Abstract
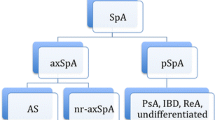
The categorization of axial spondyloarthritis (axSpA) into radiographic (r-axSpA) and non-radiographic (nr-axSpA) subtypes is important in clinical trials but may be of less value in clinical practice. This exploratory cross-sectional, multi-center study evaluated patients with axSpA under routine care at German clinical rheumatology sites (RHADAR real-world database), with a focus on imaging data used for diagnostic classifications. Our analyses included 371 patients with axSpA. The mean (standard deviation [SD]) age was 50.9 (14.0) years, disease duration was 16.4 (13.5) years, and 39.6% were female. Based on the rheumatologist’s final assessment, almost half of patients had definite r-axSpA (n = 179; 48.2%), 53 (14.3%) had suspected r-axSpA, 112 (30.2%) had non-radiographic-axSpA (nr-axSpA), and 27 (7.3%) had undefined axSpA. Patients assessed with definite or suspected r-axSpA were more likely to be treated with disease-modifying antirheumatic drugs (DMARDs) (62.0% and 64.2%, respectively) compared with nr-axSpA or undefined axSpA patients (37.5% and 48.1%, respectively). Almost all patients (348/371; 93.8%) had sacroiliac joint imaging data (radiographs or magnetic resonance imaging) documented in their charts, but only 216 (58.2%) had conventional radiographs required for formal diagnosis of r-axSpA by modified New York criteria. Follow-up radiographic imaging in nr-axSpA patients was uncommon (23/216 [25.0%]) but confirmed r-axSpA in 9/23 patients (39.1%). In conclusion, radiographs were available for slightly more than half of axSpA patients. Follow-up imaging was infrequent during rheumatology care in Germany but confirmed r-axSpA in ~ 40% of patients originally considered to have nr-axSpA. The distinction between r-axSpA and nr-axSpA may be ill-defined in routine clinical practice.

Similar content being viewed by others
Data availability
Data are available for collaborative research upon reasonable request.
References
Mease PJ, Liu M, Rebello S et al (2019) Comparative disease burden in patients with rheumatoid arthritis, psoriatic arthritis, or axial spondyloarthritis: data from two Corrona registries. Rheumatol Ther 6:529–542. https://doi.org/10.1007/s40744-019-00172-9
Krüger K, von Hinüber U, Meier F et al (2018) Ankylosing spondylitis causes high burden to patients and the healthcare system: results from a German claims database analysis. Rheumatol Int 38:2121–2131. https://doi.org/10.1007/s00296-018-4124-z
van der Heijde D, Ramiro S, Landewé R et al (2017) 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Ann Rheum Dis 76:978–991. https://doi.org/10.1136/annrheumdis-2016-210770
Michelena X, López-Medina C, Marzo-Ortega H (2020) Non-radiographic versus radiographic axSpA: what’s in a name? Rheumatology (Oxford) 59:iv18–iv24. https://doi.org/10.1093/rheumatology/keaa422
Ramiro S, Nikiphorou E, Sepriano A et al (2023) ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis 82:19–34. https://doi.org/10.1136/ard-2022-223296
López-Medina C, Ramiro S, van der Heijde D et al (2019) Characteristics and burden of disease in patients with radiographic and non-radiographic axial spondyloarthritis: a comparison by systematic literature review and meta-analysis. RMD Open 5:e001108. https://doi.org/10.1136/rmdopen-2019-001108
Protopopov M, Poddubnyy D (2018) Radiographic progression in non-radiographic axial spondyloarthritis. Expert Rev Clin Immunol 14:525–533. https://doi.org/10.1080/1744666x.2018.1477591
Poddubnyy D, Sieper J, Akar S et al (2022) Radiographic progression from non-radiographic to radiographic axial spondyloarthritis; results from a 5-year multicountry prospective observational study (abstract OP0149). Ann Rheum Dis 81(suppl 1):96. https://doi.org/10.1136/annrheumdis-2022-eular.2946
Mandl P, Navarro-Compán V, Terslev L et al (2015) EULAR recommendations for the use of imaging in the diagnosis and management of spondyloarthritis in clinical practice. Ann Rheum Dis 74:1327–1339. https://doi.org/10.1136/annrheumdis-2014-206971
Rudwaleit M, van der Heijde D, Landewé R et al (2009) The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68:777–783. https://doi.org/10.1136/ard.2009.108233
Lambert RGW, Bakker PAC, van der Heijde D et al (2016) Defining active sacroiliitis on MRI for classification of axial spondyloarthritis: update by the ASAS MRI working group. Ann Rheum Dis 75:1958–1963. https://doi.org/10.1136/annrheumdis-2015-208642
van der Linden S, Valkenburg HA, Cats A (1984) Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum 27:361–368. https://doi.org/10.1002/art.1780270401
Poddubnyy D, Diekhoff T, Baraliakos X et al (2022) Diagnostic evaluation of the sacroiliac joints for axial spondyloarthritis: should MRI replace radiography? Ann Rheum Dis 81:1486–1490. https://doi.org/10.1136/ard-2022-222986
Deodhar A, Reveille JD, van den Bosch F et al (2014) The concept of axial spondyloarthritis: joint statement of the Spondyloarthritis Research and Treatment Network and the Assessment of SpondyloArthritis international Society in response to the US Food and Drug Administration’s comments and concerns. Arthritis Rheumatol 66:2649–2656. https://doi.org/10.1002/art.38776
