Abstract
Purpose
The aim of this study was to develop and validate a model to predict 90-day mortality after acute colorectal cancer surgery.
Methods
The model was developed in all patients undergoing acute colorectal cancer surgery in 2014–2016 and validated in a patient group operated in 2017 in Denmark. The outcome was 90-day mortality. Tested predictor variables were age, sex, performance status, BMI, smoking, alcohol, education level, cohabitation status, tumour localization and primary surgical procedure. Variables were selected according to the smallest Akaike information criterion. The model was shrunken by bootstrapping. Discrimination was evaluated with a receiver operated characteristic curve, calibration with a calibration slope and the accuracy with a Brier score.
Results
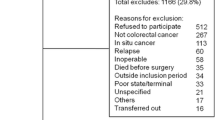
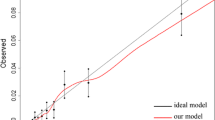
A total of 1450 patients were included for development of the model and 451 patients for validation. The 90-day mortality rate was 19% and 20%, respectively. Age, performance status, alcohol, smoking and primary surgical procedure were the final variables included in the model. Discrimination (AUC = 0.79), calibration (slope = 1.04, intercept = 0.04) and accuracy (brier score = 0.13) were good in the developed model. In the temporal validation, discrimination (AUC = 0.80) and accuracy (brier score = 0.13) were good, and calibration was acceptable (slope = 1.19, intercept = 0.52).
Conclusion
We developed prediction model for 90-day mortality after acute colorectal cancer surgery that may be a promising tool for surgeons to identify patients at risk of postoperative mortality.



Similar content being viewed by others
Availability of data and material
Data is owed by the Danish registries and are unfortunately not possible to share. However, data could be accessed through the different registries.
Code availability
not applicable.
References
Vos T, Abajobir AA, Abbafati C et al (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease study 2016. Lancet 390:1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F (2017) Global patterns and trends in colorectal cancer incidence and mortality. Gut 66:683–691. https://doi.org/10.1136/gutjnl-2015-310912
Oliphant R, Mansouri D, Nicholson GA, McMillan DC, Horgan PG, Morrison DS (2014) Emergency presentation of node-negative colorectal cancer treated with curative surgery is associated with poorer short and longer-term survival. Int J Color Dis 29:591–598. https://doi.org/10.1007/s00384-014-1847-5
Elliss-Brookes L, McPhail S, Ives A, Greenslade M, Shelton J, Hiom S, Richards M (2012) Routes to diagnosis for cancer - determining the patient journey using multiple routine data sets. Br J Cancer 107:1220–1226. https://doi.org/10.1038/bjc.2012.408
McPhail S, Elliss-Brookes L, Shelton J, Ives A, Greenslade M, Vernon S, Morris EJA, Richards M (2013) Emergency presentation of cancer and short-term mortality. Br J Cancer 109:2027–2034. https://doi.org/10.1038/bjc.2013.569
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91:605–609. https://doi.org/10.1002/bjs.4456
Amelung FJ, Consten ECJ, Siersema PD, Tanis PJ (2016) A population-based analysis of three treatment modalities for malignant obstruction of the proximal colon: acute resection versus stent or stoma as a bridge to surgery. Ann Surg Oncol 23:3660–3668. https://doi.org/10.1245/s10434-016-5247-7
Askari A, Malietzis G, Nachiappan S, Antoniou A, Jenkins J, Kennedy R, Faiz O (2015) Defining characteristics of patients with colorectal cancer requiring emergency surgery. Int J Color Dis 30:1329–1336. https://doi.org/10.1007/s00384-015-2313-8
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Color Dis 11:733–739. https://doi.org/10.1111/j.1463-1318.2008.01613.x
