Abstract
Purpose
We aimed to investigate the potential of [68Ga]Ga-FAPI-04 PET/CT as an alternative diagnostic and theranostic tool in well-differentiated NETs refractory to [177Lu]Lu-DOTATATE therapy.
Methods
Patients who received at least two cycles of [177Lu]Lu-DOTATATE therapy for metastatic NETs and progressed under treatment were included. All patients had performed [68Ga]Ga-DOTATATE and [68Ga]Ga-FAPI-04 PET/CT within 3 weeks. The number of PET-positive lesions related to NETs and tumor sites was documented. Mann-Whitney U and chi-square tests were used to compare SUVmax levels of tracers and the number of detected metastases.
Results
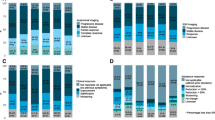
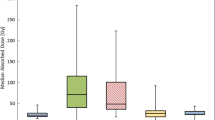
Twelve patients (7 male, 5 female) who met the eligibility criteria were included in the study. Ten patients had grade 1–2 NET of various origins, and two had paraganglioma and pheochromocytoma. One hundred ninety-eight of 230 lesions (86%) were SSTR positive with a median SUVmax of 16.6 (2.2–76.5), and 88 of 230 lesions (38.2%) were [68Ga]Ga-FAPI-04 positive with a median SUVmax of 5.1 (2.3–21). Median SUVmax level and detected number of tumors were significantly higher in [68Ga]Ga-DOTATATE PET/CT (p=<0.001). [68Ga]Ga-FAPI-04 PET/CT was completely (n:2) or almost completely (n:3) negative in 5 (42%) patients. Two (17%) patients had flip-flop SSTR/FAPI uptake in tumors. In four patients (33%), tumor uptake or the number of PET-positive lesions was inferior in [68Ga]Ga-FAPI-04 PET/CT. In only one patient (8%), tumor uptakes were higher in [68Ga]Ga-FAPI-04 PET/CT. Low-dose [177Lu]Lu-FAPI-46 dosimetry was performed on the FAPI-dominant patient; absorbed radiation doses per GBq were 1.26 Gy, 0.36 Gy, 0.32 Gy, and 0.2 Gy for kidneys, liver, spleen, and total body, respectively. The mean absorbed dose per GBq was 0.33 Gy for liver mass and 0.41 Gy for metastatic lymph nodes.
Conclusion
Our preliminary results demonstrated that [68Ga]Ga-FAPI-04 PET/CT mainly failed in well-differentiated NETs refractory to [177Lu]Lu-DOTATATE therapy and had a limited role as an alternative diagnostic or theranostic agent. Further investigations with a larger patient population are required to determine the impact of [68Ga]Ga-FAPI-04 PET/CT on NETs.




Similar content being viewed by others
References
Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing but NET: a review of neuroendocrine tumors and carcinomas. Neoplasia. 2017;19:991–1002.
Shah MH, Goldner WS, Benson AB, Bergsland E, Blaszkowsky LS, Brock P, et al. Neuroendocrine and adrenal tumors, version 2.2021, NCCN clinical practice guidelines in oncology. J Nat Compr Canc Netw. 2021;19:839–68.
Wolin EM. The expanding role of somatostatin analogs in the management of neuroendocrine tumors. Gastrointes Cancer Res: GCR. 2012;5:161.
Zappi A, Persano I, Galvani L, Parlagreco E, Andrini E, Campana D, et al. Chemotherapy in well differentiated neuroendocrine tumors (NET) G1, G2, and G3: a narrative review. J Clin Med. 2023;12:717.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of 177Lu-DOTATATE for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Zhang J, Song Q, Cai L, Xie Y, Chen Y. The efficacy of 177Lu-DOTATATE peptide receptor radionuclide therapy (PRRT) in patients with metastatic neuroendocrine tumours: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2020;146:1533–43.
Wang L-f, Lin L, Wang M-j, Li Y. The therapeutic efficacy of 177Lu-DOTATATE/DOTATOC in advanced neuroendocrine tumors: a meta-analysis. Medicine. 2020:99.
Sanli Y, Denizmen D, Subramaniam RM. Gastro-enteric-pancreatic neuroendocrine tumor treatment: 177Lu-DOTATATE. PET Clin. 2023;18:201–14.
Strosberg JR, Caplin ME, Kunz PL, Ruszniewski PB, Bodei L, Hendifar A, et al. 177Lu-DOTATATE plus long-acting octreotide versus high-dose long-acting octreotide in patients with midgut neuroendocrine tumours (NETTER-1): final overall survival and long-term safety results from an open-label, randomised, controlled, phase 3 trial. Lancet Oncol. 2021;22:1752–63.