Walsh JA, Pei S, Penmetsa GK et al (2018) Cohort identification of axial spondyloarthritis in a large healthcare dataset: current and future methods. BMC Muculoskelet Disord 19:317. https://doi.org/10.1186/s12891-018-2211-7
Neurology and pain management coding alert: get a grip on new spondyloarthritis code set for 2022 (2021) https://www.aapc.com/codes/coding-newsletters/my-neurology-coding-alert/icd-10-2022-get-a-grip-on-new-spondyloarthritis-code-set-for-2022-170532-article. Accessed 7 Aug 2023
Zhao SS, Ermann J, Xu C et al (2019) Comparison of comorbidities and treatment between ankylosing spondylitis and non-radiographic axial spondyloarthritis in the United States. Rheumatology (Oxford) 58:2025–2030. https://doi.org/10.1093/rheumatology/kez171
Zhao SS, Hong C, Cai T et al (2020) Incorporating natural language processing to improve classification of axial spondyloarthritis using electronic health records. Rheumatology (Oxford) 59:1059–1065. https://doi.org/10.1093/rheumatology/kez375
Kiltz U, Braun J, Becker A et al (2019) Long version on the S3 guidelines for axial spondyloarthritis including Bechterew’s disease and early forms, update 2019: evidence-based guidelines of the German Society for Rheumatology (DGRh) and participating medical scientific specialist societies and other organizations. Z Rheumatol 78(suppl 1):3–64. https://doi.org/10.1007/s00393-019-0670-3
Ward MM, Deodhar A, Gensler LS et al (2019) 2019 update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Rheumatol 71:1599–1613. https://doi.org/10.1002/art.41042
Kleinert S, Bartz-Bazzanella P, von der Decken C, RHADAR Group (2021) A real-world rheumatology registry and research consortium: the German RheumaDatenRhePort (RHADAR) Registry. J Med Internet Res 23:e28164. https://doi.org/10.2196/28164
Kleinert S, Schuch F, Rapp P et al (2023) Impairment in cognitive function in patients with axial spondyloarthritis and psoriatic arthritis. Rheumatol Int 43:89–97. https://doi.org/10.1007/s00296-022-05248-4
Ethik-Kommission der Bayerischen Landesärztekammer. Application documents if the EK-BLÄK is a primary advisor according to §15 BO. https://ethikkommission.blaek.de/studien/sonstige-studien/antragsunterlagen-ek-primarberatend-15-bo. Accessed 14 Aug 2023.
National Ankylosing Spondylitis Society (2016) The Bath indices. https://nass.co.uk/wp-content/uploads/2018/09/Bath-Indices.pdf. Accessed 09 Aug 2023.
Zochling J (2011) Measures of symptoms and disease status in ankylosing spondylitis. Arthritis Care Res 63:S47-58. https://doi.org/10.1002/acr.20575
Ciurea A, Kissling S, Bürki K et al (2022) Current differentiation between radiographic and non-radiographic axial spondyloarthritis is of limited benefit for prediction of important clinical outcomes: data from a large, prospective, observational cohort. RMD Open 8:e002067. https://doi.org/10.1136/rmdopen-2021-002067
Poddubnyy D, Sieper J, Akar S et al (2022) Characteristics of patients with axial spondyloarthritis by geographic regions: PROOF multicountry observational study baseline results. Rheumatology (Oxford) 61:3299–3308. https://doi.org/10.1093/rheumatology/keab901
Hunter T, Sandoval D, Booth N, Holdsworth E, Deodhar A (2021) Comparing symptoms, treatment patterns, and quality of life of ankylosing spondylitis and non-radiographic axial spondyloarthritis patients in the USA: findings from a patient and rheumatologist survey. Clin Rheumatol 40:3161–3167. https://doi.org/10.1007/s10067-021-05642-6
Marques ML, Ramiro S, Van Lunteren M et al (2023) Can axial spondyloarthritis unequivocally be diagnosed by rheumatologists in patients with chronic back pain of less than two years duration? Main results of the SPondyloarthritis Caught Early (SPACE) cohort (abstract OP0005). Ann Rheum Dis 82(suppl 1):3–4. https://doi.org/10.1136/annrheumdis-2023-eular.2967
Diekhoff T, Eshed I, Radny F et al (2022) Choose wisely: imaging for the diagnosis of axial spondyloarthritis. Ann Rheum Dis 81:237–242. https://doi.org/10.1136/annrheumdis-2021-220136
Protopopov M, Proft F, Wichuk S et al (2023) Comparing MRI and conventional radiography for the detection of structural changes indicative of axial sponydloarthritis in the ASAS cohort. Rheumatology (Oxford) 62:1631–1635. https://doi.org/10.1093/rheumatology/keac432
Sepriano A, Ramiro S, van der Heijde D et al (2022) Imaging outcomes for axial spondyloarthritis and sensitivity to change: a five-year analysis of the DESIR cohort. Arthritis Care Res (Hoboken) 72:251–258. https://doi.org/10.1002/acr.24459
Kucybala I, Urbanik A, Wojciechowski W (2018) Radiologic approach to axial spondyloarthritis: where are we now and where are we heading? Rheumatol Int 38:1753–1762. https://doi.org/10.1007/s00296-018-4130-1
Acknowledgements
We thank the patients and medical staff who participated in this study. Data management services were provided by Nils Koerber and medical writing support was provided by Sharon L. Cross, PhD under the direction of the authors; both were funded by RHADAR GbR (A Network of Rheumatologists) with a grant from Novartis Pharma GmbH.
