Abstract
Purpose
The available evidence regarding the role of fruit and vegetable consumption in the development of colorectal polyps remains inconclusive, and there is a lack of data on different histopathologic features of polyps. We aimed to evaluate the associations of fruit and vegetable consumption with the prevalence of colorectal polyps and its subtypes in a high-risk population in China.
Methods
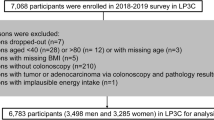
We included 6783 Chinese participants aged 40–80 years who were at high risk of colorectal cancer (CRC) in the Lanxi Pre-colorectal Cancer Cohort (LP3C). Dietary information was obtained through a validated food-frequency questionnaire (FFQ), and colonoscopy screening was used to detect colorectal polyps. Dose–response associations of fruit and vegetable intake with the prevalence of polyps were calculated using multivariate-adjusted regression models, which was reported as odds ratios (ORs) with 95% confidence intervals (CIs).
Results
2064 cases of colorectal polyps were ascertained in the LP3C during 2018–2019. Upon multivariable adjustments, including the diet quality, fruit consumption was inversely associated with the prevalence of polyps (P trend = 0.02). Participants in the highest tertile of fruit intake had a 25% lower risk (OR: 0.75; 95% CI 0.62‒0.92) compared to non-consumers, while vegetable consumption had no significant association with polyp prevalence (P trend = 0.86). In terms of colorectal histopathology and multiplicity, higher fruit intake was correlated with 24, 23, and 33% lower prevalence of small polyps (OR: 0.76; 95% CI 0.62‒0.94; P trend = 0.05), single polyp (OR: 0.77; 95% CI 0.62‒0.96; P trend = 0.04), and distal colon polyps (OR: 0.67; 95% CI 0.51‒0.87; P trend = 0.003), respectively.
Conclusions
Fresh fruit is suggested as a protective factor to prevent colorectal polyps in individuals at high risk of CRC, and should be underscored in dietary recommendations, particularly for high-risk populations.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the last author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CRC:
-
Colorectal cancer
- FFQ:
-
Food frequency questionnaire
- HCA:
-
Heterocyclic amine
- LP3C:
-
Lanxi Pre-colorectal Cancer Cohort
- MET-h/wk:
-
Metabolic equivalent task hours per week
- OR:
-
Odds ratio
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Fl B (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
Yang Y, Han Z, Li X, Huang A, Shi J, Gu J (2020) Epidemiology and risk factors of colorectal cancer in China. Chin J Cancer Res 32:729–741. https://doi.org/10.21147/j.issn.1000-9604.2020.06.06
Chen R, Zheng RS, Zhang SW, Zeng HM, Wang SM, Sun KX, Gu XY, Wei WW, He J (2019) Analysis of incidence and mortality of esophageal cancer in China, 2015. Zhongha Yu Fang Yi Xue Za Zhi 53:1094–1097. https://doi.org/10.3760/cma.j.issn.0253-9624.2019.11.004
Miller V, Yusuf S, Chow CK, Dehghan M, Corsi DJ, Lock K, Popkin B, Rangarajan S, Khatib R, Lear SA, Mony P, Kaur M, Mohan V, Vijayakumar K, Gupta R, Kruger A, Tsolekile L, Mohammadifard N, Rahman O, Rosengren A, Avezum A, Orlandini A, Ismail N, Lopez-Jaramillo P, Yusufali A, Karsidag K, Iqbal R, Chifamba J, Oakley SM, Ariffin F, Zatonska K, Poirier P, Wei L, Jian B, Hui C, Xu L, Xiulin B, Teo K, Mente A (2016) Availability, affordability, and consumption of fruits and vegetables in 18 countries across income levels: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet Glob Health 4:e695–e703. https://doi.org/10.1016/S2214-109X(16)30186-3