Brabander T, Van der Zwan WA, Teunissen JJ, Kam BL, Feelders RA, de Herder WW, et al. Long-term efficacy, survival, and safety of [177Lu-DOTA0, Tyr3] octreotate in patients with gastroenteropancreatic and bronchial neuroendocrine tumors efficacy, survival, and toxicity after 177Lu-DOTATATE. Clin Cancer Res. 2017;23:4617–24.
Yordanova A, Mayer K, Brossart P, Gonzalez-Carmona MA, Strassburg CP, Essler M, et al. Safety of multiple repeated cycles of 177 Lu-octreotate in patients with recurrent neuroendocrine tumour. Eur J Nucl Med Mol Imaging. 2017;44:1207–14.
Ballal S, Yadav MP, Tripathi M, Sahoo RK, Bal C. Survival outcomes in metastatic gastroenteropancreatic neuroendocrine tumor patients receiving concomitant 225Ac-DOTATATE–targeted α-therapy and capecitabine: a real-world-scenario management-based long-term outcome study. J Nucl Med. 2023;64:211–8.
Chan HS, Konijnenberg MW, Daniels T, Nysus M, Makvandi M, de Blois E, et al. Improved safety and efficacy of 213Bi-DOTATATE-targeted alpha therapy of somatostatin receptor-expressing neuroendocrine tumors in mice pre-treated with L-lysine. EJNMMI Res. 2016;6:1–11.
Kratochwil C, Flechsig P, Lindner T, Abderrahim L, Altmann A, Mier W, et al. 68Ga-FAPI PET/CT: tracer uptake in 28 different kinds of cancer. J Nucl Med. 2019;60:801–5.
Kuyumcu S, Kovan B, Sanli Y, Buyukkaya F, Simsek DH, Özkan ZG, et al. Safety of fibroblast activation protein–targeted radionuclide therapy by a low-dose dosimetric approach using 177Lu-FAPI04. Clin Nucl Med. 2021;46:641–6.
Assadi M, Rekabpour SJ, Jafari E, Divband G, Nikkholgh B, Amini H, et al. Feasibility and therapeutic potential of 177Lu–fibroblast activation protein inhibitor–46 for patients with relapsed or refractory cancers: a preliminary study. Clin Nucl Med. 2021;46:e523–e30.
Baum RP, Schuchardt C, Singh A, Chantadisai M, Robiller FC, Zhang J, et al. Feasibility, biodistribution, and preliminary dosimetry in peptide-targeted radionuclide therapy of diverse adenocarcinomas using 177Lu-FAP-2286: first-in-humans results. J Nucl Med. 2022;63:415–23.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur. J. Cancer. 2009;45:228–47.
Kuyumcu S, Özkan ZG, Sanli Y, Yilmaz E, Mudun A, Adalet I, et al. Physiological and tumoral uptake of 68 Ga-DOTATATE: standardized uptake values and challenges in interpretation. Ann Nucl Med. 2013;27:538–45.
Shi X, Xing H, Yang X, Li F, Yao S, Zhang H, et al. Fibroblast imaging of hepatic carcinoma with 68 Ga-FAPI-04 PET/CT: a pilot study in patients with suspected hepatic nodules. Eur J Nucl Med Mol Imaging. 2021;48:196–203.
Kömek H, Gündogan C, Can C. 68Ga-FAPI PET/CT versus 68Ga-DOTATATE PET/CT in the evaluation of a patient with neuroendocrine tumor. Clin Nucl Med. 2021;46:e290–e2.
Cheng Z, Zou S, Cheng S, Song S, Zhu X. Comparison of 18F-FDG, 68Ga-FAPI, and 68Ga-DOTATATE PET/CT in a patient with pancreatic neuroendocrine tumor. Clin Nucl Med. 2021;46:764–5.
Wang H, Du Z, Huang Q, Ren S, Guan Y, Xie F, et al. The superiority of [68 Ga] Ga-FAPI-04 over [18 F]-FDG in a case of neuroendocrine tumour with hepatic metastasis. Eur J Nucl Med Mol Imaging. 2021;48:3005–6.
Kreppel B, Gonzalez-Carmona MA, Feldmann G, Küppers J, Moon ES, Marinova M, et al. Fibroblast activation protein inhibitor (FAPi) positive tumour fraction on PET/CT correlates with Ki-67 in liver metastases of neuroendocrine tumours. Nuklearmed-Nucl Med. 2021;60:344–54.
Ergül N, Yılmaz B, Cin M, Çermik TF. 68Ga-DOTA-FAPI-04 PET/CT in neuroendocrine carcinoma of the liver with elevated AFP level: comparison with: 18: F-FDG PET/CT. Clin Nucl Med. 2022;47:e29–31.
