck KH, Kumagai K, Lee R, Lewalter T, Lindsay BD, Macle L, Mansour M, Marchlinski FE, Michaud GF, Nakagawa H, Natale A, Nattel S, Okumura K, Packer D, Pokushalov E, Reynolds MR, Sanders P, Scanavacca M, Schilling R, Tondo C, Tsao H‑M, Verma A, Wilber DJ, Yamane T (2018) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace 20(1):e1–e160. https://doi.org/10.1093/europace/eux274
Gerstenfeld EP, Dixit S, Callans D, Rho R, Rajawat Y, Zado E, Marchlinski FE (2002) Utility of exit block for identifying electrical isolation of the pulmonary veins. J Cardiovasc Electrophysiol 13(10):971–979. https://doi.org/10.1046/j.1540-8167.2002.00971.x
Chen S, Meng W, Sheng He D, Chen G, Zhang F, Yan Y, Zhu-Ge Y, Liu S (2012) Blocking the pulmonary vein to left atrium conduction in addition to the entrance block enhances clinical efficacy in atrial fibrillation ablation. Pacing Clin Electrophysiol 35(5):524–531. https://doi.org/10.1111/j.1540-8159.2012.03343.x
Kléber AG, Rudy Y (2004) Basic mechanisms of cardiac impulse propagation and associated arrhythmias. Physiol Rev 84(2):431–488. https://doi.org/10.1152/physrev.00025.2003
Wynn G, Gupta D, Maille B, Snowdon R, Waktare J, Todd D, Hall M, Mahida S, Modi S (2018) Demonstration of pulmonary vein exit block following pulmonary vein isolation: a novel use for adenosine. J Cardiovasc Electrophysiol 29(11):1493–1499. https://doi.org/10.1111/jce.13744
Squara F, Liuba I, Chik W, Santangeli P, Zado ES, Callans DJ, Marchlinski FE (2015) Loss of local capture of the pulmonary vein myocardium after antral isolation: prevalence and clinical significance. J Cardiovasc Electrophysiol 26(3):242–250. https://doi.org/10.1111/jce.12585
Mochizuki A, Nagahara D, Kamiyama N, Fujito T, Miura T (2020) Revaluation of the significance of demonstrable exit block after radiofrequency pulmonary vein isolation. Circ Rep 2(4):218–225. https://doi.org/10.1253/circrep.CR-19-0135
Vijayaraman P, Dandamudi G, Naperkowski A, Oren J, Storm R, Ellenbogen KA (2012) Assessment of exit block following pulmonary vein isolation: far-field capture masquerading as entrance without exit block. Heart Rhythm 9(10):1653–1659. https://doi.org/10.1016/j.hrthm.2012.06.004
Pratola C, Baldo E, Notarstefano P, Toselli T, Ferrari R (2008) Radiofrequency ablation of atrial fibrillation: Is the persistence of all intraprocedural targets necessary for long-term maintenance of sinus rhythm? Circulation 117(2):136–143. https://doi.org/10.1161/CIRCULATIONAHA.106.678789
Duytschaever M, de Meyer G, Acena M, El-Haddad M, de Greef Y, van Heuverswyn F, Vandekerckhove Y, Tavernier R, Lee G, Kistler P (2013) Lessons from dissociated pulmonary vein potentials: entry block implies exit block. Europace 15(6):805–812. https://doi.org/10.1093/europace/eus353
Kim JY, Kim S‑H, Song IG, Kim YR, Kim T‑S, Kim J‑H, Jang S‑W, Lee MY, Rho T‑H, Oh Y‑S (2016) Achievement of successful pulmonary vein isolation: methods of adenosine testing and incremental benefit of exit block. J Interv Card Electrophysiol 46(3):315–324. https://doi.org/10.1007/s10840-016-0122-9
Papageorgiou N, Karim N, Williams J, Garcia J, Creta A, Ang R, Srinivasan N, Providencia R, Hunter RJ, Dhinoja M, Ezzat V, Sawhney V, Dennis A, Lowe M, Lambiase PD, Chow AWC (2021) Initial experience of the high-density grid catheter in patients undergoing catheter ablation for atrial fibrillation. J Interv Card Electrophysiol. https://doi.org/10.1007/s10840-021-00950-y