Funding
This study was funded by the RheumaDatenRhePort GbR (A Network of Rheumatologists), Bahnhofstr. 32, 82152 Planegg, Germany. RHADAR GbR received a grant for this study from Novartis Pharma GmbH.
Author information
Authors and Affiliations
Contributions
All authors met the ICMJE criteria for authorship, made contributions to conception and/or implementation of the study, were involved in reviewing and revising the manuscript, gave final approval to the version to be published, and take full responsibility for the integrity and accuracy of all aspects of this work.
Corresponding author
Ethics declarations
Conflict of interest
SK, PB-B, CVdD, KK, GG, SS-M, CK, WV, and MW are members of RheumaDatenRhePort. SK received grants or contracts from Abbvie, Novartis, and Sparrow for phase 2/3 clinical trials, received consulting fees or honoraria from Abbvie, Celgene, Galapagos, Novartis, and Siemens Healthineers, and participated on a data safety monitoring or advisory board for Abbvie. FS received consulting or speaker’s fees from Abbvie, Galapagos, Lilly, Novartis, and Rheumaakademie and travel or meeting support from Abbvie. MR received consulting or speaking fees from Abbvie, BMS, Galapagos, Janssen, Novartis, and UCB, travel or meeting support from Pfizer, and participated on data safety monitoring or advisory boards for Abbvie, Galapagos, Novartis, and UCB. JW received consulting fees from Abbvie. FP received consulting fees from Abbvie, Boehringer, Galapagos, Medac, and Viatris. PBB received speaking fees from AbbVie, Boehringer Ingelheim, Chugai/Roche, Janssen-Cilag, Novartis, Pfizer, and UCB, travel or meeting support from Abbvie, and participated on a data safety monitoring or advisory board for RHADAR GbR. KK received speaking fees from Abbvie, Galapagos, Novartis, Rheumakademie, and UCB, travel or meeting support from UCB, and participated on a data safety monitoring or advisory board for RHADAR GbR. GG received speaking fees from Abbvie, Galapagos, and Novartis and travel or meeting support from Abbvie and Novartis. PW received consulting or speaking fees from Abbvie, Galapagos, Jannsen, and Medac. SSM received speaking fees from AbbVie, Boehringer Ingelheim, GSK, Janssen-Cilag, Lilly, Novartis, and UCB and participated on a data safety monitoring or advisory board for RHADAR GbR. MW received grants or contracts from AbbVie, BMS, Boehringer, Galapagos, Gilead, GSK, Hexal, Janssen, Novartis, Pfizer, and UCB, consulting or speaking fees from Abbvie, Aescu, Alexion, Amgen, Biogen, BDI, BDRH, BMS, Boehringer, Celltrion, DGRH, Fresenius, Galapagos, Gilead, GSK, Hexal, Janssen, Medac, MSD, Mundipharma, Mylan, Novartis, Pfizer, RHADAR, RheCORD, Rheumaliga, Riemser, Roche, Sanofi-Aventis, SOBI, and UCB, travel or meeting support from Abbvie, Amgen, Celltrion, Galapagos, GSK, Novartis, Pfizer, Sanofi-Aventis, and UCB, and participated on a data safety monitoring or advisory board for Abbvie, Boehringer, Fresenius, Galapagos, Gilead, GSK, Janssen, Novartis, Pfizer, Sanofi-Aventis, and UCB. PR, PS, CvdD, CK, and WV do not have any competing interests to declare.
Ethical approval
The study was exempted from ethical approval under German law due to the use of anonymized data.
Informed consent
Written informed consent was obtained from all patients prior to study start.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kleinert, S., Schuch, F., Rapp, P. et al. Radiographic and non-radiographic axial spondyloarthritis are not routinely distinguished in everyday clinical care: an analysis of real-world data from rheumatology practices. Rheumatol Int 44, 653–661 (2024). https://doi.org/10.1007/s00296-023-05463-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05463-7