Li L, Hu X, Ma J, Yang S, Gong W, Zhang C. A systematic review of [68Ga] Ga-DOTA-FAPI-04 and [18F] FDG PET/CT in the diagnostic value of malignant tumor bone metastasis. Front Oncol. 2022;12:978506.
Tian R, Xie Q, Yu F, Du C, Yao X, Zang S, et al. Detection of bone metastases by 68 Ga-DOTA-SSAs and 18 F-FDG PET/CT: a two-center head-to-head study of gastroenteropancreatic neuroendocrine neoplasms. Contrast Media Mol Imaging. 2022;2022
Simsek DH, Kuyumcu S, Turkmen C, Sanlı Y, Aykan F, Unal S, et al. Can complementary 68Ga-DOTATATE and 18F-FDG PET/CT establish the missing link between histopathology and therapeutic approach in gastroenteropancreatic neuroendocrine tumors? J Nucl Med. 2014;55:1811–7.
Graham N, Qian B-Z. Mesenchymal stromal cells: emerging roles in bone metastasis. Int J Mol Sci. 2018;19:1121.
Guo W, Pang Y, Yao L, Zhao L, Fan C, Ke J, et al. Imaging fibroblast activation protein in liver cancer: a single-center post hoc retrospective analysis to compare [68 Ga] Ga-FAPI-04 PET/CT versus MRI and [18 F]-FDG PET/CT. Eur J Nucl Med Mol Imaging. 2021;48:1604–17.
Siripongsatian D, Promteangtrong C, Kunawudhi A, Kiatkittikul P, Boonkawin N, Chinnanthachai C, et al. Comparisons of quantitative parameters of Ga-68-labelled fibroblast activating protein inhibitor (FAPI) PET/CT and [18F] F-FDG PET/CT in patients with liver malignancies. Mol Imaging Biol. 2022;24:818–29.
Lindner T, Loktev A, Altmann A, Giesel F, Kratochwil C, Debus J, et al. Development of quinoline-based theranostic ligands for the targeting of fibroblast activation protein. J Nucl Med. 2018;59:1415–22.
Ballal S, Yadav MP, Kramer V, Moon ES, Roesch F, Tripathi M, et al. A theranostic approach of [68 Ga] Ga-DOTA. SA. FAPi PET/CT-guided [177 Lu] Lu-DOTA. SA. FAPi radionuclide therapy in an end-stage breast cancer patient: new frontier in targeted radionuclide therapy. Eur J Nucl Med Mol Imaging. 2021;48:942–4.
Ballal S, Yadav MP, Moon ES, Roesch F, Kumari S, Agarwal S, et al. Novel fibroblast activation protein inhibitor-based targeted theranostics for radioiodine-refractory differentiated thyroid cancer patients: a pilot study. Thyroid. 2022;32:65–77.
Ferdinandus J, Costa PF, Kessler L, Weber M, Hirmas N, Kostbade K, et al. Initial clinical experience with 90Y-FAPI-46 radioligand therapy for advanced-stage solid tumors: a case series of 9 patients. J Nucl Med. 2022;63:727–34.
Sidrak MMA, De Feo MS, Corica F, Gorica J, Conte M, Filippi L, et al. Fibroblast activation protein inhibitor (FAPI)-based theranostics—where we are at and where we are heading: a systematic review. Int J Mol Sci. 2023;24:3863.
Robbins ME, O’Malley Y, Zhao W, Davis CS, Bonsib SM. The role of the tubulointerstitium in radiation-induced renal fibrosis. Radiat Res. 2001;155:481–9.
Del Prete M, Buteau F-A, Arsenault F, Saighi N, Bouchard L-O, Beaulieu A, et al. Personalized 177 Lu-octreotate peptide receptor radionuclide therapy of neuroendocrine tumours: initial results from the P-PRRT trial. Eur J Nucl Med Mol Imaging. 2019;46:728–42.
Privé BM, Boussihmad MA, Timmermans B, van Gemert WA, Peters SM, Derks YH, et al. Fibroblast activation protein-targeted radionuclide therapy: background, opportunities, and challenges of first (pre) clinical studies. Eur J Nucl Med Mol Imaging. 2023;1-13
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This prospective study was approved by our institutional review board, and written informed consent was obtained from all patients.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Has Simsek, D., Guzel, Y., Denizmen, D. et al. The inferior performance of [68Ga]Ga-FAPI-04 PET/CT as a diagnostic and theranostic biomarker in [177Lu]Lu-DOTATATE refractory well-differentiated neuroendocrine tumors. Eur J Nucl Med Mol Imaging 51, 828–840 (2024). https://doi.org/10.1007/s00259-023-06497-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-023-06497-6