Hidaka A, Harrison TA, Cao Y, Sakoda LC, Barfield R, Giannakis M, Song M, Phipps AI, Figueiredo JC, Zaidi SH, Oland AE, Amitay EL, Berndt SI, Borozan I, Chan AT, Gallinger S, Gunter MJ, Guinter MA, Harlid S, Hampel H, Jenkins MA, Lin Y, Moreno V, Newcomb PA, Nishihara R, Ogino S, Obón-Santacana M, Parfrey PS, Potter JD, Slattery ML, Steinfelder RS, Um CY, Wang X, Woods MO, van Guelpen B, Thibodeau SN, Hoffmeister M, Sun W, Hsu L, Buchanan DD, Campbell PT, Peters U (2020) Intake of dietary fruit, vegetables, and fiber and risk of colorectal cancer according to molecular subtypes: a pooled analysis of 9 studies. Cancer Res 80:4578–4590. https://doi.org/10.1158/0008-5472.CAN-20-0168
Kunzmann AT, Coleman HG, Huang W-Y, Cantwell MM, Kitahara CM, Berndt SI (2016) Fruit and vegetable intakes and risk of colorectal cancer and incident and recurrent adenomas in the PLCO cancer screening trial. Int J Cancer 138:1851–1861. https://doi.org/10.1002/ijc.29922
Supachai K, Siripongpreeda B, Soonklang K, O-Pad N, Krohkaew K, Suebwongdit C, Panaiem S (2020) Association between low fruit and vegetable consumption and colorectal polyps in Thailand. Asian Pac J Cancer Prev 21:2733–2737. https://doi.org/10.31557/APJCP.2020.21.9.2733
Smith-Warner SA, Elmer PJ, Fosdick L, Randall B, Bostick RM, Grandits G, Grambsch P, Louis TA, Wood JR, Potter JD (2002) Fruits, vegetables, and adenomatous polyps: the Minnesota Cancer Prevention Research Unit case–control study. Am J Epidemiol 155:1104–1113. https://doi.org/10.1093/aje/155.12.1104
Ben Q, Zhong J, Liu J, Wang L, Sun Y, Yv L, Yuan Y (2015) Association between consumption of fruits and vegetables and risk of colorectal adenoma: a PRISMA-Compliant meta-analysis of observational studies. Medicine (Baltimore) 94:e1599. https://doi.org/10.1097/MD.0000000000001599
Colorectal Oncology Committee of Chinese Medical Doctor Association (2020) Chinese expert consensus on multidisciplinary treatment of bone metastasis from colorectal cancer (2020 version). Zhonghua Zhong Liu Za Zhi 42:433–437. https://doi.org/10.3760/cma.j.cn112152-20200402-00295
Wu F, Wang B, Zhuang P, Lu Z, Li Y, Wang H, Liu X, Zhao X, Yang W, Jiao J, Zheng W, Zhang Y (2021) Association of preserved vegetable consumption and prevalence of colorectal polyps: results from the Lanxi Pre-colorectal Cancer Cohort (LP3C). Euro J Nutr. https://doi.org/10.1007/s00394-021-02719-5
Yu C, Shi Z, Lv J, Du H, Qi L, Guo Y, Bian Z, Chang L, Tang X, Jiang Q, Mu H, Pan D, Chen J, Chen Z, Li L (2015) Major dietary patterns in relation to general and central obesity among Chinese adults. Nutrients 7:5834–5849. https://doi.org/10.3390/nu7075253
Peking University Medical Press (2019) China food composition 2018
Ma H, Li X, Zhou T, Sun D, Liang Z, Li Y, Heianza Y, Qi L (2020) Glucosamine use, inflammation, and genetic susceptibility, and incidence of type 2 diabetes: a prospective study in UK Biobank. Diabetes Care 43:719–725. https://doi.org/10.2337/dc19-1836
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR, Tudor-Locke C, Greer JL, Vezina J, Whitt-Glover MC, Leon AS (2011) 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 43:1575–1581. https://doi.org/10.1249/MSS.0b013e31821ece12