Degett TH, Dalton SO, Christensen J, Sogaard J, Iversen LH, Gogenur I (2019) Mortality after emergency treatment of colorectal cancer and associated risk factors -a nationwide cohort study. Int J Color Dis 34:85–95. https://doi.org/10.1007/s00384-018-3172-x
Annual report of Danish Colorectal Cancer Group (DCCG.dk) (2016) https://dccg.dk/wp-content/uploads/2017/10/Aarsrapport_2016.pdf. Accessed 7 February 2021
Huddart S, Peden CJ, Swart M, McCormick B, Dickinson M, Mohammed MA, Quiney N, Hemmings V, Riga A, Belguamkar A, Zuleika M, White D, Corrigan L, Howes T, Richards S, Dalton S, Cook T, Kryztopik R, Cornwell A, Goddard J, Grifiths S, Frost F, Pigott A, Pittman J, Cossey L, Smart N, Daniels I (2015) Use of a pathway quality improvement care bundle to reduce mortality after emergency laparotomy. Br J Surg 102:57–66. https://doi.org/10.1002/bjs.9658
Tengberg LT, Bay-Nielsen M, Bisgaard T, Cihoric M, Lauritsen ML, Foss NB (2017) Multidisciplinary perioperative protocol in patients undergoing acute high-risk abdominal surgery. Br J Surg 104:463–471. https://doi.org/10.1002/bjs.10427
Vester-Andersen M, Waldau T, Wetterslev J, Møller MH, Rosenberg J, Jørgensen LN, Jakobsen JC, Møller AM, InCare trial group, Gillesberg IE, Jakobsen HL, Hansen EG, Poulsen LM, Skovdal J, Søgaard EK, Bestle M, Vilandt J, Rosenberg I, Itenov TS, Pedersen J, Madsen MR, Maschmann C, Rasmussen M, Jessen C, Bugge L (2015) Randomized multicentre feasibility trial of intermediate care versus standard ward care after emergency abdominal surgery (InCare trial). Br J Surg 102:619–629. https://doi.org/10.1002/bjs.9749
Vester-Andersen M, Waldau T, Wetterslev J, Møller MH, Rosenberg J, Jørgensen LN, Gillesberg I, Jakobsen HL, Hansen EG, Poulsen LM, Skovdal J, Søgaard EK, Bestle M, Vilandt J, Rosenberg I, Berthelsen RE, Pedersen J, Madsen MR, Feurstein T, Busse MJ, Andersen JDH, Maschmann C, Rasmussen M, Jessen C, Bugge L, Ørding H, Møller AM (2013) Effect of intermediate care on mortality following emergency abdominal surgery. The InCare trial: study protocol, rationale and feasibility of a randomised multicentre trial. Trials 14:37. https://doi.org/10.1186/1745-6215-14-37
Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39:22–25. https://doi.org/10.1177/1403494810387965
Moons KG, Altman DG, Reitsma JB et al (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:W1–W73. https://doi.org/10.7326/m14-0698
Ingeholm P, Gogenur I, Iversen LH (2016) Danish Colorectal Cancer Group database. Clin Epidemiol 8:465–468. https://doi.org/10.2147/clep.s99481
Park IJ, Yu CS, Kim HC, Jung YH, Han KR, Kim JC (2006) Metachronous cancer. Color Dis 8:323–327. https://doi.org/10.1111/j.1463-1318.2006.00949.x
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish National Patient Register. Scand J Public Health 39:30–33. https://doi.org/10.1177/1403494811401482
Statistics Denmark (2021) https://www.dst.dk/en. Accessed 7 February 2021
Jensen VM, Rasmussen AW (2011) Danish Education Registers. Scand J Public Health 39:91–94. https://doi.org/10.1177/1403494810394715
Harrell FE Jr, Lee KL, Matchar DB, Reichert TA (1985) Regression models for prognostic prediction: advantages, problems, and suggested solutions. Cancer Treat Rep 69:1071–1077
Moons KG, Kengne AP, Woodward M et al (2012) Risk prediction models: I. Development, internal validation, and assessing the incremental value of a new (bio)marker. Heart 98:683–690. https://doi.org/10.1136/heartjnl-2011-301246
Steyerberg EW, Eijkemans MJ, Harrell FE Jr, Habbema JD (2000) Prognostic modelling with logistic regression analysis: a comparison of selection and estimation methods in small data sets. Stat Med 19:1059–1079. https://doi.org/10.1002/(sici)1097-0258(20000430)19:8<1059::aid-sim412>3.0.co;2-0
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, Pencina MJ, Kattan MW (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138. https://doi.org/10.1097/EDE.0b013e3181c30fb2
