Abstract
Background
The optimal management method for pediatric pancreatic trauma is controversial. Moreover, the efficacy of stent placement via endoscopic retrograde pancreatography (ERP) remains poorly documented.
Methods
The present, retrospective review of pediatric patients with pancreatic trauma was conducted from 2010 to 2020 at a single institution.
Results
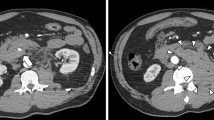
Ten, male children with the median age of 9.5 years (range 4–14 years) with a grade I (n = 2), II (n = 4) or III (n = 4) pancreatic injury were identified. Of six of these patients in whom ERP was performed, four had a pancreatic duct injury (PDI). Pancreatic stent placement was performed in all the patients with ERP at a site proximal to the injury in four patients and across the injury in two patients. A pseudocyst or pancreatic fluid collection was detected in five patients, of these, two with a grade II injury were managed successfully with conservative therapy while three with PDI required surgery. In the four patients with PDI, only one in whom the stent was placed across the PDI was able to avoid surgery.
Conclusion
Therapeutic ERP might be effective even if a patient has a PDI, therefore, early ERP should be considered as a treatment option.





Similar content being viewed by others
References
Englum BR, Gulack BC, Rice HE, Scarborough JE, Adibe OO (2016) Management of blunt pancreatic trauma in children: Review of the National Trauma Data Bank. J Pediatr Surg 51(9):1526–1531. https://doi.org/10.1016/j.jpedsurg.2016.05.003
Wood JH, Partrick DA, Bruny JL, Sauaia A, Moulton SL (2010) Operative vs nonoperative management of blunt pancreatic trauma in children. J Pediatr Surg 45(2):401–406. https://doi.org/10.1016/j.jpedsurg.2009.10.095
Kopljar M, Ivandić S, Mesić M, Bakota B, Žiger T, Kondža G, Pavić R, Milan M, Čoklo M (2020) Operative versus non-operative management of blunt pancreatic trauma in children: systematic review and meta-analysis. Injury. https://doi.org/10.1016/j.injury.2020.02.035
Garvey EM, Haakinson DJ, McOmber M, Notrica DM (2015) Role of ERCP in pediatric blunt abdominal trauma: a case series at a level one pediatric trauma center. J Pediatr Surg 50(2):335–338. https://doi.org/10.1016/j.jpedsurg.2014.08.017
Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, McAninch JW, Pachter HL, Shackford SR, Trafton PG (1990) Organ injury scaling, II: pancreas, duodenum, small bowel, colon, and rectum. J Trauma 30(11):1427–1429
Varadarajulu S, Noone TC, Tutuian R, Hawes RH, Cotton PB (2005) Predictors of outcome in pancreatic duct disruption managed by endoscopic transpapillary stent placement. Gastrointest Endosc 61(4):568–575. https://doi.org/10.1016/s0016-5107(04)02832-9
Canty TG Sr, Weinman D (2001) Management of major pancreatic duct injuries in children. J Trauma 50(6):1001–1007. https://doi.org/10.1097/00005373-200106000-00005
Kim HS, Lee DK, Kim IW, Baik SK, Kwon SO, Park JW, Cho NC, Rhoe BS (2001) The role of endoscopic retrograde pancreatography in the treatment of traumatic pancreatic duct injury. Gastrointest Endosc 54(1):49–55. https://doi.org/10.1067/mge.2001.115733
Rosenfeld EH, Vogel A, Russell RT, Maizlin I, Klinkner DB, Polites S, Gaines B, Leeper C, Anthony S, Waddell M et al (2018) Comparison of diagnostic imaging modalities for the evaluation of pancreatic duct injury in children: a multi-institutional analysis from the Pancreatic Trauma Study Group. Pediatr Surg Int 34(9):961–966. https://doi.org/10.1007/s00383-018-4309-2
Thomson DA, Krige JE, Thomson SR, Bornman PC (2014) The role of endoscopic retrograde pancreatography in pancreatic trauma: a critical appraisal of 48 patients treated at a tertiary institution. J Trauma Acute Care Surg 76(6):1362–1366. https://doi.org/10.1097/TA.0000000000000227
Houben CH, Ade-Ajayi N, Patel S, Kane P, Karani J, Devlin J, Harrison P, Davenport M (2007) Traumatic pancreatic duct injury in children: minimally invasive approach to management. J Pediatr Surg 42(4):629–635. https://doi.org/10.1016/j.jpedsurg.2006.12.025
Rescorla FJ, Plumley DA, Sherman S, Scherer LR 3rd, West KW, Grosfeld JL (1995) The efficacy of early ERCP in pediatric pancreatic trauma. J Pediatr Surg 30(2):336–340. https://doi.org/10.1016/0022-3468(95)90585-5
Mattix KD, Tataria M, Holmes J, Kristoffersen K, Brown R, Groner J et al (2007) Pediatric pancreatic trauma: predictors of nonoperative management failure and associated outcomes. J Pediatr Surg 42(2):340–344. https://doi.org/10.1016/j.jpedsurg.2006.10.006
Lin BC, Chen RJ, Fang JF, Hsu YP, Kao YC, Kao JL (2004) Management of blunt major pancreatic injury. J Trauma 56(4):774–778. https://doi.org/10.1097/01.ta.0000087644.90727.df
Lin BC, Wong YC, Chen RJ, Liu NJ, Wu CH, Hwang TL, Hsu YP (2017) Major pancreatic duct continuity is the crucial determinant in the management of blunt pancreatic injury: a pancreatographic classification. Surg Endosc 31(10):4201–4210. https://doi.org/10.1007/s00464-017-5478-0
Oláh A, Issekutz A, Haulik L, Makay R (2003) Pancreatic transection from blunt abdominal trauma: early versus delayed diagnosis and surgical management. Dig Surg 20(5):408–414. https://doi.org/10.1159/000072708
Kawahara I, Maeda K, Ono S, Kawashima H, Deie R, Yanagisawa S et al (2014) Surgical reconstruction and endoscopic pancreatic stent for traumatic pancreatic duct disruption. Pediatr Surg Int 30(9):951–956. https://doi.org/10.1007/s00383-014-3570-2
Wales PW, Shuckett B, Kim PC (2001) Long-term outcome after nonoperative management of complete traumatic pancreatic transection in children. J Pediatr Surg 36(5):823–827. https://doi.org/10.1053/jpsu.2001.22970
Acknowledgements
We thank Dr. Yuki Ogura, Dr. Hideyuki Horike and Dr. Yasuhiro Morita for providing clinical support. We also thank Dr. Minoru Kitago and Eisuke Iwasaki for important advice, and Mr. James R Valera for his assistance with editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional ethical committee (2020b-163) and was performed in accordance with the ethical standards of the 2000 Declaration of Helsinki. For this type of study, formal informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ishikawa, M., Shimojima, N., Koyama, T. et al. Efficacy of early endoscopic intervention in pediatric pancreatic duct injury management. Pediatr Surg Int 37, 1711–1718 (2021). https://doi.org/10.1007/s00383-021-05003-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-05003-z