Wang K, Li Y, Liu G, Rimm E, Chan AT, Giovannucci EL, Song M (2020) Healthy lifestyle for prevention of premature death among users and nonusers of common preventive medications: a prospective study in 2 US cohorts. J Am Heart Assoc 9:e016692. https://doi.org/10.1161/JAHA.119.016692
Parker J, Gupta S, Torkington J, Dolwani S (2023) Comparison of recommendations for surveillance of advanced colorectal polyps: a systematic review of guidelines. J Gastroenterol 38:854–864. https://doi.org/10.1111/jgh.16157
He X, Wu K, Ogino S, Giovannucci EL, Chan AT, Song M (2018) Association between risk factors for colorectal cancer and risk of serrated polyps and conventional adenomas. Gastroenterology 155:355-373.e18. https://doi.org/10.1053/j.gastro.2018.04.019
Willett WC (2021) Chapter 5: Food frequency methods; Chapter 6: Reproducibility and validity of food-frequency questionnaires; Chapter 11: Implications of total energy intake for epidemiologic analyses. Nutritional Epidemiology, 3rd edn. Oxford, England: Oxford University Press; 2012
Wu H, Dai Q, Shrubsole MJ, Ness RM, Schlundt D, Smalley WE, Chen H, Li M, Shyr Y, Zheng W (2009) Fruit and vegetable intakes are associated with lower risk of colorectal adenomas. J Nutr 139:340–344. https://doi.org/10.3945/jn.108.098889
Millen AE, Subar AF, Graubard BI, Peters U, Hayes RB, Weissfeld JL, Yokochi LA, Ziegler RG (2007) Fruit and vegetable intake and prevalence of colorectal adenoma in a cancer screening trial. Am J Clin Nutr 86:1754–1764. https://doi.org/10.1093/ajcn/86.5.1754
Annema N, Heyworth JS, McNaughton SA, Iacopetta B, Fritschi L (2011) Fruit and vegetable consumption and the risk of proximal colon, distal colon, and rectal cancers in a case–control study in Western Australia. J Am Diet Assoc 111:1479–1490. https://doi.org/10.1016/j.jada.2011.07.008
Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Laure Preterre A, Iqbal K, Bechthold A, de Henauw S, Michels N, Devleesschauwer B, Boeing H, Schlesinger S (2018) Food groups and risk of colorectal cancer. Int J Cancer 142:1748–1758. https://doi.org/10.1002/ijc.31198
Kunzmann AT, Coleman HG, Huang W-Y, Kitahara CM, Cantwell MM, Berndt SI (2015) Dietary fiber intake and risk of colorectal cancer and incident and recurrent adenoma in the prostate, lung, colorectal, and ovarian cancer screening trial. Am J Clin Nutr 102:881–890. https://doi.org/10.3945/ajcn.115.113282
Ambalam P, Raman M, Purama RK, Doble M (2016) Probiotics, prebiotics and colorectal cancer prevention. Best Pract Res Clin Gastroenterol 30:119–131. https://doi.org/10.1016/j.bpg.2016.02.009
Feng Q, Liang S, Jia H, Stadlmayr A, Tang L, Lan Z, Zhang D, Xia H, Xu X, Jie Z, Su L, Li X, Li X, Li J, Xiao L, Huber-Schönauer U, Niederseer D, Xu X, Al-Aama JY, Yang H, Wang J, Kristiansen K, Arumugam M, Tilg H, Datz C, Wang J (2015) Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat Commun 6:6528. https://doi.org/10.1038/ncomms7528
Fragoso MF, Romualdo GR, Vanderveer LA, Franco-Barraza J, Cukierman E, Clapper ML, Carvalho RF, Barbisan LF (2018) Lyophilized açaí pulp (Euterpe oleracea Mart) attenuates colitis-associated colon carcinogenesis while its main anthocyanin has the potential to affect the motility of colon cancer cells. Food Chem Toxicol 121:237–245. https://doi.org/10.1016/j.fct.2018.08.078
Lim S, Xu J, Kim J, Chen T-Y, Su X, Standard J, Carey E, Griffin J, Herndon B, Katz B, Tomich J, Wang W (2013) Role of anthocyanin-enriched purple-fleshed sweet potato p40 in colorectal cancer prevention. Mol Nutr Food Res 57:1908–1917. https://doi.org/10.1002/mnfr.201300040