Andronache M, Drca N, Viola G (2019) High-resolution mapping in patients with persistent AF. Arrhythm Electrophysiol Rev 8(2):111–115. https://doi.org/10.15420/aer.2018.57.1
Anter E, Tschabrunn CM, Josephson ME (2015) High-resolution mapping of scar-related atrial arrhythmias using smaller electrodes with closer interelectrode spacing. Circ Arrhythm Electrophysiol 8(3):537–545. https://doi.org/10.1161/CIRCEP.114.002737
Bun S‑S, Delassi T, Latcu DG, El Jamili M, Ayari A, Errahmouni A, Berte B, Saoudi N (2018) A comparison between multipolar mapping and conventional mapping of atrial tachycardias in the context of atrial fibrillation ablation. Arch Cardiovasc Dis 111(1):33–40. https://doi.org/10.1016/j.acvd.2017.04.005
Seitz J, Bars C, Théodore G, Beurtheret S, Lellouche N, Bremondy M, Ferracci A, Faure J, Penaranda G, Yamazaki M, Avula UMR, Curel L, Siame S, Berenfeld O, Pisapia A, Kalifa J (2017) AF ablation guided by spatiotemporal electrogram dispersion without pulmonary vein isolation: a wholly patient-tailored approach. J Am Coll Cardiol 69(3):303–321. https://doi.org/10.1016/j.jacc.2016.10.065
Li M‑F, Wu J, Jin C‑L, Chen C‑F, Xu Y‑Z (2021) Safety and efficacy of high power shorter duration ablation for atrial fibrillation: a systematic review and meta-analysis. Int J Clin Pract 75(4):e13732. https://doi.org/10.1111/ijcp.13732
Andrade JG, Nattel S, Macle L (2015) Pulmonary vein exit block despite recovery of entry conduction during redo-ablation for atrial fibrillation. Europace 17(5):752. https://doi.org/10.1093/europace/euv033
Yagishita A, Gimbel JR, Arruda M (2016) Rate-dependent exit conduction block from pulmonary vein to left atrium after entrance block: new implications of pacing rate to confirm bidirectional conduction block. Circ Arrhythm Electrophysiol 9(6):e3871. https://doi.org/10.1161/CIRCEP.115.003871
Ouyang F, Antz M, Ernst S, Hachiya H, Mavrakis H, Deger FT, Schaumann A, Chun J, Falk P, Hennig D, Liu X, Bänsch D, Kuck K‑H (2005) Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double lasso technique. Circulation 111(2):127–135. https://doi.org/10.1161/01.CIR.0000151289.73085.36
de Greef Y, Tavernier R, Vandekerckhove Y, Duytschaever M (2010) Triggering pulmonary veins: a paradoxical predictor for atrial fibrillation recurrence after PV isolation. J Cardiovasc Electrophysiol 21(4):381–388. https://doi.org/10.1111/j.1540-8167.2009.01646.x
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Weyand, M. Beuter, D. Heinzmann and P. Seizer declare that they have no competing interests.
Ethical approval was waived by the ethics committee of the Landesärztekammer Baden-Württemberg in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Additional information

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Weyand, S., Beuter, M., Heinzmann, D. et al. High-resolution mapping as an alternative for exit block testing in the presence of entrance block after high-power short-duration pulmonary vein isolation. Herzschr Elektrophys 33, 440–445 (2022). https://doi.org/10.1007/s00399-022-00895-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00399-022-00895-3
Keywords
- Atrial fibrillation
- Catheter ablation
- Electrophysiologic study
- Radiofrequency ablation
- Ablation endpoint