Royston P, Moons KG, Altman DG, Vergouwe Y (2009) Prognosis and prognostic research: developing a prognostic model. BMJ 338:b604. https://doi.org/10.1136/bmj.b604
Hanley JA, McNeil BJ (1982) The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–36. https://doi.org/10.1148/radiology.143.1.7063747
Danish Health Authority (2018) https://alkohologsamfund.dk/sites/alkohologsamfund.dk/files/media/document/Forebyggelsespakke Alkohol 2018.pdf. Accessed 7 February 2021
Richards CH, Leitch FE, Horgan PG, McMillan DC (2010) A systematic review of POSSUM and its related models as predictors of post-operative mortality and morbidity in patients undergoing surgery for colorectal cancer. J Gastrointest Surg 14:1511–1520. https://doi.org/10.1007/s11605-010-1333-5
Ozkan O, Guner A, Kaya U, Kece C, Reis E, Kesici S (2014) Evaluation of CR-POSSUM, original ACPGBI and new ACPGBI scoring systems for colorectal cancer surgery. Chirurgia (Bucur) 109:800–805
Richards CH, Leitch EF, Anderson JH, McKee RF, McMillan DC, Horgan PG (2011) The revised ACPGBI model is a simple and accurate predictor of operative mortality after potentially curative resection of colorectal cancer. Ann Surg Oncol 18:3680–3685. https://doi.org/10.1245/s10434-011-1805-1
Kumar P, Rodrigues GS (2009) Comparison of POSSUM and P-POSSUM for risk-adjusted audit of patients undergoing emergency laparotomy. Ulus Travma Acil Cerrahi Derg 15:19–22
Mohil RS, Bhatnagar D, Bahadur L, Rajneesh DDK, Magan M (2004) POSSUM and P-POSSUM for risk-adjusted audit of patients undergoing emergency laparotomy. Br J Surg 91:500–503. https://doi.org/10.1002/bjs.4465
D'Amico G, Malizia G, D'Amico M (2016) Prognosis research and risk of bias. Intern Emerg Med 11:251–260. https://doi.org/10.1007/s11739-016-1404-z
Thygesen LC, Ersboll AK (2014) When the entire population is the sample: strengths and limitations in register-based epidemiology. Eur J Epidemiol 29:551–558. https://doi.org/10.1007/s10654-013-9873-0
De Ceglie A, Filiberti R, Baron TH, Ceppi M, Conio M (2013) A meta-analysis of endoscopic stenting as bridge to surgery versus emergency surgery for left-sided colorectal cancer obstruction. Crit Rev Oncol Hematol 88:387–403. https://doi.org/10.1016/j.critrevonc.2013.06.006
Amelung FJ, de Beaufort HW, Siersema PD, Verheijen PM, Consten EC (2015) Emergency resection versus bridge to surgery with stenting in patients with acute right-sided colonic obstruction: a systematic review focusing on mortality and morbidity rates. Int J Color Dis 30:1147–1155. https://doi.org/10.1007/s00384-015-2216-8
Wolff RF, Moons KGM, Riley RD, Whiting PF, Westwood M, Collins GS, Reitsma JB, Kleijnen J, Mallett S, for the PROBAST Group† (2019) PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med 170:51–58. https://doi.org/10.7326/m18-1376
Funding
The Danish Cancer Society financed this study (grant no. 71237007).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation and analysis were performed by Thea Helene Degett, Jane Christensen, and Kirsten Frederiksen. The first draft of the manuscript was written by Thea Helene Degett, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
According to Danish regulation, register-based studies do not require ethical approval.
Consent to participate
According to Danish regulation, register based studies does not require individual consent from participants.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Degett, T.H., Christensen, J., Dalton, S.O. et al. Prediction of the postoperative 90-day mortality after acute colorectal cancer surgery: development and temporal validation of the ACORCA model. Int J Colorectal Dis 36, 1873–1883 (2021). https://doi.org/10.1007/s00384-021-03950-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03950-6