Brown EM, Latimer C, Allsopp P, Ternan NG, McMullan G, McDougall GJ, Stewart D, Crozier A, Rowland I, Gill CIR (2014) In vitro and in vivo models of colorectal cancer: antigenotoxic activity of berries. J Agric Food Chem 62:3852–3866. https://doi.org/10.1021/jf4050759
Hosseini F, Majdi M, Naghshi S, Sheikhhossein F, Djafarian K, Shab-Bidar S (2021) Nitrate-nitrite exposure through drinking water and diet and risk of colorectal cancer: a systematic review and meta-analysis of observational studies. Clin Nutr 40:3073–3081. https://doi.org/10.1016/j.clnu.2020.11.010
Liu Y, Li S, Jiang L, Zhang Y, Li Z, Shi J (2021) Solanaceous vegetables and colorectal cancer risk: a hospital-based matched case–control study in Northeast China. Front Nutr 8:688897. https://doi.org/10.3389/fnut.2021.688897
Mariadason JM, Catto-Smith A, Gibson PR (1999) Modulation of distal colonic epithelial barrier function by dietary fibre in normal rats. Gut 44:394–399. https://doi.org/10.1136/gut.44.3.394
Voorrips LE, Goldbohm RA, van Poppel G, Sturmans F, Hermus RJ, van den Brandt PA (2000) Vegetable and fruit consumption and risks of colon and rectal cancer in a prospective cohort study: The Netherlands cohort study on diet and cancer. Am J Epidemiol 152:1081–1092. https://doi.org/10.1093/aje/152.11.1081
Sakai H, Tabata S, Kimura M, Yabe S, Isa Y, Kai Y, Sato F, Yumoto T, Miyano K, Narita M, Uezono Y (2017) Active ingredients of hange-shashin-to, baicalelin and 6-gingerol, inhibit 5-fluorouracil-induced upregulation of CXCL1 in the colon to attenuate diarrhea development. Biol Pharm Bull 40:2134–2139. https://doi.org/10.1248/bpb.b17-00479
Windey K, de Preter V, Verbeke K (2012) Relevance of protein fermentation to gut health. Mol Nutr Food Res 56:184–196. https://doi.org/10.1002/mnfr.201100542
Acknowledgements
We thank grants from Lanxi Municipal Government, all participants and staff of the Lanxi Pre-colorectal Cancer Cohort for their contributions and Lanxi Red Cross Hospital for support of project development.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study investigation. Writing – Original Draft Preparation, Y.W.; Conceptualization, P.Z., J.J., W.Z., and Y.Z.; Methodology, S.W., Y.W., X.H., and F.W.; Validation, S.W., Y.W., J.Z., F.P., X.L., Y.L., Y.A., and P.Z.; Formal Analysis, S.W. and F.W.; Investigation, Y.W.; Resources, S.W.; Data Curation, F.W. and P.Z.; Writing – Review & Editing, P.Z., J.J., and Y.Z.; Visualization, Y.W.; Supervision, Y.Z.; Project Administration, W.Z. and Y.Z. All authors read and approved the manuscript. The work reported in the paper has been performed by the authors, unless clearly specified in the text.
Corresponding authors
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Ethical approval
The original protocol was approved by the ethical committee of Lanxi Red Cross Hospital, China. The ethical approval number is 20180302.
Consent to participate and publish
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, S., Wu, Y., Hu, X. et al. Fruit but not vegetable consumption is beneficial for low prevalence of colorectal polyps in a high-risk population: findings from a Chinese Lanxi Pre-colorectal Cancer Cohort study. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03377-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03377-z