Abstract
Purpose
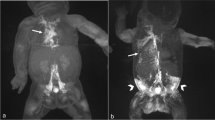
Central lymphatic obstructions are associated with anasarca and high mortality. We hypothesized that opening dilated cutaneous lymphatic channels by creating a lymphocutaneous fistula (LCF) would decompress the lymphatic circulation and improve anasarca.
Methods
We reviewed all patients that had at least one LCF created between 9/2019 and 12/2022. LCF efficacy was determined by changes in weight, urine/diuresis, ventilation, and clinical status.
Results
We created eleven LCFs in four infants. LCFs initially drained 108 cc/kg/d (IQR68–265 cc/kg/d). Weights significantly decreased after LCF creation (6.9 [IQR6.1–8.1] kg vs. 6.1 [IQR 4.9–7.6] kg, P = 0.042). Ventilatory support decreased significantly in all patients after at least one LCF was created, and 3/4 patients (75%) had significantly lower peak inspiratory pressures (28 [IQR 25–31] cmH2O vs. 22 [IQR 22–24] cmH2O, P = 0.005; 36 [IQR36–38] cmH2O vs. 33 [IQR 33–35] cmH2O, P = 0.002; 36 [IQR 34–47] cmH2O vs. 28 [28–31] cmH2O, P = 0.002). LCFs remained patent for 29d (IQR 16–49d). LCFs contracted over time, and 6/11 (54.5%) were eventually revised. There were no complications. Two patients died from overwhelming disease, one died from unrelated causes, and one remains alive 29 months after their initial LCF.
Conclusion
LCFs provide safe and effective temporary lymphatic decompression in patients with central lymphatic obstruction. While LCFs are not a cure, they can serve as a bridge to more definitive therapies or spontaneous lymphatic remodeling.
Level of evidence
IV.




Similar content being viewed by others
References
Liu M, Smith CL, Biko DM, Li D, Pinto E, O’Connor N, Skraban C, Zackai EH, Hakonarson H, Dori Y, Sheppard SE (2022) Genetics etiologies and genotype phenotype correlations in a cohort of individuals with central conducting lymphatic anomaly. Eur J Hum Genet 30:1022–1028
Mäkinen T, Boon LM, Vikkula M, Alitalo K (2021) Lymphatic malformations: genetics, mechanisms and therapeutic strategies. Circ Res 129:136–154
Dori Y (2016) Novel lymphatic imaging techniques. Tech Vasc Interv Radiol 19:255–261
Reisen B, Kovach SJ, Levin LS, Pinto E, Nadolski GJ, Itkin M, Dori Y, Laje P (2020) Thoracic duct-to-vein anastomosis for the management of thoracic duct outflow obstruction in newborns and infants: a CASE series. J Pediatr Surg 55:234–239
Biko DM, Johnstone JA, Dori Y, Victoria T, Oliver ER, Itkin M (2016) Recognition of neonatal lymphatic flow disorder: fetal mr findings and postnatal MR lymphangiogram correlation. Acad Radiol 25:1446–1450
Ramirez-Suarez KI, Tierradentro-Garcia LO, Smith CL, Krishnamurthy G, Escobar FA, Otero HJ, Rapp JB, Dori Y, Biko DM (2022) Dynamic contrast-enhanced magnetic resonance lymphangiography. Pediatr Radiol 52:285–294
Mejia EJ, Otero HJ, Smith CL, Shipman M, Liu M, Pinto E, DeWitt A, Rome JJ, Dori Y, Biko DM (2020) Use of contrast-enhanced ultrasound to determine thoracic duct patency. J Vasc Interv 31:1670–1674
Dori Y, Smith CL, DeWitt AG, Srinivasan A, Krishnamurthy G, Escobar FA, Biko DM (2020) Intramesenteric dynamic contrast pediatric MR lymphangiography: initial experience and comparison with intranodal and intrahepatic MR lymphangiography. Eur Radiol 30:5777–5784
Weissler JM, Cho EH, Koltz PF, Carney MJ, Itkin M, Laje P, Levin LS, Dori Y, Kanchwala SK, Kovach SJ (2018) Lymphovenous anastomosis for the treatment of chylothorax in infants: a novel microsurgical approach to a devastating problem. Plast Reconstr Surg 141:1502–1507
Pinto E, Dori Y, Smith C, DeWitt A, Williams C, Griffis H, Escobar F, Biko DM, Krishnamurthy G, Rome J, Glatz AC, Liu M, Ravishankar C, Zhang H, Taha D (2020) Neonatal lymphatic flow disorders: impact of lymphatic imaging and interventions on outcomes. J Perinatol 41:494–501
Dori Y, Itkin M (2016) Etiology and new treatment options for patients with plastic bronchitis. J Thorac Cardiovasc Surg 152:e49-50
Kylat RI, Witte MH, Barber BJ, Dori Y, Ghishan FK (2019) Resolution of protein-losing enteropathy after congenital heart disease repair by selective lymphatic embolization. Pediatr Gastroenterol Hepatol Nutr 22:594–600
Lippi G, Favaloro EJ, Cervellin G (2012) Hemostatic properties of the lymph: relationships with occlusion and thrombosis. Semin Thromb Hemost 38:213–221
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
PL and KM served as primary surgeons for all operations. CS, YD and GK were the primary interventionalists for all procedures and provided imaging analysis. PL, BS, EP and DL assisted with data collection and analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Laje, P., Smood, B., Smith, C. et al. Surgical creation of lymphocutaneous fistulas for the management of infants with central lymphatic obstruction. Pediatr Surg Int 39, 257 (2023). https://doi.org/10.1007/s00383-023-05532-9
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05532-9